Medicare patients make up the majority of health systems’ revenue; yet, organizations earn only a one percent profit while caring for this population. Despite historically low profit margins, Medicare can be lucrative for health systems, and through the Medicare Shared Savings Program, healthcare organizations can increase revenue with four tools:
1. The ability to aggregate and analyze data.
2. The ability to align financial incentives between payers and providers.
3. The ability to engage patients in behavior or lifestyle modifications.
4. The ability to garner support from clinicians and encourage them to lead the shift to VBC.
As the shift from fee-for-service to value-based care continues, health systems can leverage MSSP to deliver the highest level of care while also increasing profit margins.

If business executives were asked, “Does it make sense to accept a negative two percent margin caring for the Medicare segment comprising the majority of your revenue?” most would say no, unless they were trading currency or selling screws. Yet health systems accept fee-for-service Medicare and Medicaid payment schedules that yield such meager margins.
Most healthcare executives would have two responses to working with these slim margins: it is part of their professional duty to care for these patients, and care is essentially mandated by the government. Now, with the emergence of new payment models, healthcare can add a third reason to care for Medicare and Medicaid patients—the potential for double-digit profits.
Historically, health systems have preferred to care for patients with private insurance because the reimbursement rates are higher. For example, in 2019, The New York Times reported that Medicare will pay a hospital $17,000 for a knee replacement, compared to the roughly $37,000 the hospital makes for that procedure for a patient with private insurance.
Although providing care to Medicare patients is unavoidable for most health systems—as is earning less than a 1 percent profit while caring for this population—Medicare can be lucrative through value-based programs such as the Medicare Shared Savings Program (MSSP) and the Bundled Payments Care Initiative. This article outlines how the shift to value-based programs helps healthcare organizations improve margins and take better care of patients and communities.
In an effort to shift the mindset from volume to value, CMS created the MSSP in 2012, a payment model that financially rewards providers and health systems for delivering value, practicing evidence-based medicine, and helping patients reach optimum health. The shift to value-based care (VBC) requires health systems to provide the highest quality care at the lowest price in order to financially succeed.
At the American Hospital Association Regional Policy board meeting in September 2019, CMS Administrator Seema Verma warned health systems that if they don’t transition to VBC fast enough, the government may get more involved—making it more difficult for hospitals to generate revenue. Recent revisions to the MSSP promoting a faster path to downside risk, coupled with significant hurdles to success in the Merit-based Incentive Payment System (MIPS) program, are driving health systems towards VBC.
Verma also spoke about the future of CMS and VBC: “Make no mistake—if your business model is focused merely on increasing volume rather than improving health outcomes, coordinating care and cutting waste, you will not succeed under the new paradigm.”
The MSSP is an opportunity for healthcare organizations to improve care and generate money in this new value-based model. By using broader amounts of data and improving data sources through four specific tools, the new VBC landscape allows health systems to increase their operating margins in a way they can’t under the fee-for-service (FFS) model.
To be successful in the new VBC landscape, health systems must utilize analytics tools for managing large amounts of data. Organizations coupling advanced data analytics capabilities with changes in physician compensation plans and care delivery models will succeed; those that fail to change and manage data well will go out of business.
So, how can health systems create a roadmap to success in the new VBC landscape? There are four tools that are absolutely key to success in this new healthcare climate and within the MSSP:
Why is data the differentiating factor in success and failure within VBC? Data analytics finds opportunities for cost savings and improved patient care. To achieve the best patient outcomes, health systems must mine data accurately at scale and in near real time (e.g., the ACO measure analysis, Figure 1). Traditional transactional systems such as EMRs and point solutions are inadequate to identify opportunities to drive success in the value-based world.
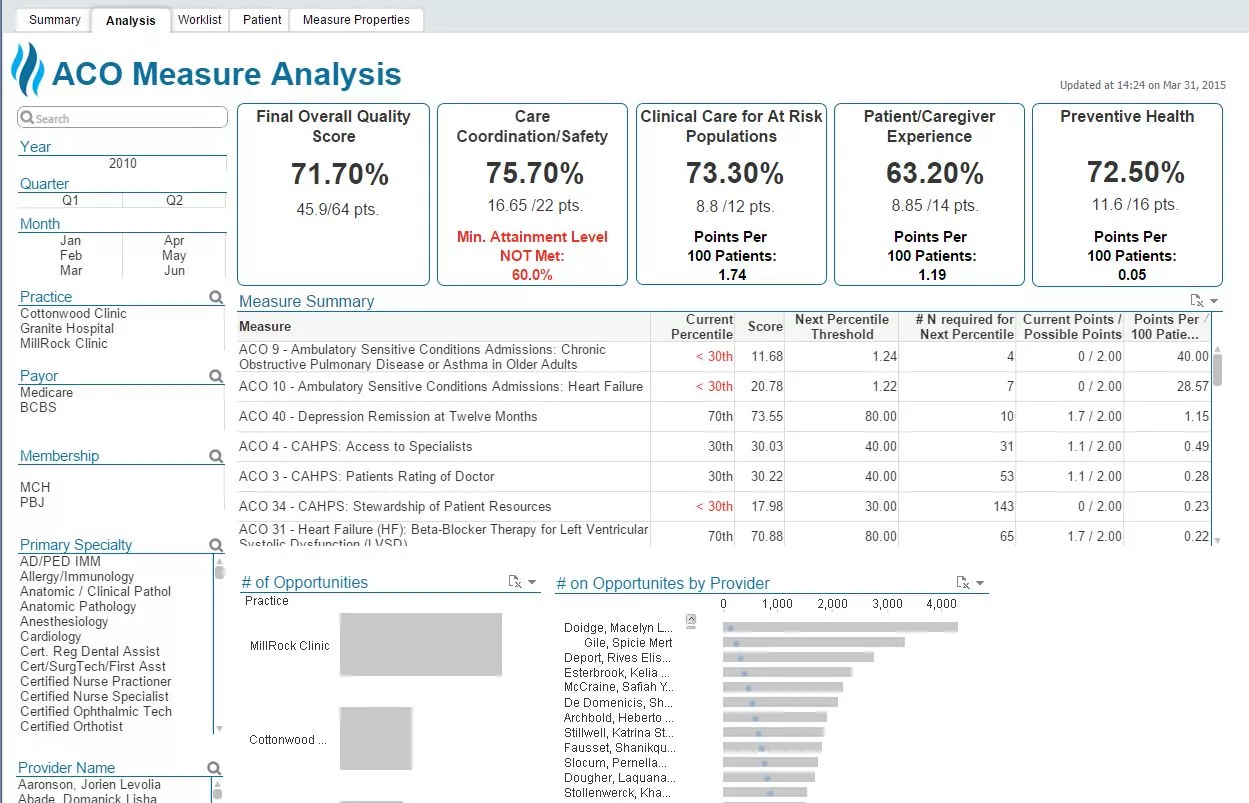
The retrospective collection and analysis of data allows for continuous improvements in care models. Data also drives predictive analytics tools designed to prevent bad outcomes and better-individualized patient care; because it allows for a type of “concierge customized care for the masses,” data can both standardize care and tailor it at the same time.
For example, specific Health Catalyst tools empower organizations to mine data effectively:
The MSSP methodology financially rewards providers who deliver high-quality, appropriate care at the lowest cost. In a nutshell, providers benefit financially by delivering high-quality, low-cost care regardless of the volume of care provided.
How do health systems effectively engage patients? One way is to partner with companies that keep patients accountable with constant reminders and specific guidance for managing lifestyle decisions. This is incredibly hard. Using data to prospectively identify patients in need of additional education or support is a critical component to any successful patient engagement program or tool. Second, enlisting the help of family members, friends, and community health workers in the care process is highly effective.
Clinicians must lead the change from FFS to VBC; however, getting clinicians on board is no easy task. In an era in which most clinicians associate data analytics with the EMR and outcomes metrics with clinically meaningless box checking, healthcare must educate its workforce about the real value of data analytics. When done well, data empowers clinicians to answer their own questions and ultimately provide better, more efficient care. Over time, clinicians learn to trust the analytics tools and drive a culture of data-driven decision making.
Once health systems have experience and success increasing revenue with the MSSP, they can apply these same tools and expertise to higher-risk programs, such as Medicare Advantage (MA), Medicaid, and commercial plans. The limited downside to the MSSP makes it an ideal training ground to master the capabilities needed to succeed in value-based programs. Second, the MSSP allows systems to increase margins in the Medicare population.
There is a much greater financial risk and reward for health systems when participating in MA—a program in which Medicare beneficiaries are managed by private insurance companies. In the past, health systems earning profits in MA have either been lucky or first learned how to succeed through programs such as the MSSP. Sometimes health systems who have received a bonus in the MA program can’t explain how they achieved it. When health systems apply the same tools and skills they develop through the MSSP to other areas of the organization and other programs (e.g., MA), they are more prepared to take on risk, resulting in higher margins and less waste.
One organization’s experience shows how health systems can make real gains through the MSSP. Mission Health, a health system in North Carolina, knew it could increase profits through the MSSP by taking a more data-informed approach. The health system formed one of the largest ACOs in the country, Mission Health Partners (MHP), ultimately caring for 90,000 Medicare patients.
After forming MHP, its leadership team created a comprehensive, strategic plan to garner better access to real-time data. With data driving the MSSP strategy, MHP discovered ways to transition the initial progress into long-term success (Figure 2), consistently identifying opportunities for outcomes improvement and improving the health of Medicare patients in western North Carolina.
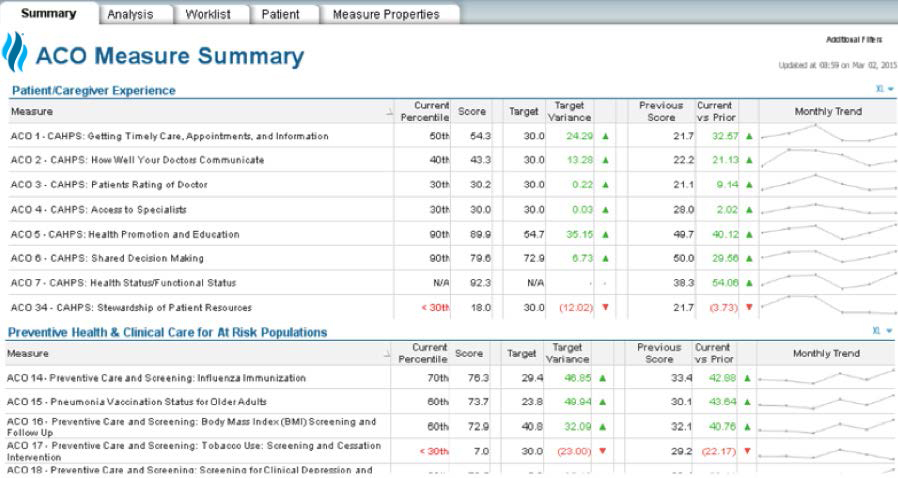
Mission Health’s MSSP success started with a roadmap that led to a clear goal—increase profits through the MSSP by improving VBC. All healthcare organizations must have a clear understanding of where they are today in the journey from FFS to VBC and where they want to be in 5, 10, and 15 years. Command of data informs the roadmap on how to get there.
It is important to financially understand the impact of moving 40 percent of overall revenue to a value-based product such as the MSSP. Assuming system revenues of $4 billion, $1 billion of that revenue is generated by Medicare patients (40 percent). Assuming a 1 percent margin in the Medicare FFS model, profits equal $10 million. If the same system participated in the MSSP and achieved quality goals in the 67th percentile while reducing the total cost of care by 4 percent, it would receive a cash payment of almost twice that realized in the FFS model (this is all assuming that the system understands its true costs of delivering care and really makes 1 percent Medicare margins).
Which organizations will survive the payment model shift? Data analytics is a foundational asset for any health system going forward. It is the direction that supports the roadmap to success in the new value-based paradigm.
With healthcare’s continued evolution away from FFS and toward VBC, including the new CMS programs like MSSP, a new day is dawning for health systems. To succeed in a time of rapid payer model change, health systems must have the ability to aggregate and analyze data, align financial incentives between payers and providers, engage patients in their own behavior changes, and garner support from clinicians as they strive to create a culture that delivers VBC.
Calculate the Financial Impact of Your MSSP.
Would you like to learn more about this topic? Here are some articles we suggest: