
More than $33M
in positive margin impact by expense reduction and more hospital in/outpatient revenue


Deliver healthcare data, analytics, and insights at the speed of change with our enterprise-grade platform.

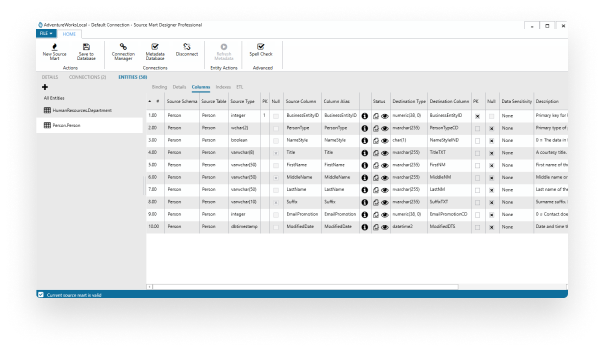
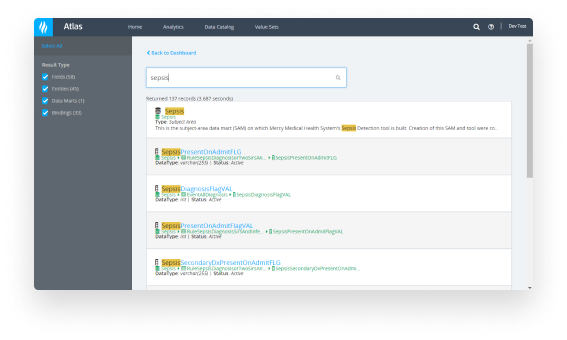

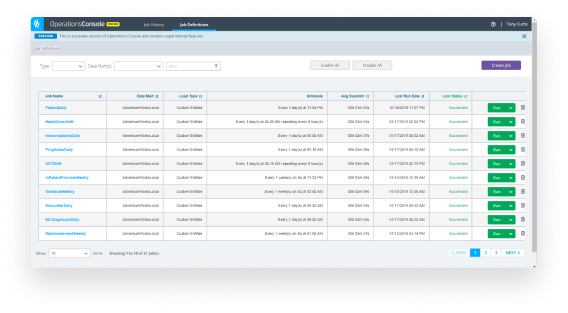

Extract, load, and transform enterprise-wide data into the Health Catalyst unified data model (including deduplication of patient records).
Build custom analytics and/or implement over 20 analytics accelerators aimed at targeted improvement opportunities for enterprise healthcare organizations.

in positive margin impact by expense reduction and more hospital in/outpatient revenue

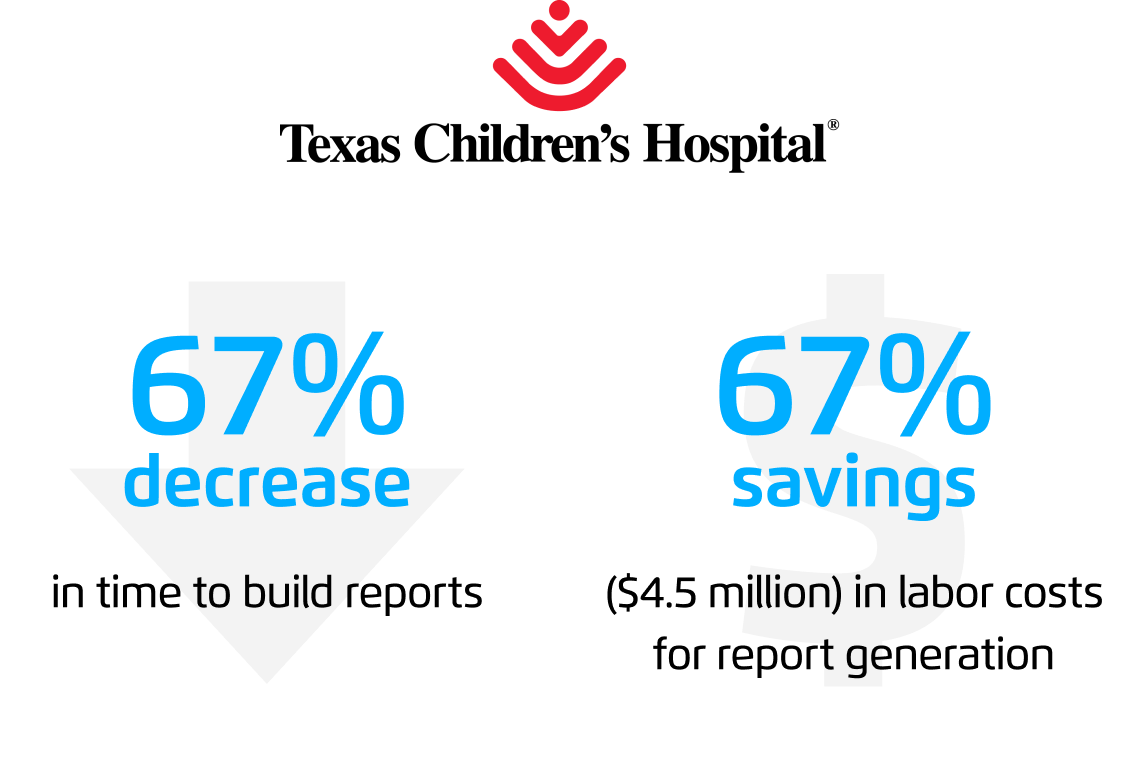
in analyst time, freeing up time for more meaningful improvement activities




This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.