Healthcare is confronting rising costs, aging and growing populations, an increasing focus on population health, alternative payment models, and other challenges as the industry shifts from volume to value. These obstacles drive a growing need for more digitization, accompanied by a data-centric improvement strategy.
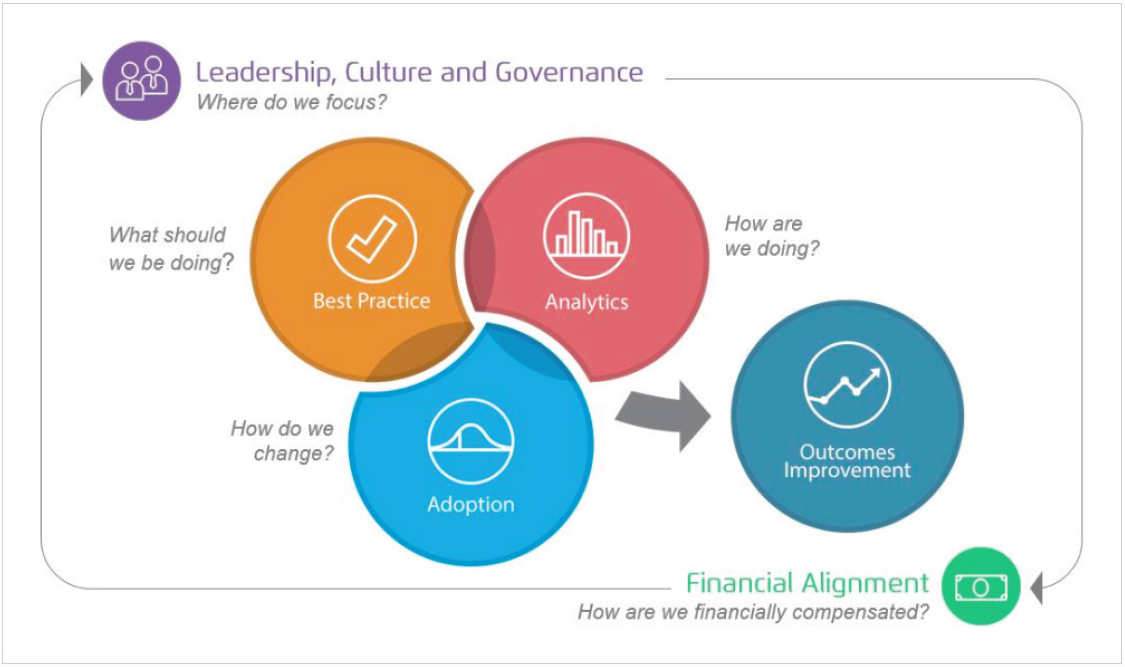
To establish and maintain data as a primary strategy that guides clinical, financial, and operational transformation, organizations must have three systems in place:
1. Best practices to identify target behaviors and practices.
2. Analytics to accelerate improvement and identify gaps between best practices and analytic results.
3. Adoption processes to outline the path to transformation.


Forward-thinking health systems are talking about both improvement strategies and the use of data to fundamentally transform healthcare while the industry confronts shared challenges. Obstacles include rising costs; aging and growing populations; the need for better access and outcomes at lower cost; changing demographics (including health status, economics, etc.); and an increasing focus on population health, alternative payment models, and other new models as the industry shifts from volume to value-based payment. To succeed in an increasingly digitized and data-driven industry, organizations must ensure that their data strategy is central to their overall improvement strategy, as opposed to two independent strategies.
Meeting current healthcare challenges requires an overall vision with a data strategy to support and sustain organizational goals—namely, a robust and comprehensive approach that leverages data at the center of the improvement and delivery strategy.
To leverage data as a strategic asset, organizations must make data a primary, not tangential, strategy. Three systems comprise the foundation of a data-first transformation strategy (Figure 1) that supports the fourth element, improvement:
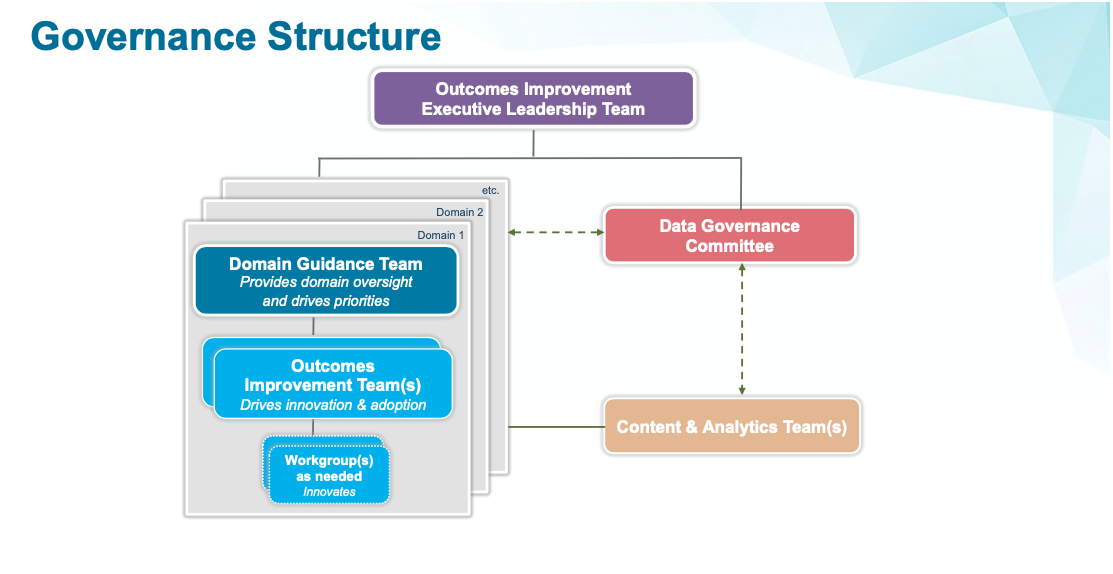
Organizations that have built successful and sustainable improvement strategies, with data and analytic strategies supporting them, have a few key characteristics.
First, they have built a structure to support sustainable improvement, with strong governance, clear priorities, and engaged clinicians with the required resources to support the efforts (Figure 2).
Second, successful health systems have aligned incentives to ensure focus and commitment around their organizational vision and strategies.
And, third, they have provided the technology and tools to manage expanding data and interoperability (e.g., a cloud-based analytics platform. such as the Health Catalyst® Data Operating System [DOS™]).
The right tools and technology, supported by the right structure, can successful improvement, such as the following:
The need for change is clear, as is the opportunity. As healthcare data skills, assets, and capabilities mature, health systems must use data strategically to transform care clinically, financially, and operationally. An evolving industry will require and drive the need for broader and richer patient data, compelling organizations to move forward with a clear data and analytics strategy. Successful health systems will acquire the needed data (e.g., data beyond the clinical care setting), integrate it into operations, supply an interoperable data platform, and create an agile governance structure to manage the data and support a culture around data use. Furthermore, to truly transform healthcare, that data strategy has to be embedded in an overall improvement strategy and vision.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/V4K6BDPkhjDNF