The journey for healthcare organizations to become data driven is complex but absolutely critical for success in today’s increasingly digitized environment. Data literacy is an essential capability because it empowers team members at every level of the organization—from individual learners to executives—to aggregate, analyze, and utilize data to drive decision making.
To optimize data usage and reach high levels of data literacy, health systems can create a data literacy program based on four foundational elements:
1. Infrastructure
2. Access
3. Support
4. Privacy and Security
According to an article published by Dalhousie University, data literacy is the ability to collect, manage, evaluate, and apply data in a critical manner. Data literacy empowers users to comprehend healthcare data and then use it to make clinical and business decisions with confidence, viewing the provision of care through a broader lens that includes data insight and analytics talent.
The journey to prioritize data and become a data-driven healthcare organization starts at the top. Leadership must drive the change, emphasize the importance of data literacy at every level, and understand that the journey to becoming data-driven is an ever-evolving state based on the analytic tools and talent available. The evolution of other data tools (such as AI, ML, predictive modeling, etc.) will also impact the data literacy program needs.
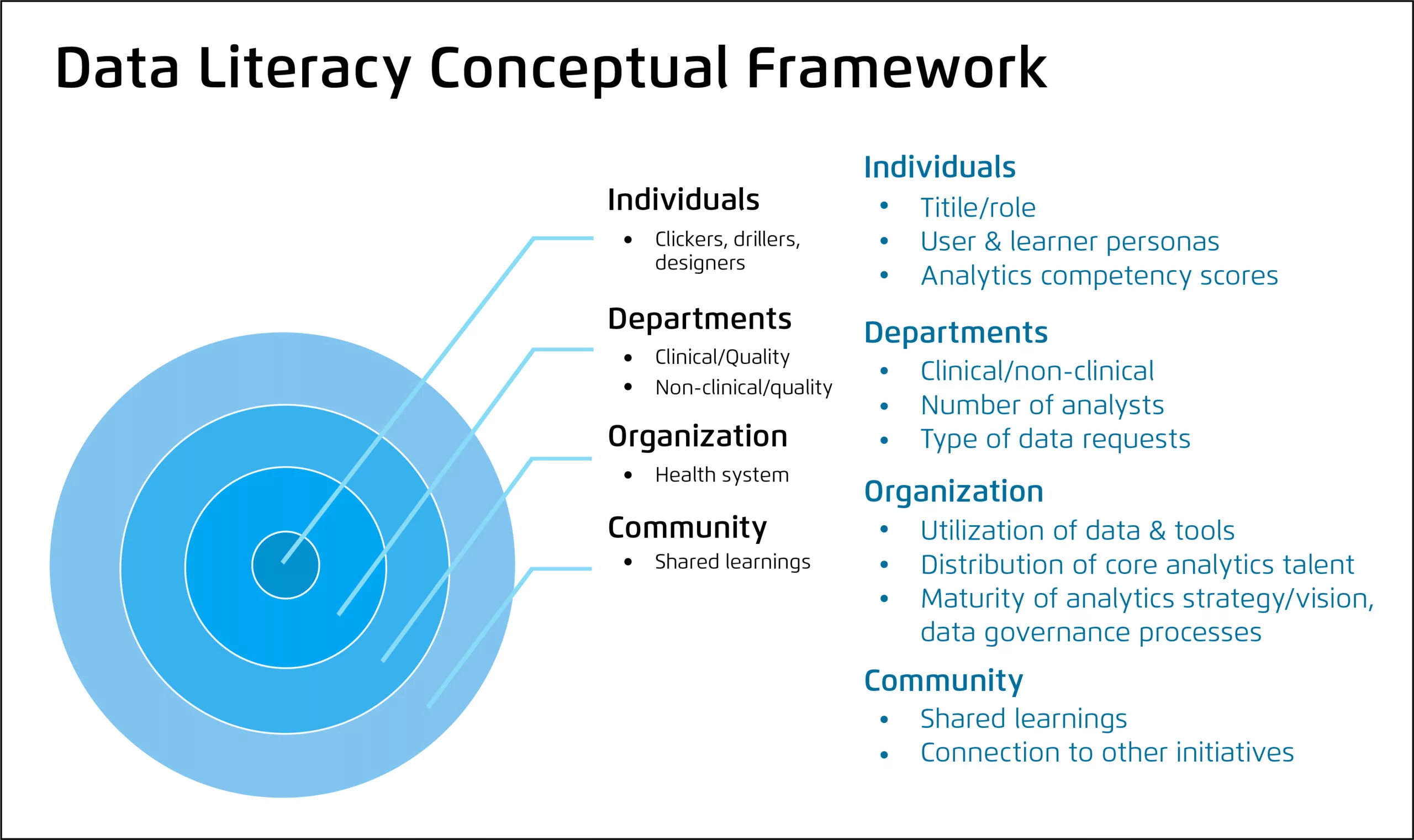
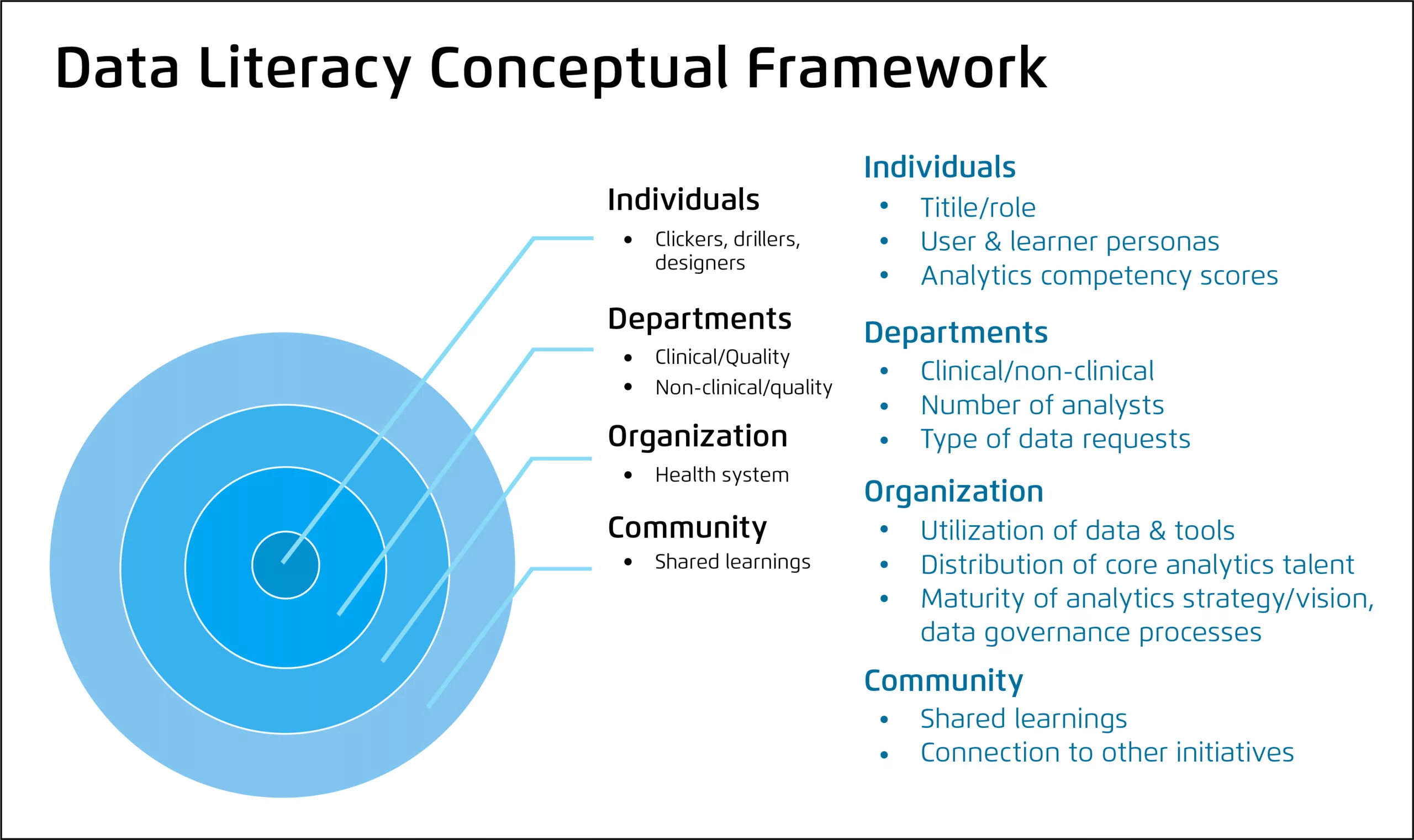
Once the leadership team has committed to prioritizing data, investing in data, and becoming a data-informed organization, the data literacy assessment is the next step. Health systems can best promote healthcare data literacy by first compartmentalizing the learning needs at different levels of the organization, as described in the data literacy conceptual framework (Figure 1):
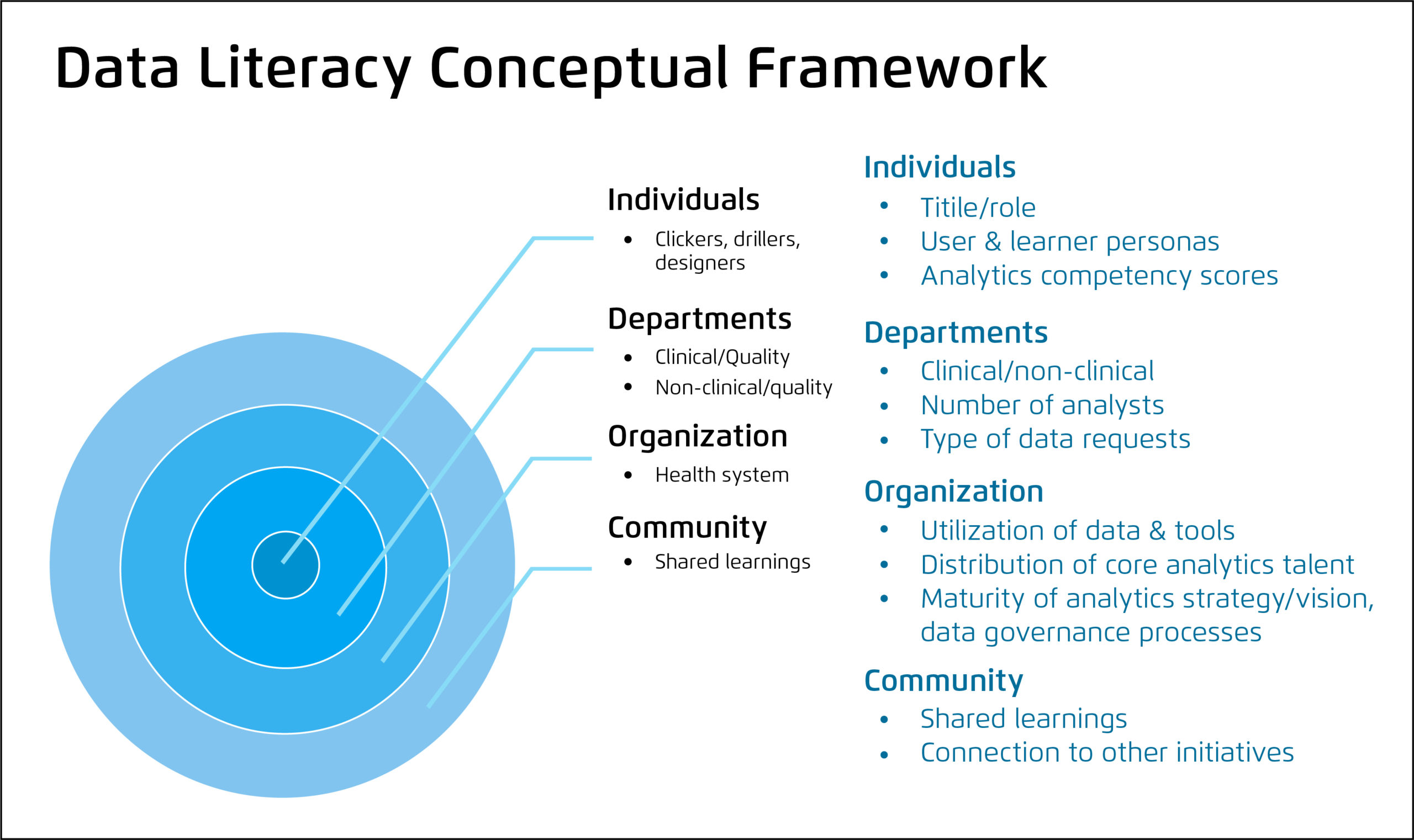
If health systems only focus on developing data literacy in individual learners, they can’t see things from a higher level (e.g., the department level). Looking at the distribution of analytics talent at every level to identify opportunity and target learners also promotes effective data literacy. Evaluating and measuring healthcare data literacy at all levels offers a better vantage point for leadership to measure progress and narrow in on missed opportunities or other areas needing more time-intensive training.
The Health Catalyst Healthcare Analytics Adoption Model (HAAM) (Figure 2) is a valuable tool to evaluate an organization’s progress as it embarks on the journey to becoming data driven. Most healthcare organizations start at, or near, the bottom of the HAAM. At this point most individual users, teams, and departments are working in silos, implementing fragmented solutions, and working on their own goals while relying on their own data sources.
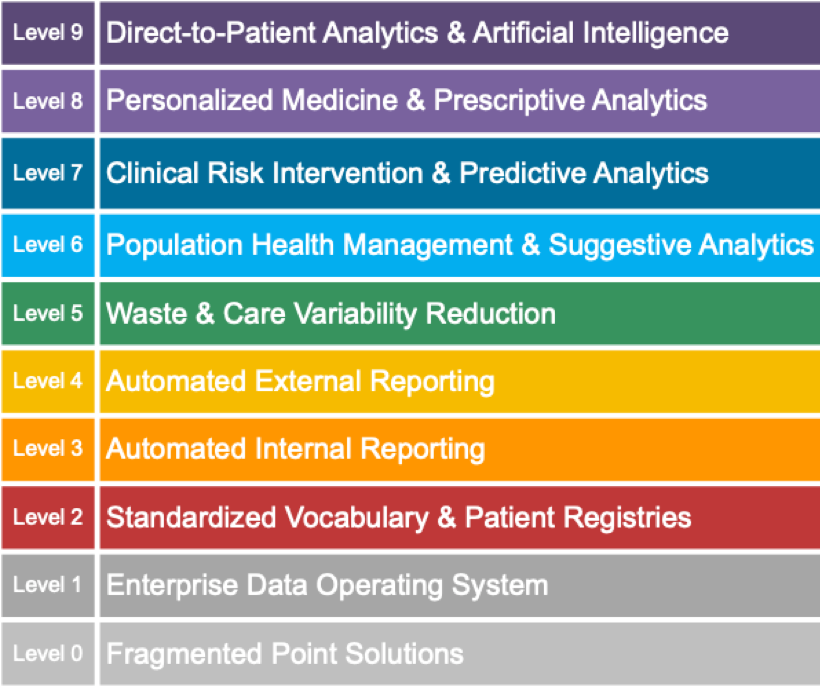
To become a data-driven organization, health systems should invest in an integrative baseline architecture, such as the Data Operating System (DOS™), in which data starts to come together into one place. As health systems progress, they develop analytics talent in their team members, start utilizing data more efficiently, and finally, drive healthcare improvements. From there, health systems become more forward thinking with data and leverage insights to improve processes, quality, and create predictive models to identify opportunities even closer to the point of care.
Data literacy should be an integral focal point for organizations—as part of their data governance strategy—to close gaps between delivering insights and acting on them, which will accelerate outcomes improvement. The Data Life Cycle (Figure 3) illustrates the complete data lifecycle and cyclical relationship of data literacy to data quality and data utilization through three core elements:

Data literacy programs can benefit any health system, regardless of where it is in the journey to becoming data driven. Healthcare data literacy programs support the utilization of high-quality data to drive insights with confidence. When more team members have the ability to effectively collect, manage, evaluate, and apply data in a critical manner data, they will effect long-lasting change.
Assessing analytics user personas within clinical and operational departments allows improvement teams to measure and visualize baseline analytics talent trends across the organization. Gathering baseline assessment data in a thoughtful structured way—rather than assuming a baseline based on personal anecdotes or one-off experiences—is key to describing a health system’s analytic current state, developing the data literacy program, and measuring progress moving forward.
A health system can leverage the results of the organizationwide analytics assessment along with data literacy best practices to develop an outcomes improvement plan. The plan should include development of learning objectives, competency-based curriculum, and outcomes measurement.
A sample curriculum could include five components:
The health system implementing a data literacy program should also institute process changes to make new employees aware of data-literacy learning opportunities. For example, an organization can embed data literacy training options into new leader orientation, which includes application training as part of standard work when a new tool is built.
The health system should also update its workflows and checklists to further include analytics engineers or developers in the data process. For example, an apprentice model for leading and shadowing data literacy trainings ensures creation of a bench of data experts and capitalizes on those individuals most interested in teaching. This prevents making teaching a burden for specific team members and allows less tenured experts to build confidence in the subject. With a bench of experts, the organization is also in a position to scale education as more learners emerge.
Ideally, a health system monitors data literacy at the organizational level, as data is an organizationwide investment. A multidisciplinary, or a multirepresented, group of stakeholders also discusses and monitors data quality processes and data utilization trends.
For example, a data governance steering committee—led or co-led by the chief analytics officer and the chief information and improvement officer—for leaders across the organization oversees data requests and prioritizes which data is most valuable and how to use it. The steering committee can also focus on opportunities to grow analytics talent, eliminating silos and identifying ways for groups to work together and benefit from each other’s efforts, setting data literacy goals, evaluating the data literacy program and the ROI, and finding ways to scale programs across the organization.
Healthcare organizations strive to get the most out of their team members—from data analysts to clinicians. To maximize potential, organizations first need to assess the level of analytics talent and opportunities for improving/developing that talent. Once a health system has identified areas for improvement, it can tailor training needs and competency programs to fit the unique needs of the health system and its data users.
Data literacy accelerates effective analytics use and improves clinical, operational, and financial outcomes at every level of the organization. To become successful data-driven organizations, health systems must build and maintain data literacy.
A programmatic approach to implementing data literacy education will increase utilization of available technology and reduce ad-hoc requests for analytics support, empowering team members to use data tools directly (self-service) and improve outcomes more quickly. Programs targeted at improving data literacy in healthcare organizations should include regular assessments of analytics skills and learning needs, embedding learning opportunities at various levels of the organization, and monitoring progress as part of data governance practices.
Would you like to learn more about this topic? Here are some articles we suggest: