Compared to industries such as aerospace and automotive, healthcare lags behind in decision support innovation. Following the aerospace and automotive arenas, healthcare can learn critical lessons about improving its clinical decision support capabilities to help clinicians make more efficient, data-informed decisions:
1. Achieve widespread digitization: Healthcare must digitize its assets and operations (patient registration, scheduling, encounters, diagnosis, orders, billings, and claims) for effective CDS similarly to how aerospace digitized the aircraft, air traffic control, baggage handling, ticketing, maintenance, and manufacturing.
2. Build data volume and scope: Healthcare must collect socioeconomic, genomic, patient-reported outcomes, claims data, and more to truly understand the patient at the center of the human health data ecosystem.
 Download
Download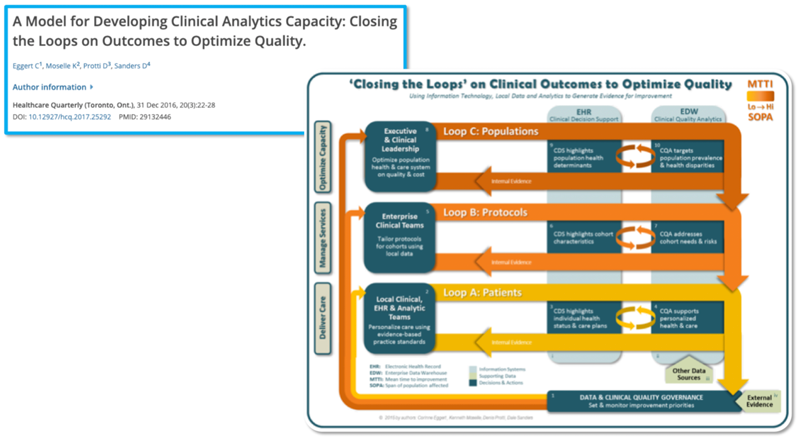
This report is based on a webinar presented on January 16, 2020, by Dale Sanders, Health Catalyst Chief Technology Officer, and Scott Weingarten, MD, MPH, Chief Executive Officer, Stanson Health, titled, “Clinical Decision Support: Driving the Last Mile.”
Industries outside of healthcare are pushing the limits of innovation with artificial intelligence (AI)-enabled decision support. Yet, healthcare lags behind in how it leverages AI in clinical decision support (CDS) to help clinicians make more efficient, data-informed decisions. Health data volume and quality aren’t always robust enough to support informed decisions, and the industry needs to evolve concepts around how to use decision support.
EHR adoption provided a foundation for CDS by delivering patient information to clinicians at the point of care. Now healthcare needs a framework to build on the EHR to help clinicians and patients benefit from meaningful, precise decision support. By looking to the automotive and aerospace sectors, both highly digitized since the 1990s, as role models in innovation in decision support, technically and culturally, healthcare can create a pathway for CDS that leverages available technology (e.g., AI) in pursuit of improving outcomes and lowering costs.
Following the aerospace and automotive arenas, healthcare can learn critical lessons about improving its CDS capabilities:
Healthcare must digitize its assets and operations for effective CDS. Aerospace, for example, digitized the aircraft, air traffic control, baggage handling, ticketing, maintenance, manufacturing. Following suit, healthcare needs to digitize patient registration, scheduling, encounters, diagnosis, orders, billings, and claims.
According to a paper from IEEE, simple AI models and a lot of data trump more elaborate models based on less data. As the automotive industry demonstrates, vehicle health monitoring relies on a data-intense environment. Tesla, for example, has 780 million miles of driving data, and adds another million every 10 hours. The automaker uses these digitized assets to extend the life, quality, and safety of its vehicles.
While healthcare big data volume is projected to exceed data growth in other sectors through 2025, effective CDS demands better quality data. To truly understand the patient at the center of the human health data ecosystem, healthcare must collect socioeconomic, genomic, patient-reported outcomes, claims data, and more. Currently, the industry only collects data on patients seeking care and no data on patients not seeking care. Putting all data categories on a timeline for strategic data acquisition creates a roadmap for the industry over the next 5 to 10 years to increase the precision of understanding of patients.
Meanwhile, healthcare needs to ensure the quality of its growing data volume. Studies have highlighted concerns about data quality, including poor disease labeling in EHRs, discrepancies in observed clinician behavior and EHR documentation, and questionable randomized clinical trials conclusions.
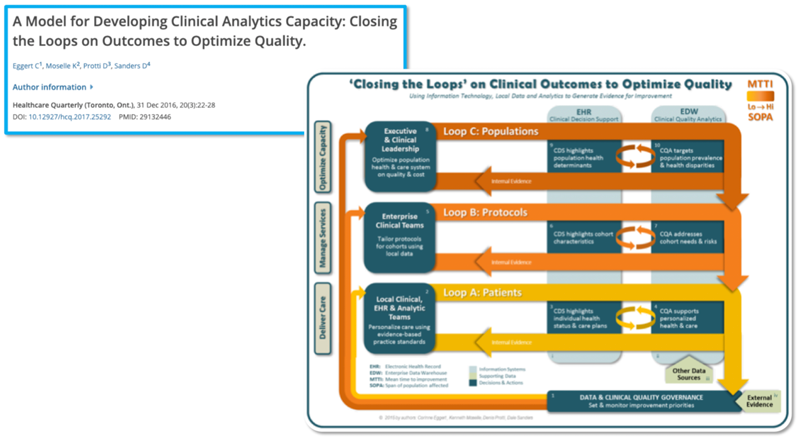
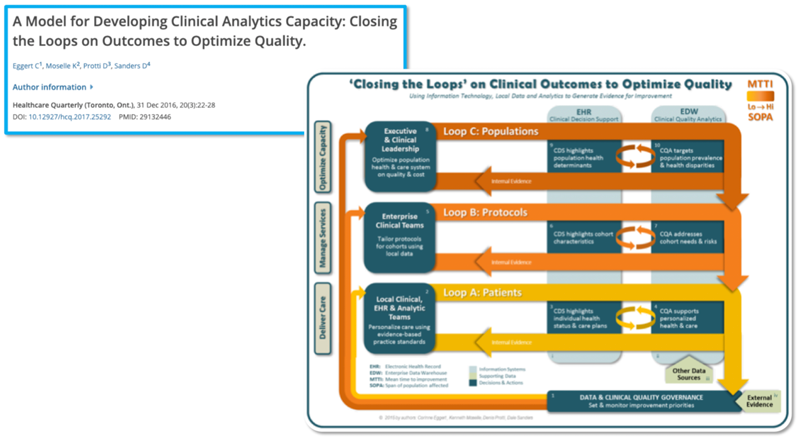
Developing the clinical analytics capacity for effective decision making occurs in three closed loops: the top loop is decisions around populations, the middle loop is decisions we make about protocols, and the final loop is the decisions about patients (Figure 1). From population health decisions that affect millions of people to a public health setting impacting subsets of people in general, down to the patient level, the three closed loops of CDS outline certain protocols for certain patients.
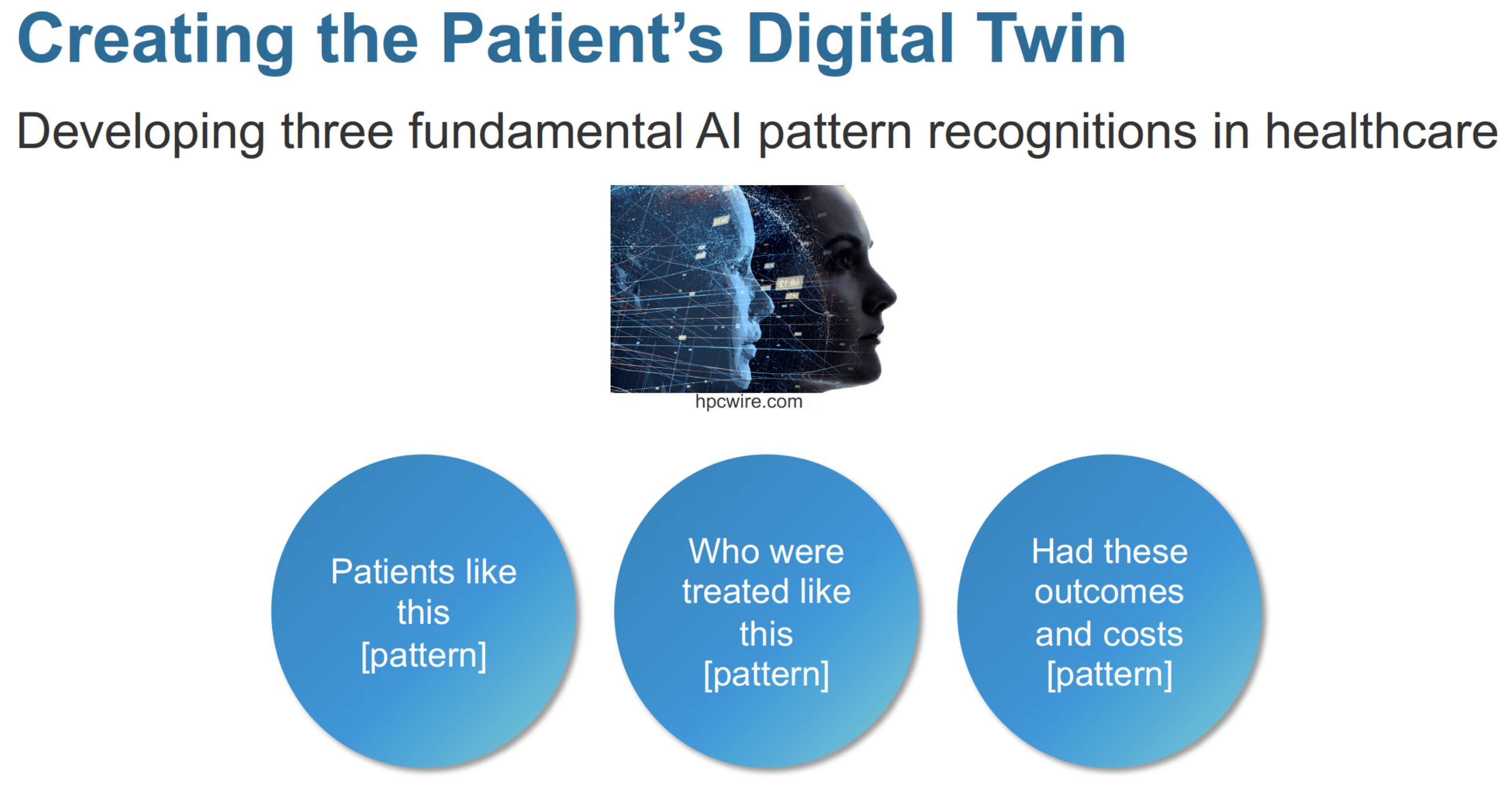
To achieve the three closed loops of CDS, healthcare can adopt the notion of the digital twin and better leverage AI to improve pattern recognition—using the power of AI to reveal patterns in data the human brain would not otherwise see—versus using AI for prediction. Figure 2 shows three applicable patterns:
Borrowing from the progress of the automotive and aerospace industries, health systems clearly need to increase the data for every member of their network. This includes increasing data collection from wearable innovation, such as microns thin, wireless sensors embedded into wafer-thin, skin-like patched.
The need for and ability to collect more health data will give way to a new type of skillset—a “digititian,” who sits between the patient and the physician and the care team to develop digital profiles of patient types. For example, a patient with diabetes should have a different digital profile than a patient who’s undergone a spine surgery. The digititian would define different patient data profiles, then work with the patient and the care team to collect and analyze data and identify actions for the whole care team.
Following the roadmap to bigger, better health data and improved CDS, healthcare can better optimize bringing key insights to practice. According to the National Academy of Medicine, there’s a 17-year gap between the discovery of potentially lifesaving information and its widespread translation into practice. Minimizing that gap needs to be an industrywide priority. In addition, a couple of studies in the New England Journal of Medicine discovered that patients are treated with care consistent with the evidence only about 50 percent of the time.
Add to that equation studies in JAMA showing about a third of all healthcare costs are waste, and 10 percent of healthcare is overtreatment, in which the harm exceeds the benefit. Based on these findings, there’s ample opportunity to improve.
The good news is, with heavy investment in medical research, healthcare information is expanding. The estimating doubling time of medical information is increasing from about 50 years in 1950 to 73 days in 2020.
However, as data grows, providers will need the right technology (e.g., cloud-based platforms) to absorb and manage all the information that could benefit patients and leverage it for CDS. To identify an effective approach to using expanding amounts of healthcare data, a University of Utah study reviewed previously published research on interventions aimed to improve the quality of care. It concluded that when an organization provides CDS is part of its workflow, it’s 112 times more likely to improve care than without CDS.
By optimizing CDS, health systems are improving patient outcomes and lowering cost. Health systems can design order sets and preference lists to promote the right action and discourage the wrong action. For example, using strategic order sets and preference lists, Cedar Sinai saved approximately $3.7 million a year with no change in mortality, use of rapid response teams or in code blue, while maintaining a high level of quality.
Health systems can also implement CDS to accelerate evidence or the translation of evidence into practice. A 2019 study showed that antidepressants and antipsychotics with high anticholinergic properties can increase the risk of dementia by 50 percent when taken over a three-year period. Some of these antidepressants and antipsychotics show up on order sets and preference lists, even though antidepressants and antipsychotics exist with fewer anticholinergic effects. This leaves an opportunity to reduce preventable dementia and improve the health of communities, as well as the burden and morbidity associated with dementia.
As CDS, and healthcare IT capabilities overall, evolves to better leverage AI, the industry can expect increasing data inputs (e.g., wireless sensors) to include patient preferences, social determinants of health, genetic information, proteomic information, microbiome information, and precision medicine that will enable even better guidance on what will help patients and what will not. There’s also effort underway to make the EHR more usable using voice recognition. In addition, a number of companies are working on ambient listening devices and virtual assistants to listen to provider-patient conversations, structure the information and enable the information to guide to not only the healthcare provider but also the patient at home.
If healthcare looks to the automotive and aerospace industries for capable decision-support role models, it can identify a fundamental two-part for more capable CDS: increased digitization and more increased data volume and scope. By building these two assets along with better leveraging AI in data management and decision making, healthcare can achieve the CDS to positively impact patients and the entire system of care delivery.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.