Thibodaux Regional Medical Center formed a sepsis improvement team to reduce mortality and costs while enhancing patient experience. By implementing best practices, analytics, and engaging clinicians, the organization has decreased the sepsis mortality rate, reduced ICU length of stay, and improved patient satisfaction.
Although Thibodaux Regional Medical Center had achieved sepsis mortality rates below the national average, leadership knew they could do even better.
To further improve sepsis outcomes, Thibodaux formed a sepsis improvement team charged with reducing sepsis mortality and lowering costs while improving the patient experience. The team implemented best-practice care protocols, an advanced analytics system, an application targeted at sepsis care, and an adoption approach that engaged clinicians using education and data.
Backed by executive leadership and guided by clear goals, the sepsis improvement initiative has achieved impressive results in just six months.
Sepsis is a serious medical condition caused by an overwhelming immune response to infection that can lead to tissue damage, organ failure, and death.1 In fact, between 28 and 50 percent of people who get sepsis die.2 Unfortunately, sepsis is a growing problem in the United States: The number of hospitalizations due to sepsis increased from 621,000 in 2000 to 1,141,000 in 2008 and continues to rise.3
For many years now, Thibodaux Regional Medical Center in Louisiana has dedicated itself to improving sepsis outcomes. Its emergency department (ED) is a level 2 trauma center handling approximately 43,000 patient visits a year. A number of these ED visits are patients with sepsis, severe sepsis, and septic shock. Although the medical center had launched a sepsis improvement project in the past and achieved sepsis mortality rates better than the national average (an improvement that others would consider success), it was not enough to satisfy Thibodaux leadership. They were determined that they could do even better.
Before launching a sepsis project, however, Thibodaux leadership wanted to make sure that continued work on sepsis was what the community needed most. Like most healthcare organizations, Thibodaux had finite resources to dedicate to improvement, and leaders wanted to use those resources wisely. Thibodaux therefore used a prioritization methodology that included Pareto analysis using the Key Process Analysis (KPA) application from Health Catalyst (see Figure 1) as well as impact analysis, quality measures benchmark review, and organizational readiness. Through this methodology, leaders determined that sepsis management and pneumonia were the biggest medical opportunities for improvement. Because they felt that work on sepsis would have a positive effect on pneumonia, they gave sepsis the priority.

Thibodaux launched a sepsis improvement team under its care transformation structure that provides executive sponsorship, physician leadership, resourcing, and oversight for its improvement projects. Leaders gave the sepsis improvement team a threefold challenge aligned with the IHI Triple Aim: Reduce sepsis mortality and lower cost while improving the patient experience.
Under the clear and effective sponsorship of Thibodaux’s CEO, the sepsis improvement team was given the right people, the right tools, and the right environment to be successful. Key components of this supportive infrastructure included the following:
Because physician engagement and adoption would be an essential element of success for this project, the improvement team gathered input from the admitting physicians and kept them in the loop before formulating the improvement plan. In the course of this information gathering, the team identified two key facts about sepsis. First, sepsis is a silent killer. The patient frequently presents with multiple non-specific complaints that make it easy to misdiagnose the patient and fail to recognize the seriousness of the patient’s condition. Second, one thing about sepsis that is unique among infectious diseases is that in severe sepsis, timing becomes the most important component of the patient’s care.
Armed with this information, the sepsis team determined that the organization needed to focus its efforts first in the ED, where the majority of sepsis patients presented. Specifically, they needed to improve early recognition and shorten the time to treatment.
Using Thibodaux’s adopted care transformation methodology, the sepsis improvement team’s solution focused on three areas (representing the three systems of care transformation):
The following describes specific ways in which Thibodaux addressed these three essential improvement areas.
Before Thibodaux redoubled its sepsis management effort, its analysis had indicated several key problems. First, no screening tool was in place in the ED for early identification of sepsis patients. Furthermore, clinicians followed best practice recommendations for sepsis inconsistently, and treatment was frequently delayed pending an accurate diagnosis.
To improve early recognition of sepsis in the ED, the team implemented a screening tool that clinicians could use as patients presented in the ED. All patients are now screened for suspected infection, altered mental status, and systemic inflammatory response syndrome (SIRS) criteria. If patients meet certain of those criteria, they are placed on sepsis alert or sepsis watch. Patients with a sepsis watch or sepsis alert show up in the EHR with a uniquely colored patient header, helping ensure that they get rapid treatment.
Thibodaux also implemented sepsis care protocols. Clinicians treat patients with a sepsis watch or sepsis alert according to the sepsis triage protocol. This protocol empowers nurses to implement the interventions needed to complete the septic workup. Use of the protocol has resulted in the entire septic workup usually being completed within 13-25 minutes. Results are back from workup within an hour and often much more quickly. Positive screening for severe sepsis or septic shock triggers a sepsis alert in the medical record that flags the patient to be put into the pathway of accelerated care and be seen within 15 minutes of arrival to the ED.
Thibodaux also incorporated the three-hour best practice bundle developed as part of the national Surviving Sepsis Campaign4 into its improvement effort. The bundle consists of the following recommended treatment elements within three hours of the time of presentation:
The first two are covered in the triage protocol as part of the septic workup, and the remaining two elements are included in the sepsis protocols and order sets. The most difficult change in practice for Thibodaux physicians was the adoption of rapid IV fluid administration (known as fluid resuscitation). This practice may conflict with what many physicians were taught in medical school, but because of new evidence, it is now embraced as a key lifesaving intervention for patients with sepsis. Education, research, and improved outcomes needed to be shared with physicians to convince them to change their practice. To further reinforce this change in practice, the fluid resuscitation protocol was added to the ED sepsis protocol.
Thibodaux recognized the importance of analytics in convincing clinicians of the need for practice change, as well as in providing the information needed to sustain those practice changes. The team deployed an advanced analytics application for sepsis powered by Health Catalyst to support process improvement efforts, making it possible to see the impact of interventions and to correlate those interventions with patient outcomes. The combination of the improvement methodology with analytics has given Thibodaux the ability to be very responsive and proactive.
As clinical leaders in the ED interact with the sepsis analytics application, they frequently start with the sepsis summary dashboard (see Figure 2). There they can view all the major outcome metrics related to sepsis in one place, with the ability to narrow in on specific dates and look for trends and practice issues. This enables them to quickly identify issues that need further investigation so they can dig further into the application to get answers.

The sepsis team also included in its application an early recognition dashboard that is used to see how often the protocol is applied, how well the screening is done, and how quickly the physicians are getting to see the patients. Once again, easy access to this information keeps leaders informed and alerts them to the need for celebration or intervention.
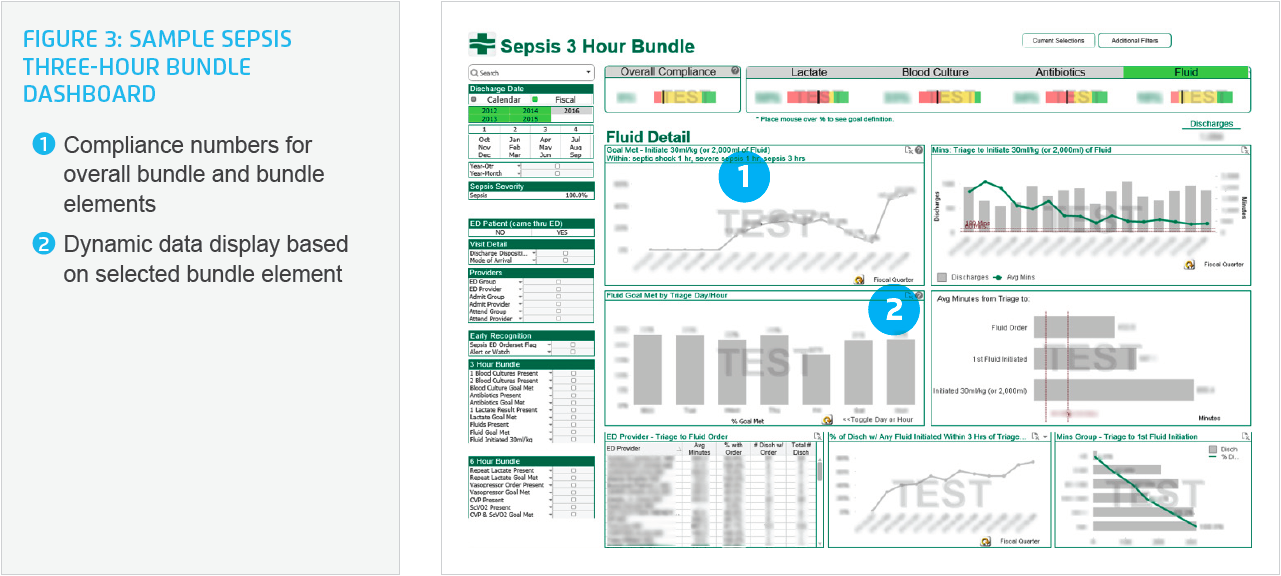
Physician leaders access the three-hour bundle screen (see Figure 3) frequently to see where variation in practice is creeping in. They use the application to identify cases that need further scrutiny and are able to drill down to individual patients and providers and intervene as needed to improve patient care. The interactive nature and almost immediate access to the data enables physician leaders in the ED to explore the relationship between interventions and outcomes, search for root causes, and identify opportunities for further improvement. By providing data and information to support conversations with clinicians, this dashboard serves as a key tool for sustaining clinical practice changes.
The advanced analytics application provides physician leaders with a patient-detail dynamic report that enables them to drill down, sort the columns, and view patient-specific data in a way that answers the particular question they are researching. Manual chart reviews were required previously to get to patient information. Now leaders can evaluate not just one patient, but multiple patients or cohorts of patients in a dynamic way.
Keeping faithful to its mission of patient-centered excellence, Thibodaux also incorporated patient satisfaction information in the application. This data helps leaders make sure that changes in practice are not having a negative impact on patients’ experience of their care.
The sepsis improvement team knew that well-laid plans and sophisticated analytics applications would not deliver successful outcomes without a deployment plan that engendered high levels of engagement and adoption. The team took this task head on. In addition to using agile methodology to develop and deploy the analytics application, team members provided clear communication with consistent messaging in multiple venues. This included education and training to foster adoption.
The team used multiple methods of communication across the organization to share expectations and outcomes with the medical staff, the board, and frontline staff. Team members clearly communicated the end result that they were moving toward. They had fun with the education process, starting off with a big kickoff event with a band, caterer, and T-shirts. They hosted “Sepsis on the Road” seminars where they sat with primary care physicians, showed them the application, and shared their plan for practice changes to improve the care for sepsis patients. These seminars included a high level of physician participation and enabled doctors to talk with doctors about the coming changes. Importantly, Thibodaux provided time off regular duties so that staff could attend these events, as well as extra rewards to keep clinicians incentivized to participate on these teams.
Thibodaux has achieved an observed risk-adjusted mortality rate for sepsis patients considerably less than predicted, which leaves no question that its sepsis management effort has resulted in lives being saved. Thibodaux leadership charged the sepsis improvement team with improving sepsis mortality, decreasing cost, and improving the patient experience. The team accomplished all of these goals within six months of deploying the sepsis solution.
Assisted by analytics technology, it was a change in practice that drove Thibodaux’s sepsis mortality rate down to approximately half of the national average. Thibodaux measured compliance with newly implemented best practices and discovered the following:
Thibodaux achieved this cost reduction in multiple ways. Most significantly, it reduced ICU LOS by .96 days. Furthermore, it achieved time savings among physicians due to easy access to patient information in dashboards and for staff by reducing manual chart audits.
Patient satisfaction is a difficult metric to impact because of its multifactorial nature. To get this large of an impact in six months is tribute to the effective, yet caring and compassionate way that the ED staff carried out practice changes.
In addition to quantifiable results, the work of the sepsis improvement team has allowed ED clinicians to impact the quality of life of their patients. As just one example, the first day the sepsis protocol went into place an extremely ill cancer patient in septic shock came into the ED. His quality of life had suffered due to the amount of time he had to spend in hospitals, and he and his family fully expected that this additional illness would require a prolonged hospitalization that would most likely end in his death. With the changes in practice that had been put in place for treating sepsis, clinicians were able to intervene and treat him quickly. After a short stay in the ICU, he was able to go home, gather his family, and spend time with them at the end of his life.
“I’ve been doing process improvements for a long time, and physician engagement was the thing we were always missing. This sepsis improvement effort has really proven that having doctors talk to doctors is the way to get things done.”
– Danna Caillouet, Program Coordinator
Thibodaux’s sepsis initiative serves as a model for using data to identify effective clinical processes and track outcomes. The team will soon move to the next level: Using data to motivate individuals. This will include the expansion of provider metrics to give providers greater insight into the effectiveness of their processes. The team will also turn its attention to hospital-acquired sepsis and focus on implementing the six-hour bundle.
Finally, the team will continue its education and engagement efforts. Recognizing that turnover in the ED staff will affect outcomes, team members are developing a sepsis-focused orientation program for new employees to ensure that their gains are not lost. The need for strong leadership in the ED that is focused on sepsis improvement will continue to remain the key to ongoing improvement. They will also be focusing on education of admitting physicians and the transitions of care for patients leaving the hospital or going to the ICU.
Thibodaux’ commitment to continuous clinical improvement will continue to be driven by the attitude that improvement is an ongoing journey—not a destination—and this in turn will ensure that their results will only get better.