To succeed in risk-based contracting, Mass General Brigham (formerly Partners HealthCare) utilizes its data platform and population health analytics. This approach enhances data accessibility and visualizations, empowering managers with insights and promoting physician engagement in managing cost trends for high-quality, safe care delivery.
As risk-based contracts become more predominate, the need for healthcare organizations to deliver high quality, safe care with minimum waste will only grow.1 Providers that take on this risk in the accountable care environment must focus on developing care management programs for high need, high cost patients—populations that require complex and multi-faceted care.
Such programs involve regular coordination among specialists and primary care teams, especially for patients that may have multiple chronic conditions or advanced illness.2 These teams are tasked with four primary responsibilities:
As the largest integrated health care delivery system in Massachusetts, Mass General Brigham (formerly Partners HealthCare) is deeply experienced in coordinating care across numerous entities. It is also an early pioneer of population health programs. Beginning in 2011, Mass General Brigham launched new care models designed to manage the health of populations while reigning in growing healthcare costs; an initiative that has since evolved into a system-wide integrated care management program.
Also in 2011, Mass General Brigham signed accountable care contracts within all major payer categories, placing a significant fraction of revenue in risk-based arrangements. This new reimbursement model presented Mass General Brigham with the formidable challenge of holding increases in total medical expenses below the national average. To meet this and other objectives in the new value-based landscape, Mass General Brigham sought to implement an analytic environment that would manage risk and optimize value for high-need populations.4
Risk-based contracting for population health management is grounded in simple math. Healthcare organizations that exceed total medical spending targets for these contracts affectively absorb a penalty. Those that keep expenses below these targets create a savings they can keep. With multiple at-risk contracts, Mass General Brigham currently is at risk for the costs of care for over 500,000 patients, making medical expense management critically important—especially for high-risk, high-utilization populations. A typical patient within the health system’s integrated care programs, for example, is 76 years old, has more than three acute-care hospitalizations per year, and is taking more than 12 active medications.
At the same time, Mass General Brigham recognizes that it is inconsistent with provider values and workflow to manage different subpopulations of patients to different targets. Therefore, Mass General Brigham has created an Internal Performance Framework (IPF) that uses a single set of performance targets, Cost Standardized Medical Expenses (CSME), and a single incentive pool for all Mass General Brigham contracts, with the goal of promoting the best possible care for all patients while also meeting the demands of multiple external contract requirements. To gain insights into the populations, care teams needed the ability to organize and study a combination of data across the enterprise. In a parallel need, financial decision makers required insights into clinical performance.
Advancement in either area, however, was hindered by an IT infrastructure with limited interoperability, and separate data warehouses for clinical, financial and claims data. Without a foundation in place to house and integrate data from multiple sources, analytic activities at Mass General Brigham were historically done manually—a time intensive process prone to error—or not at all. Mass General Brigham recognized the need for more effective analytics capabilities to manage its risk-based contracts, especially to identify cost reduction and care improvement opportunities.
To enable the analysis of current performance and drive clinical transformation, Mass General Brigham implemented a late-binding enterprise data warehouse platform (EDW) from Health Catalyst. The EDW aggregates clinical, financial, operational, claims, and other data to create consistent views of the data to inform decisions for providers and managers alike. It uses common patient/provider identifiers to assure accurate identification of both patients and providers. This in turn supports the use of flags to easily identify high-risk patient cohorts.
As the EDW was implemented, Mass General Brigham and Health Catalyst developed a number of analytic applications that enable Mass General Brigham’s leaders to make informed decisions in the new era of value-based care. This includes applications to effectively manage episodes of care and—the focus of this story—populations within at-risk contracts.
The ACO/shared risk management and population health advanced analytics gives Mass General Brigham new insight to manage populations with superior care and minimum waste. It measures and tracks the expenses and utilization that drive population trends associated with risk contracts, and identifies patient populations that generate higher expenses.
In an effort to accurately attribute medical expenses to a particular condition or episode of care, Mass General Brigham uses grouper tools to categorize care data in meaningful ways. Groupers are a generally accepted method for aggregating healthcare data to assess condition-specific or event-specific utilization and costs. Healthcare services can be analyzed and grouped by specific clinical conditions to generate an overall picture of the services used to manage that condition. Beyond services, groups can be defined by a wide range of categories, such as site of care, to analyze cost and utilization for many different types of population data. Just some of these include product lines, primary care panels, and disease populations.
Mass General Brigham developed two industry standard grouping technologies to develop two useful views of the data. The first is a “reconstituted” grouper that provides a user-friendly breakdown by category of care—such as outpatient, inpatient, medications, imaging, labs, pathology, and post-acute. The second standard grouping technology enables mutually exclusive views of a patient’s care by clinical service line—for example, cardiovascular, endocrine, renal, and gastrointestinal, to name several.
The application supports the ability to drill up or down to the individual patient, provider, or provider group level, and helps drive managerial action when troublesome cost trends are identified.
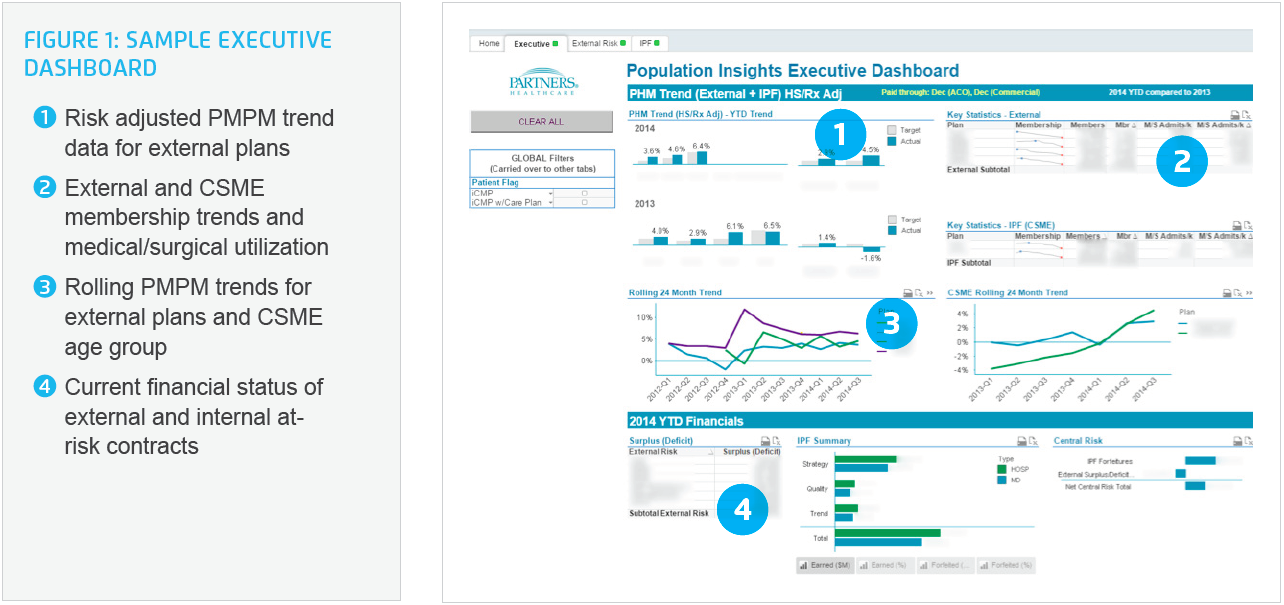
The executive dashboard provides high-level trend information across all plans, including per-member-per-month (PMPM) payments to providers from payers, membership levels, and medical/surgical admissions, plus financial data relevant to administrative users. The dashboard also provides executives with information regarding monthly performance relative to external risk and internal performance targets (Figure 1).
Further, the external risk dashboard displays a high-level comparison of the external plans in terms of PMPM trends for the current year (relative to the prior year), and for the previous year (relative to two years prior). All other visualizations on this dashboard provide details for a specific selected plan (Figure 2). Payer-specific data is displayed by clinical category, location hierarchy ([Regional Service Organization (RSO)>practice>primary care provider]), “reconstituted” service group and utilization types.

Similar to the external risk dashboard, an internal performance framework dashboard displays a high-level comparison of this initiative’s plan rollups in terms of PMPM trends for the current year (relative to the prior year) and for the prior year (relative to two years prior).
Mass General Brigham experienced rapid time-to-value by using an iterative development approach for the EDW and analytics application. Functionality was released in six-week cycles, quickly bringing the tool into the hands of end users. Improvement ideas were rapidly incorporated with each cycle.
Information is accessible to managers as soon as it is released. Integrated clinical, financial, and claims data allows comprehensive views of cost trends. Instead of a push report that could take up toone month to create, for example, the information is available to managers as soon as it is released. This allows managers to easily monitor and identify drivers of cost trends for timely action.
Customized service grouper, mutually exclusive clinical grouper, and Practice/RSO grouper to drive managerial action. Mass General Brigham developed a customized service grouper with six top-level groups: inpatient, post-acute, imaging, lab/pathology, outpatient, and pharmacy. More than 20 clinical categories were also developed, allowing Mass General Brigham to attribute total medical expenses to specific categories and conditions without overlap. The categories are additive (either by identifying a primary condition if done on a patient level, or by using claim level diagnosis). By making these views mutually exclusive, managers are assured that expenses are accurately attributed to an individual patient or provider—key to avoiding double counting of costs, revenue, volume, and so forth.
Enhanced visualizations that enable analytic insights. Intuitive visualizations make it easy to navigate and digest complex information. Data can be consumed by numerous front-end visualization tools based on the end-user preference, or queried directly within the EDW. Trends are viewable by key location, service, and clinical categories, with additional ability to drill down to the atomic level, such as by individual physician or patient, to identify and understand the root cause of cost increases.
Visualizations are based on end-user needs and responsibilities; for example, clinicians need clinical views while finance department staff require primarily financial views of data. This is also a particularly useful representation of data for spotting potentially problematic cost trends. For instance, if diagnostic and treatment costs for a given condition by a specific provider are on a sudden upswing, managers can drill down to determine whether these costs are justified based on clinical efficacy, whether an alternative treatment model is justified, or whether provider education is warranted.
To give a specific example, the treatment of hepatitis C with the FDA-approved oral agent Sofosbuvir has proven to be effective—but it can quickly lead to exorbitant costs for an organization. The drug costs $1,000 a pill, or an estimated $84,000 for its entire 12-week regimen. As a result, an organization needs to assure that this effective, yet costly drug is used wisely. Otherwise it can result in millions in excess costs.
The analytics supports data-driven conversations with physicians to understand and manage cost trends. In one possible scenario, if a physician is convinced that the data is accurate and shows he or she is an outlier in ordering excessive and expensive advanced imaging studies for low back pain, mentoring can ensue to encourage the physician to use the advanced imaging at a more appropriate rate.
“It is not sufficient to base risk-based contracts on hunches. To be successful, they have to be based on good data.”
- Sree Chaguturu, MD, Vide President, Population Health Management
Mass General Brigham continues to enhance the population health and risk-based analytics application and expand its use. New capabilities are under development to further support enterprise quality as well as safety reporting and improvement. These and other efforts will further drive adoption of tools that help Mass General Brigham manage value-based care with the best information possible.


