MultiCare established a Clinically Integrated Network (CIN) to improve patient care and outcomes through multidisciplinary collaboratives. This approach has led to a 65 percent reduction in sepsis mortality, a 75 percent decrease in guideline approval time, and an estimated $100 million in systemwide cost savings.
To transform the U.S. healthcare system, providers are in determined pursuit of the Triple Aim: improving the experience of care, improving the health of populations, and reducing the per capita costs of care.1 MultiCare, an integrated delivery system (IDS) in the Pacific Northwest, is fully committed to excelling in all three areas of the Triple Aim and is establishing a structure and culture to accomplish that goal. This is no small challenge for an organization with more than 10,000 employees, 500,000 annual outpatient visits, and 1,188 beds.
In the last 12 months, as part of its core strategy, MultiCare Health System launched MultiCare Connected Care, LLC, as its Accountable Care Organization (ACO) and Clinically Integrated Network (CIN). This serves as a model for value creation that benefits patients, providers and payers alike. The CIN is comprised of three buckets of select providers: physicians/advanced practitioners (employed and select independent), ancillary services, and facilities such as acute care hospitals and ambulatory surgery centers.
Providers in the CIN are linked by strong clinical care coordination, evidence-based care standards, and care pathways. The responsibility for creating and implementing these standards and pathways lies with Collaboratives—multidisciplinary, clinically focused teams charged with developing system-wide clinical care standards and pathways and then collaborating with operations to get them implemented. These Collaboratives are the engine that drives MultiCare Connected Care.
MultiCare’s collaborative journey began in 2010 and has produced remarkable improvements in patient outcomes—but the health system learned many important lessons along the way. Specifically, MultiCare learned that building a collaborative framework is an iterative process (see Figure 1). The organization’s leaders discovered that they had to make a conscious effort to lay out a roadmap for success, recognizing that progress does not equal perfection and that the framework had to be phased in rather than implemented all at once.

Another critical lesson that MultiCare learned in establishing its Collaboratives was the importance of combining a grassroots approach to developing improvement teams with strong support from top executives. The grassroots approach engages clinicians and other personnel on the frontlines of care. Such engagement is essential. Without it, the collaborative will fail to change practice and will not deliver the desired results. However, without leadership support, the grassroots approach can lead to disillusionment and a lack of resources that makes accomplishing the goals of the collaborative very difficult.
MultiCare experienced this dynamic firsthand when it launched its first two Collaboratives, which focused on improving outcomes for sepsis and heart failure (HF). The organization launched sepsis and HF as a grassroots movement with frontline clinical operations and clinicians. The team experienced a high level of enthusiastic engagement in the beginning, but then had difficulty implementing the improvement initiative across the system. Not until strong executive sponsorship and specific dedicated resources were brought into the equation were the Collaboratives able to gain the recognition and resources necessary to do their job effectively.
Based on this early experience, MultiCare understood that without complete investment at all levels of the organization (from top executives to professionals on the frontlines of care), the adoption of concepts and tools for system-wide improvement and the necessary culture change would be variable and unreliable, leading to uneven outcomes. In launching future Collaboratives, MultiCare ensured both grassroots engagement and leadership commitment, including allocating resources dedicated specifically to support the collaborative.
Another important lesson MultiCare learned in launching Collaboratives was the importance of having a defined prioritization process. From the beginning, MultiCare leaders were faced with decisions about which clinical areas to focus on, how to start, and how many Collaboratives to launch. Improvement across such a large health system required prioritization and focus to make wise decisions and to ensure that the appropriate resources were available and committed.
To tackle questions of structured prioritization, MultiCare put oversight for these decisions in the hands of a credible body that could ensure that initiatives were sequenced appropriately. When limited resources hampered the progress of Collaboratives, this body had to make decisions about whether to take on many projects at the same time and achieve incremental results or focus on the critical few with more dramatic results.
MultiCare also discovered that the level of change management required to create a successful CIN dedicated to continuous improvement should not be underestimated—particularly when shifting from a hospital-centric focus to a system-wide approach. Participation from each hospital in the system as well as active participation from both nursing and physician representatives was essential. Importantly, MultiCare affirmed that data and evidence were essential to supporting adoption of a system-wide collaborative model and to effect a cultural paradigm shift.
MultiCare recognized up front the importance of data and analytics to effectively drive performance and quality improvement. The organization therefore designed and deployed a specific model for its Collaboratives that accommodated the intersection of traditional performance improvement and technology-enabled analytics. Key characteristics of the model included the following:
As it developed its Collaboratives, MultiCare also embarked on a business intelligence development strategy in partnership with an expert consultant to focus on three important domains:
By working on these three areas, the Collaboratives became not only the engine driving the CIN, but also the mechanism for integrating technology, standards, and clinical improvement throughout the health system. This made them a key factor in the success of the business intelligence strategy. The Collaboratives quickly discovered that without data it was nearly impossible to know where to focus efforts in order to drive improvement and where to refocus effort if performance slipped.
In fact, MultiCare credits ready access to data as the fundamental driver for successfully implementing evidence-based practice through the Collaboratives. The ability to engage the physicians with data and results that were readily available, reliable, and relevant—and then show them the impact on outcomes of their improvement efforts—proved very effective in driving adoption. Having an EDW with advanced analytics made this possible. It supplied the Collaboratives with the data they needed to identify opportunities for improvement, measure the impact of interventions, and see results quickly (see Figure 2).
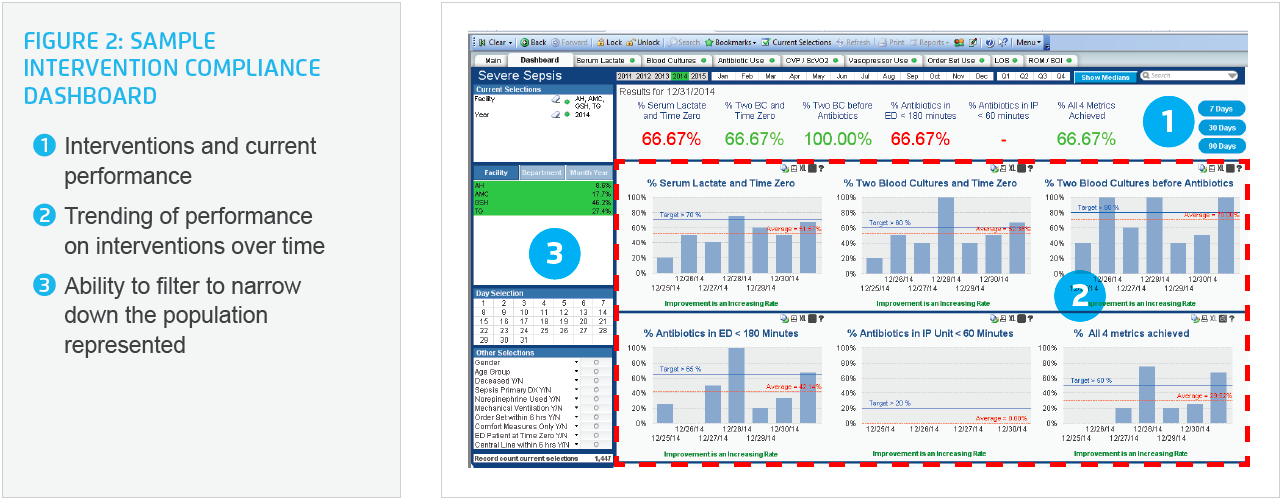
With insights provided by the EDW, the Collaboratives became adept at identifying changes in documentation that would increase structured data elements and subsequently improve strategic insight and results trending. Due to the work of the Collaboratives, there is now an ever-increasing amount of standardized data to pull from and drive advanced analytic applications. Instead of asking analysts to do manual chart audits and run reports to get the answer to a question, the Collaboratives now use advanced analytics applications to readily view the information themselves.
As MultiCare’s leaders gained experience in successfully organizing and resourcing Collaboratives, they also aligned the objectives of the Collaboratives with the strategic plan of the health system. As such, the Collaboratives were tasked with accomplishing the following:
Strong physician leadership in partnership with other clinicians was absolutely essential if the Collaboratives were to deliver on that set of objectives. Engagement of clinical operations and nursing was also critical, particularly given the level of coordination and education of providers and patients that was involved in spreading best practices across the care continuum. To achieve this partnership, MultiCare structured the leadership of each collaborative to include a physician champion, a strong representative from operations, and a dedicated program manager.
Aligning with organizational goals and using data to drive its prioritization process, MultiCare determined that it could support six active Collaboratives in 2014: Critical Care, Women’s, Surgery, Medicine, Cardiac, and Pediatric. Within each collaborative, active workgroups focused on particular clinical improvement areas (see Figure 3).

Each collaborative was charged with delivering the following system-wide materials for their focused patient populations:
Engaged practitioners developed evidence-based guidelines and pathways through the Collaboratives. Once developed, all care guidelines went through a standardized approval process. MultiCare instituted a single approval process for care guidelines and pathways before they are distributed to all practitioners across the system.
The ability to standardize practice and eliminate unnecessary clinical variation differentiates MultiCare from its competitors and has delivered significant results for the organization. The following are key achievements of MultiCare’s Collaboratives to date.
MultiCare’s Collaboratives successfully made the transition from being improvement projects—as they would be considered in most organizations—to an integral part of the way MultiCare does business. In fact, MultiCare’s Collaboratives now serve as the foundation of a culture of continuous improvement across the health system.
The immense effort behind MultiCare’s collaborative structure has contributed to a system-wide cost reduction trajectory of greater than $100 million over the last three years.
The health system achieved a 75 percent reduction in the time required to approve system-wide care guidelines and pathways. Instituting a central body to review guidelines and pathways reduced the approval time from six months to six weeks. This streamlined process is important not only because of administrative time saved but also because it speeds the time between the development of a guideline to improved practice at the point of care.
The work of the Collaboratives also led to high adoption of clinical best practices. For example, MultiCare achieved 92 percent utilization of the pre-op order set and 100 percent utilization of the post-op order set for elective colon surgery patients. The health system has also reached near 100 percent utilization of the standardized delivery note for obstetrics.
Empowering Collaboratives with clinical decision support and the ability to identify and monitor compliance with in-process measures led to the following clinical outcome improvements:
“We deployed a specific model in developing our Collaboratives that would accommodate the intersection of traditional quality improvement and technology-enabled analytics. The result is a structure that is physician led, evidence-based, and multidisciplinary, with dedicated resources.”
– Christopher Kodama, MD, MBA, FAAP, President, MultiCare Connected Care
Up to this time, MultiCare has focused principally on achieving clinical results, addressing such outcome measures as complication rates, readmissions, and mortality. Although the Collaboratives intend to continue to deliver improved clinical outcomes, they will also purposefully renew their focus on patient experience and cost reduction. This three-pronged approach puts MultiCare in a better position to deliver on the Triple Aim.
Furthermore, MultiCare will focus on becoming more agile and flexible in order to respond quickly to patient needs and market pressures. The need for agility is fueled by increasing pressure nationwide to adopt value-based care delivery strategies and to adapt quickly to new information, findings, and regulatory changes. For example, recent studies revealed that spine and back care are associated with a large amount of variation and waste, and the media and payers are placing this area under greater scrutiny. Although back and spine care had not risen to the top in MultiCare’s original prioritization process, the health system needed to address them in response to the media and market attention. Health system leaders will be modifying their processes to ensure that they can respond quickly to such demands.