Post-operative atrial fibrillation (POAF) occurs in up to 30 percent of all patients after cardiac surgery, increasing hospital stays and mortality risks. To standardize its approach to managing POAF, Allina Health's Minneapolis Heart Institute developed a nurse-driven management protocol using its data and analytics, which has led to enhanced physician practices, reduced costs, and improved patient outcomes through a standardized approach to POAF management.
Post-Operative Atrial Fibrillation (POAF) occurs in up to 30 percent of all patients after cardiac surgery. This serious complication increases the length of the patient’s hospital stay, and is associated with a twofold increase in the incidence of cerebral infarction and an increased risk of 30-day mortality. Timely and consistent management of POAF can prevent significant complications and help prevent death. To standardize such an approach to managing POAF, Allina Health’s Minneapolis Heart Institute created a physician committee to raise consensus on and develop a protocol for POAF management.
The committee ultimately created a nurse-driven protocol and decision support algorithm linked to the health system’s electronic health record (EHR). Additionally, it uses analytics, supported by Health Catalyst’s Late-Binding™ Enterprise Data Warehouse (EDW), to track physician ordering rate, patient outcomes, and cost. This combination of people, processes, and analytics tools has made a significant difference for Allina and its patients.
POAF occurs in up to 30 percent of patients following cardiac surgery.1 In patients undergoing cardiothoracic surgery, an incidence of 16-46 percent has been reported, depending on the specific surgery procedure and the extent of post-op monitoring.2 Studies suggest that POAF increases time in the intensive care unit (ICU) and extends the overall hospital stay. It is associated with a twofold elevation in the incidence of cerebral infarction and an increased risk of 30-day mortality.3
Timeliness and consistency of care are key to reducing the dangerous complications associated with POAF. At Allina Health, one of the foremost health systems in the Midwest, the stage was set to make these improvements. Commitments to elevate care for the cardiovascular (CV) patient were supported with various initiatives throughout the health system and community, including at Allina’s individual cardiac centers. Taking the lead to improve care for patients with POAF, the Minneapolis Heart Institute (MHI) at Allina Health Abbott Northwestern invested in people, systems, and technology that have elevated the bar for CV innovation and care.
Cardiac surgery at MHI maintains an exceptionally high level of quality and expertise. Through its emphasis on systemwide program development and continuous quality improvement, MHI identified unnecessary variation in the management of POAF. The underlying cause of this variation was a differing of opinions regarding the best approach for POAF management.
While standard practices were in place for prophylaxis of POAF, a standardized protocol covering broader management of POAF didn’t exist, nor did algorithms that could guide POAF decision making and timeliness of interventions. Instead, nurses were required to first contact the patient’s physician, informing her or him of the patient‘s condition and requesting orders for treatment. At times, physicians were involved in patient care and could not immediately respond, or they would need to engage in physician-to-physician consultations to determine the best possible treatment. Both scenarios involved paging, phone calls, and a somewhat lengthy communication process. Aware that POAF increases LOS and increases the complications the patient experiences, MHI was determined to ensure timely and consistent management of POAF.
MHI identified several key elements for creating an effective Post Op Afib protocol. First and foremost, physicians should reach a consensus on a standard approach that would eliminate delays in care, support appropriate use of resources, and of course, improve outcomes. To achieve and sustain these objectives, MHI followed a data-informed implementation plan designed to validate adoption and measure the impact on outcomes.
As a first step in building physician consensus, MHI developed a physician stakeholder committee. Members included CV surgeons, hospitalists, and electrophysiologists, who were responsible for the development of a POAF protocol that all physicians practicing at MHI could agree to support and use. Here the committee relied on nationally recognized and evidence-based guidelines, along with members’ individual professional experience. The latter was particularly important for developing a protocol that, while evidence based, also aligned with MHI’s patient population, culture, and operational structure.
The physician stakeholder committee also made the important decision to craft the protocol as a nurse-driven protocol. This would assure immediate action—something virtually impossible when using a more traditional approach that requires the nurse notify the physician and await a return call. In a busy hospital, physicians are often engaged with other patients, but even when they aren’t, contacting them still requires a phone call, secure text, or page, which can inadvertently delay care. By creating a nurse-driven protocol aligned with the education and licensure of the RNs, the committee enabled RNs to have a tremendous impact on safety. Nurses can deliver medications and other important interventions in a timelier fashion, which is critical for helping to prevent POAF complications and patient deaths.
With this in mind, the physician stakeholder committee brought RNs who were experts in the care of CV patients into the protocol development process. These experienced professionals critiqued and revised the protocol to better align with nursing workflow, assuring that the RNs would be able to effectively utilize the protocol to provide timely care to their patients. Pharmacists, too, provided guidance on medication dosing, working with the larger team to test potential adverse events for various medication dosages. Testing various dose ranges and potential adverse events associated with different doses helped to create comfort and confidence that the protocol medication doses were safe.
MHI then leveraged a key technology investment by linking the protocol to its EHR. Now MHI had a protocol based on expert and multidisciplinary input, designed to standardize swift and superior care. The protocol incorporates a consensus-driven decision-support algorithm based on blood pressure, heart rate, and duration of Post Op Afib to guide beta blocker, antiarrhythmic, and anticoagulation therapy recommendations in real-time. To determine appropriate medication doses and interventions, RNs enter in patient data into the linked protocol in the EHR and receive real-time decision support, initiating the appropriate orders for the patient.
Leaders were aware that use of a nurse-driven protocol for the management of POAF was a substantial change in practice. Success would be critically dependent upon the right implementation approach. To that end, RNs and physicians alike were educated about the new POAF protocol. This included one-on-one peer support, classroom/group education, and training integrated into orientation sessions for new hires of RNs.
Knowing that data drives performance, leaders relied on the EDW from Health Catalyst to aggregate the necessary data for monitoring adoption and tracking cost and patient outcomes. These functions were executed in an analytics application that ran on top of the EDW platform.
As with any major change, a few physicians were initially hesitant about using the new nurse-driven POAF protocol. In the ICU, some physicians were not yet confident of the protocol content. Here again, a focus on reaching consensus paved the way forward. Physicians and RNs tested the protocol and decision support tool together. When the tool generated orders that physicians agreed were appropriate, confidence—and physician order rate—increased.
With an analytics platform in place, MHI could track incidences of POAF and physician use rate of the nurse-driven POAF protocol. Physicians were provided their individual ordering rate in comparison to their peers. Physicians who did not initially use the nurse-driven POAF protocol to manage POAF received feedback from physician leaders. These leaders met one-on-one with them to review protocol content and discuss how the protocol could have benefited the patient had it been ordered.
MHI physicians also reviewed individual cases of POAF during medical staff meetings. As the POAF protocol use rate increased, so did the availability of data that demonstrated the positive impact to patient outcomes. This, too, further increased physician confidence and rate of use.
Use of the nurse-driven protocol and decision support algorithm has achieved what Allina set out to do: improve outcomes at a substantially reduced cost. Findings clearly show that patients with POAF who are treated via the nurse-driven protocol have outcomes that are similar to patients without POAF, and are better than patients with POAF managed independent of the protocol. These better outcomes include:
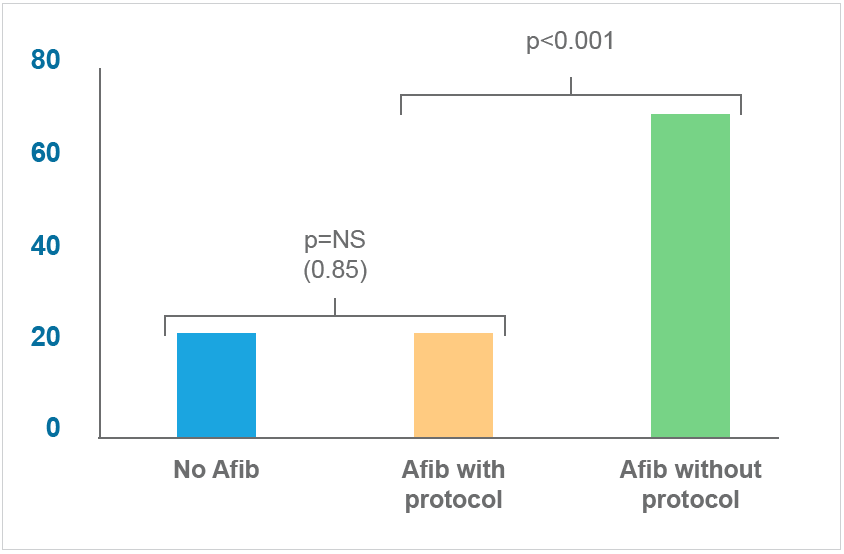

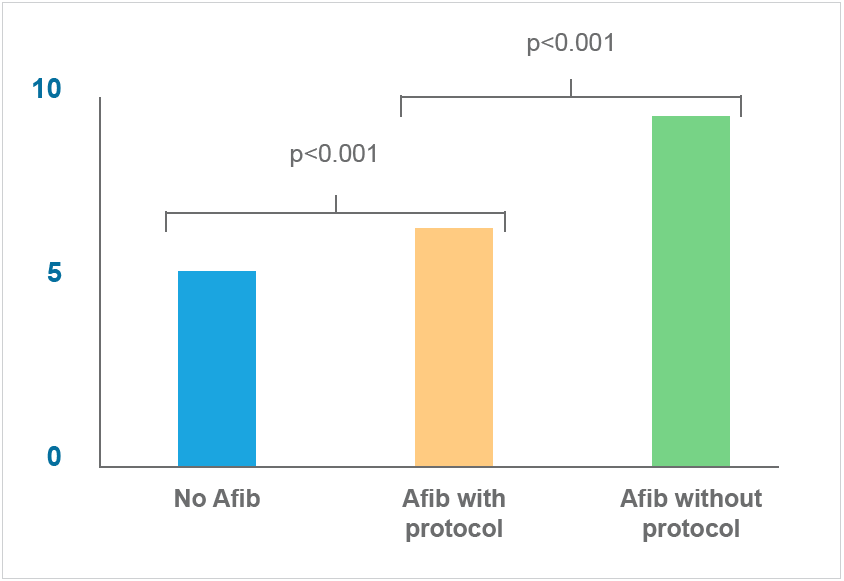

Timeliness and consistency of care have major impacts on patient outcomes. The standardized nurse-driven protocol empowers nurses to effectively manage POAF, eliminates unnecessary delays in care, and improves patient and financial outcomes.
“The decision support provided by the Post Op Afib protocol enables the nurses to do the right thing while eliminating unnecessary delays in care.”
– Dr. Raed Abdelhadi, MD, FACC, FHRS, Co-Director, Genetic Arrhythmia Clinic
MHI is committed to continuous improvement in the quality and cost of non-invasive and surgical patients for CV patients. It anticipates further increases in the use of the POAF protocol, noting that the inpatient telemetry unit has recently increased protocol use. With that, Allina Health intends to spread the use of the POAF protocol —and the associated better outcomes—throughout the health system.