Allina Health, a large integrated healthcare delivery network in Minnesota and Wisconsin, targeted cardiovascular health due to the high prevalence and mortality of cardiovascular disease (CVD). By utilizing real-time data, the organization identified clinical variations and operational issues, achieving over $75 million in savings and increased revenue over a four-year period.
Health spending in the United States is greater than the gross domestic product of most nations, and the costs for cardiovascular disease (CVD) and stroke care alone total $193.1 billion. CVD accounts for approximately one out of every three deaths in the U.S. and contributes to the shorter life expectancy of Americans. Thirty-five percent of CVD related deaths occur before the age of 75 years, and 19 percent before the age of 65.1
Allina Health, one of the foremost health systems in the Midwest, is a large integrated healthcare delivery network that includes three large cardiac centers. Due to the prevalence and mortality rate of CVD, leaders at Allina Health recognized that they needed to focus on cardiovascular health in order to truly impact the population health and patient outcomes of the communities they serve.
By leveraging real-time data from its enterprise data warehouse (EDW), Allina Health effectively identified and addressed clinical practice variation and operational issues affecting CVD care and costs. In doing so, the health system realized more than $75 million in performance enhancement savings and revenue increase over a four year period by focusing on supply chain, lab test and blood utilization, clinical practice changes and clinical documentation improvement.
Cardiovascular disease (CVD) accounts for approximately one of out every three deaths in the U.S., with 35 percent of those deaths occurring before the age of 75 years, which is younger than the current U.S. average life expectancy of 78.8 years. In addition, 19 percent of CVD-related deaths in the U.S. occur before age 65, providing a clear picture that CVD contributes to the shorter life expectancy of Americans. Cardiovascular disease treatment also comes with a hefty price tag. Nationally, health spending in the U.S. is greater than the gross domestic product of most nations, and the annual costs for CVD and stroke treatment alone total $193.1 billion.2 Despite this high level of spending, people who live in the U.S. have a life expectancy that is almost 2.5 years shorter than in other developed countries.3
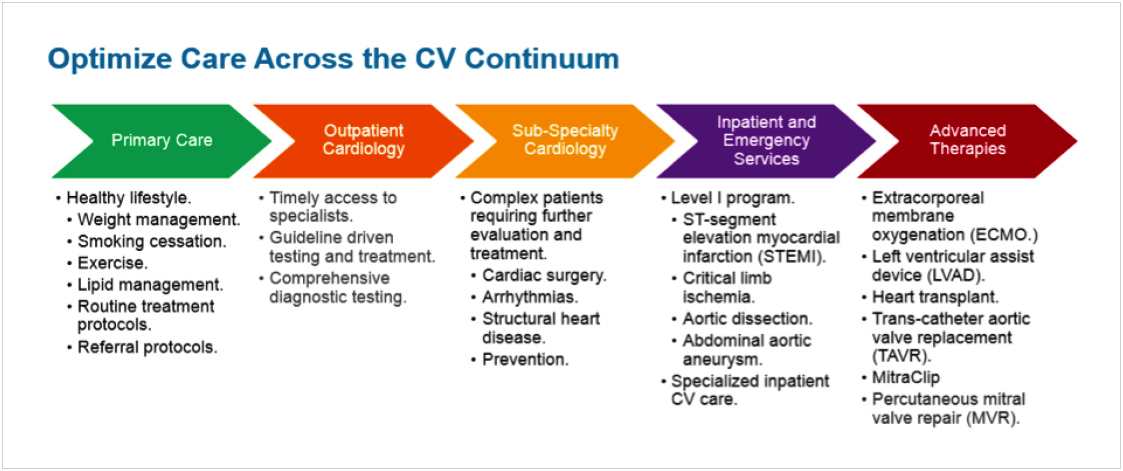
Allina Health, one of the foremost health systems in the Midwest, is a large integrated healthcare delivery network that includes three large cardiac centers. Leaders at this value-driven health system recognized that due to the prevalence and mortality rate of CVD, they needed to focus on efficient, effective CVD care in order to truly impact the population health and patient outcomes of the communities Allina Health serves. Leaders knew that in order to create meaningful change, they would need to take steps to optimize care across the entire cardiovascular (CV) continuum (see Figure 1).
Faced with the national data on the impact of CVD, Allina Health performed comprehensive research both internally and externally to define the problems and identify potential interventions. As part of that process, Allina Health leaders leveraged the robust Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture for key strategic information that enabled them to prioritize and make decisions. In analyzing internal information for clinical practice variation using analytics tools, they discovered clinical improvement opportunities related to: heart failure (HF); acute myocardial infarction (AMI); lab test utilization; community health trends; length of stay (LOS) and use of intensive care unit (ICU) beds; percutaneous cardiac intervention (PCI) and bleeding complications; blood utilization; and atrial fibrillation (A-fib) treatment.
Meanwhile, national trends in the external literature showed that costs related to electrophysiology and cardiac catheterization procedures represent a major expense driver to health system CV programs and directly link to the overall financial health of organizations associated with those programs.4 In addition, supplies are second only to labor as a source of expense, and the price of many materials has risen steeply in recent years. Furthermore, growth in non-labor costs is outpacing revenues at many hospitals, making it an imperative to better control them. Hospitals can obtain supply cost reductions of at least 10 percent to 20 percent by impacting and standardizing clinical preferences, according to studies.5
After completing this detailed analysis, Allina Health’s focus shifted from determining if and where there was a need to optimize their CV care delivery, to determining which issues to address first, and what to do about them.
Within Allina Health, ideas for improvement can come from anywhere—they can be inspired by personal experience, practices in other hospital systems, national literature, or patient feedback. The health system’s culture supports a high level of innovation and idea generation, but executing focused, systemwide efforts can be challenging.
In addition to Allina Health’s size, the health system’s complexity adds to the challenges of executing systemwide improvements. Within the 12-hospital system, all of the hospitals care for HF patients, while three hospitals perform cardiac surgery and have cardiac centers: Minneapolis Heart Institute (MHI) at Abbott Northwestern; Metropolitan Heart and Vascular Institute in Coon Rapids, Minnesota; and United Heart & Vascular Clinic with Nasseff Heart Center on the United Hospital Campus in downtown St. Paul, Minnesota. Each of the cardiology centers has different practices and treatment venues. This geographic and organizational diversity can make it challenging to gain systemwide agreement on recommendations for practice change. Other resources are systemwide. For example, all laboratory services are provided by one lab. Therefore, process changes affect all 12 hospitals and associated outpatient facilities. For supplies, there is a shared information technology (IT) system with one price file shared across the system, but several different supply contracts existed across the Allina Health system at the start of this initiative.
With all of these variables in mind, it quickly became evident that while some of the identified clinical and operational opportunities for CV Services improvement would impact all facilities, others would only impact some. Recognizing these challenges, Allina Health leaders determined that successful improvement efforts for CV Services would need to be organized and driven on a case-by-case basis because of this inherent complexity.
Whatever solution they designed would need to take into consideration which facilities were impacted and the workflows and stakeholders affected. Leaders faced these challenges head-on, with the goal of delivering on IHI’s Triple Aim to improve population health, reduce per capita costs, and improve the patient experience.
Allina Health has committed to the development of the MHI Center for Healthcare Delivery Innovation (HDI). This center for innovation positions Allina as a national leader in driving necessary change in the healthcare delivery system and supports Allina Health’s culture of continuous improvement by leveraging information and analytics to support informed decision making. When potential opportunities are identified Allina Health leaders conduct in-depth research, analysis, and planning, coupled with identifying the affected stakeholders and potential barriers to implementing change. Based on this data, the opportunities with the greatest benefit and likelihood of success were then delegated to an appropriate team of stakeholders. With these initial projects, each took on a life of its own and leaders made them successful by taking advantage of opportunities for collaboration as they arose. Allina Health’s experience had also shown that improvement efforts that have strong physician champions are the most successful. To that end, Allina Health fueled these efforts with an exceptional level of dedicated physician leadership and engaged stakeholders that believed in what they were doing to benefit patients.
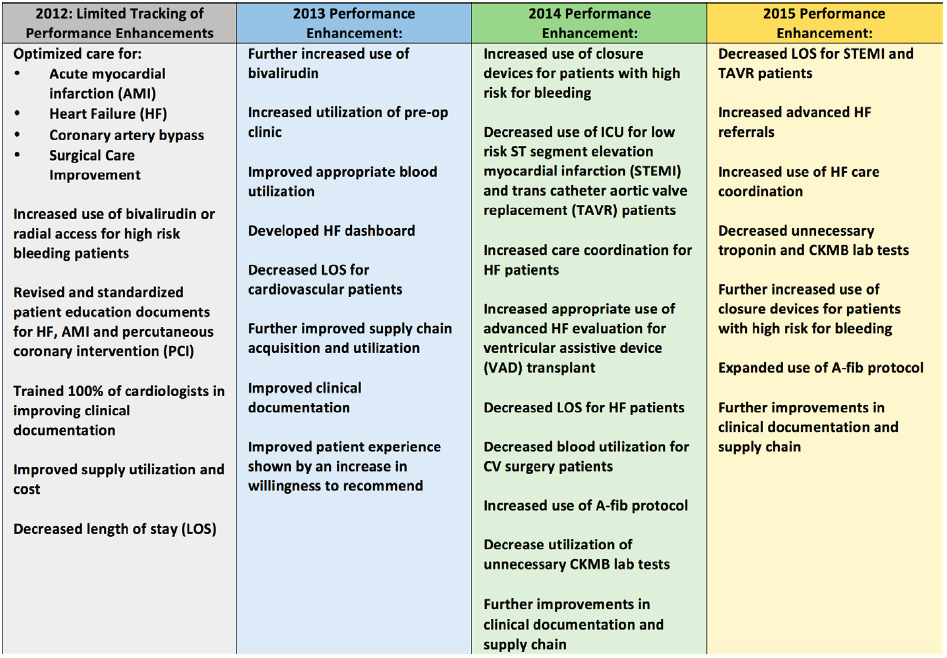
The CV performance enhancement efforts from 2012 to 2015, regardless of which stakeholders were working on them, fell into four main focus areas:
Supply Chain: Leaders identified CV supply purchasing as an improvement area that would affect all of the hospitals in the Allina Health system and that would have a high financial impact. The IT system was set up to support only one price file, a compelling reason to centralize this process. This project was led by the supply chain team, with support by a physician champion and affected stakeholders. While Allina Health had undertaken extensive supply chain work previously, traditionally the supply contracts for CV Services were bid out separately. Allina Health’s leadership believed that if they leveraged total CV supply spend across the health system with a primary vendor, they would incur cost savings. To test the theory, the supply chain team solicited bids from the four largest CV supply vendors, which, they discovered, did result in better pricing.
The supply chain team now works with all three of Allina Health’s cardiac centers together to negotiate volume pricing. This approach qualifies them for volume discounts, which is particularly advantageous for high-cost items. Executing the new contracting model required a great deal of collaboration from the three cardiac centers’ different practices and specialists. After many meetings with physician leaders, the stakeholders came to agreement and modified their purchasing practices to take advantage of combined contracting and better prices.
Overutilization and LOS: Another systemwide project focused on reducing the overutilization of laboratory tests. The entire Allina Health system is serviced by one laboratory, with one electronic health record (EHR) system and a physician order entry system. This set-up made it logical to approach this improvement at a system level. Laboratory leadership oversaw this project, and as it developed, physician champions and engaged stakeholders were recruited.
Physician champions set out to identify CV laboratory tests that Allina Health clinicians were ordering routinely at rates higher than national benchmarks. They honed in on CK-MB (creatine kinase-myocardial band) and troponin T and troponin I, which are different blood tests that indicate when there has been damage to cardiac muscle, making them useful in diagnosing cardiac conditions such as acute coronary syndrome (ACS) and acute myocardial infarction (AMI). Troponin T and troponin I start to rise at 4 to 6 hours following a cardiac event and remain high for up to two weeks. CK-MB starts to rise at 4 to 6 hours and falls to normal within 48 to 72 hours.6 When troponin tests came on the market and started to be used extensively, it made the need for CK-MB testing obsolete, with the exception of one fairly rare clinical indication (CK-MB has prognostic value post stenting, since the amount of CKMB reflects how much cardiac tissue damage occurred.) Ultimately, laboratory leaders and physician champions determined that given the emergence of troponin testing, routine ordering of CK-MB tests was no longer necessary and constituted an overutilization. In fact, their analysis found that at least 90 percent of the CK-MB testing that had been routinely performed was unnecessary. The laboratory also examined potential overuse of troponin tests. The fact that troponin levels stay consistently high for up to two weeks after a cardiac event make ongoing testing of troponin levels after the first 24 hours clinically insignificant. Therefore, any troponin tests administered after the first three, taken 8 hours apart, are considered overutilization based on the clinical evidence. The laboratory provided cardiology with clinical data and recommendations from external organizations; cardiology conducted an expert review and supported the laboratory’s recommendations that testing troponin after 24 hours constituted an overutilization.
Through discussions with CV Services and the emergency department (ED), the laboratory discovered that the ED was willing to follow cardiology recommendations related to utilization of these tests. A physician champion was assigned and a project was launched. Interventions included an education program and an ordering intervention that requests a reason/indication for testing at the time of order entry. The ordering intervention explains the reasoning behind the recommendation. After the implementation of these interventions, overutilization decreased substantially, including a 96 percent reduction in CK-MB testing and a 62 percent decrease in troponin testing after three tests have been performed in 24 hours.
Allina Health also tackled overutilization of blood and blood products. Using more blood than a patient needs for a surgical procedure exposes a patient to unnecessary risk and is not associated with better outcomes. In the spirit of reducing overutilization and improving patient outcomes, Allina developed a transfusion dashboard to assist them in monitoring alignment across their system with the Society of Thoracic Surgeons Blood Conservation guidelines. Using the most recent evidence based guidelines, provider education, and alerts in the EHR, Allina successfully reduced the number of units of blood, fresh frozen plasma, and platelets that were used during these surgical procedures.
Another aspect of overutilization that Allina Health leaders have addressed is unnecessary prolongation of an inpatient stay. By focusing on LOS reduction for CV patients, Allina Health has achieved more than $780,000 in cost savings. The health system achieved these results over several years, starting in 2012, with a focus on optimal care for patients with AMI and HF. Optimization of the patient LOS continued throughout 2013. In 2014, Allina Health reduced HF patient hospital days by 400. Leaders focused in 2015 on reducing LOS for patients with STEMI. In addition to addressing overall LOS reduction, the need to improve with STEMI, trans aortic valve replacement (TAVR), and carotid endarterectomy (CEA). These efforts not only freed up ICU beds, they also improved the continuity of care for patients, decreased overall LOS, and improved outcomes.
Clinical Practice Changes: By uncovering unnecessary clinical practice variation using analytics from its EDW, CV Services identified opportunities for practice changes with the potential for both cost savings and improved clinical outcomes. For example, care for HF patients varied greatly across the system. Leaders designed a HF management program to overcome persistent challenges with care coordination, particularly lack of a clear ownership of the HF care management process. The program focuses on five major functional areas: nursing, care coordination, protocols and guidelines, measurement and reporting, and education. Increasing advanced HF referrals has resulted in consistent, clinically appropriate, and timely care for these patients. Combining this program with an increased level of HF care coordination has reduced readmission rates and helped patients care for themselves, take their medications appropriately, and obtain follow-up care when needed.
Leaders uncovered another opportunity for patients requiring PCI, commonly known as angioplasty, which is performed at Allina Health’s three cardiac centers. Patients who undergo PCI are at risk of bleeding complications following the interventional procedure. The improvement effort kicked off as a pilot at the largest center, MHI, with the intent of eventually spreading the practices to the other centers. In retrospective analysis, as well as experience in the pilot, leaders discovered that increasing the use of closure devices for PCI patients, along with implementation of other bleeding avoidance strategies, resulted in improved clinical outcomes and decreased complications. Similarly, leaders recognized the advantages of reducing clinical variation in the care of post-op A-fib (POAF) patients, and a solution was piloted at Abbott Northwestern Hospital. The CV surgeons, in collaboration with nursing, developed and implemented a nurse-driven (POAF) protocol resulting in improved patient outcomes and a reduction in cost.
Another clinical practice change focused on educating and motivating patients to change behaviors contributing to CVD. Recognizing that many of the factors contributing to CVD are related to lifestyle (lack of exercise, poor diet, smoking, and obesity) and influenced by community and surroundings, Allina and the New Ulm Medical Center joined forces with MHI to create Hearts Beat Back: The Heart of New Ulm Project, to improve heart health through lifestyle changes at a community level. This successful program has received national recognition and serves as an aspirational model for improving population health.
Clinical Documentation Improvement: Accuracy and completeness of clinical documentation greatly impacts an organization’s ability to bill appropriately. As with many hospital systems, Allina Health recognized that millions of dollars were impacted when clinical documentation was missing that was necessary to support coding and billing at the appropriate level. In order to rectify this situation, leaders developed online training modules that physicians were required to complete. Allina Health hired RN coding documentation specialists to work one on one with the physicians to help them improve their documentation. The coding documentation specialists also performed chart reviews for specific diagnoses and identified missing documentation while patients were still in the hospital. By doing this, they were able to ensure that physicians addressed documentation deficiencies prior to patient discharge, and that documentation accurately reflected the diagnosis and the care that patient received. Allina Health’s analytics capabilities via the EDW are an important component of the clinical documentation improvement project. By analyzing comparable hospital systems in the state, leaders can identify potential coding issues, which enables timely interventions to improve the accuracy of documentation and coding for specific patient populations.
CV services attributes its wide and varied success to a unique combination of three factors:
Through their experience the past few years, leaders have learned that clinical and operational improvements yield clinically and financially beneficial results if efforts are focused on delivering on specific goals such as: improving the health of the population through adherence to clinical guidelines across the CV continuum; transforming care delivery through the reduction of clinical variation; transforming care by piloting new and creative processes and payment models; and exploring new ways to efficiently care for patients.
Allina’s efforts to improve CV Services resulted in annual savings/revenue of between $2 and $12 million, with an accumulated $75 million in savings/revenue over four years* (see Figure 2). Related successes have included:
*Note: The accumulation calculation assumes that the incremental savings for each year is repeated at the same level in each subsequent year.
“The ability to have real-time, accurate data from our enterprise data warehouse has enabled us to share physician-specific performance to help them recognize the opportunity for reducing variation.”
– Craig Strauss, MD, MPH Cardiologist, Minneapolis Heart Institute at Abbott, Northwestern Hospital Allina Health
Buoyed by their success to date in improving cardiovascular disease treatment, Allina Health’s CV leaders are dedicated to the relentless pursuit of high-quality outcomes, optimized publicly reported measures, reduced costs, increased revenue, improved patient experience, increased affordability, growth, and improved health of the community.
To leverage the potential of its largest cardiac center, Allina Health has committed to the further development of the MHI Center for Healthcare Delivery Innovation (HDI). The center will continue to expand its efforts to reduce variation through standardized CV care protocols, advanced risk-stratification tools, real-time decision support at the point of care, and innovative strategies for care delivery. The center will leverage the existing infrastructure of Allina Health’s EDW and cardiology participation in national registries to achieve the Triple Aim goals of improving population health, reducing per capita costs, and improving the patient experience across all of Allina Health.
1, 2. Mozzaffarian, D., Benjamin, E.J., Go, A.S., Arnett, D. K., Blaha, M. J.… Turner, M.B. on behalf of the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. (2016). Heart disease and stroke statistics—2016 update: A report from the American Heart Association. Circulation, 133:e38-e360. doi: 10.1161/CIR.0000000000000350
3. Squires, D., & Anderson, C. (2015). U.S. healthcare from a global perspective: Spending, use of services, prices, and health in 13 countries. The Commonwealth Fund.
4. Keast, R. K., Maxwell, S. G., Barkman, S., Chetcuti, S., Oral, H., & Eagle, K. A. (2010). Cardiovascular supply cost negotiations: partnering for the future. Health Care Management (Frederick), 29(1):68-74.
5. Lichtenberger, S., Neal, E., & Ungerman D. (2010). How sourcing excellence can lower hospital costs. Health International, 10.
6. Schrieber, D. (2015). Cardiac Markers. Medscape.