The Centers for Medicare & Medicaid Services (CMS) is tying reimbursement to hospital readmissions. Healthcare systems are investigating hospital readmissions reduction programs to improve patient outcomes and avoid CMS penalties. Learn how this healthcare system, determined to improve heart failure care for its patients, increased their documented follow-up appointments by 270 percent.
Heart failure (HF) ranks among the top 10 most expensive inpatient conditions in the United States,1 and experts expect this expense to escalate as the country’s population ages. They estimate that the prevalence of HF will increase by 25 percent — from 2.8 percent to 3.5 percent of the population — over the next 20 years. Annual direct medical costs are projected to increase from $24.7 billion to $77.7 billion.2
A not-for-profit healthcare system is committed to addressing this growing population health issue. This healthcare system has undertaken a data-driven initiative to improve the quality of HF care and reduce readmissions. This paper will outline how the healthcare system quickly established an analytics platform and team-based processes to drive impressive progress in reducing heart failure readmissions.
The healthcare system is committed to improving patient care across a variety of care process families—including cardiovascular, women and childrens, and others. As a key component of this effort, the healthcare system partnered with Health Catalyst to implement a clinical, analytic and process-based framework for value-based transformation. The healthcare system established a healthcare enterprise data warehouse (EDW) that enables an enterprise-wide, consistent view of data from the EHR and other systems. The EDW also eliminates the manual data-gathering process and automates data distribution.
One of the healthcare system’s first uses of the EDW was to prioritize its quality improvement programs. An analytics application from Health Catalyst — called the Key Process Analysis (KPA) application — analyzed the EDW data to pinpoint variability in care and areas of high resource consumption throughout the hospital. The KPA analysis revealed that cardiac services was an area of opportunity for standardizing care practices to improve quality and cost.
The decision by the healthcare system to begin its cardiac services improvement initiative by focusing on heart failure was a pragmatic one: The Centers for Medicare & Medicaid Services (CMS) is tying reimbursement to HF readmissions rates. In 2014, CMS withheld up to 2 percent of regular reimbursements for hospitals that have too many 30-day readmissions for HF. The proposed rule for 2015 would increase the maximum penalty under the program to 3 percent. The healthcare system was determined to improve HF care for its patients and avoid CMS penalties.
One of the biggest challenges the team faced was a lack of data. The healthcare system’s cardiology group had a rich data set for heart and vascular procedures and interventions; however, they did not have equivalent data for heart failure. The primary reasons for this lack of data were:
Another challenge the team faced was that they had no timely 30- or 90-day HF readmissions data available. They had numbers for overall hospital readmissions (and this information lagged by as many as 180 days), but not the readmission rate specific to heart failure. Without this important baseline, they would not be able to ascertain the impact of any intervention on HF readmissions.
Because the cardiology team was so used to rich data quality, leaders of the improvement initiative knew that clinicians would not be satisfied with a HF readmissions figure reported as a number. Clinicians would expect the ability to perform more detailed analysis — including a way to detect high risk patients with a risk stratification model.
On top of the EDW, the team implemented an analytics application that would enable them to establish readmissions baselines, track performance metrics and distribute information to everyone involved in the initiative. This Population Analytics Advanced Application- Heart Failure Module application features dashboards and visualizations that enable users to quickly and easily interpret and analyze the data.
The healthcare system also established a permanent, multi-disciplinary team to drive the HF improvement initiative. This team includes cardiologists, nurse practitioners, analysts, nurses, members of the clinical business intelligence team and a representative from billing. These team members interacted with the data, set goals, determined which best practices to implement and more. Importantly, each team member represented a group that would be affected by the improvement initiative and could speak up for that group’s needs.
With the support of Health Catalyst’s experts in clinical implementation services, the team was able to establish a comprehensive HF analytics platform in just 90 days. This rapid time-to-value was facilitated by Health Catalyst’s knowledge of how to map data from the EHR system, which enabled them to quickly locate the necessary data. Health Catalyst also led the team in an extensive data validation process to ensure that the team could trust the EDW platform as its single source of truth.
The team has now established baselines for 30- and 90-day readmission rates and an analytics platform that enables them to evaluate the impact of their quality interventions on their readmission rates. This platform includes visualizations — configured with extensive input from the multi-disciplinary team — that enable clinicians to easily understand the analytics and view trends, as shown in Figure 1.
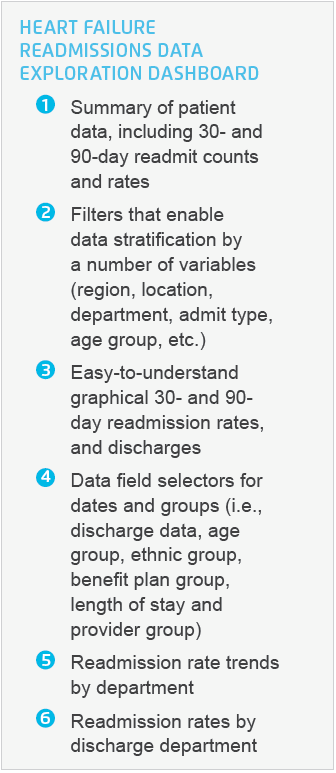

Figure 1: HF readmissions data exploration dashboard
Not only is the team now able to track their 30- and 90-day readmission rates for heart failure, they are able to do so in near real-time. Before establishing the analytics platform, they didn’t have HF-specific readmission data. The overall readmissions data they did have was as much as 180 days old, making it difficult to get timely insight into the impact of their quality interventions. This barrier to clinical improvement has now been eliminated.
The healthcare system now has an approved, consistent platform for managing and improving the HF readmission rate that is available across all the healthcare system’s regions. This means that all providers can “speak the same language” and follow the same best practice processes to reduce HF readmissions. Heart failure cohort definitions and documentation processes are consistent across the enterprise — enabling comparison across regions, units and providers. Dashboards are shared and discussed in monthly system-wide forums.
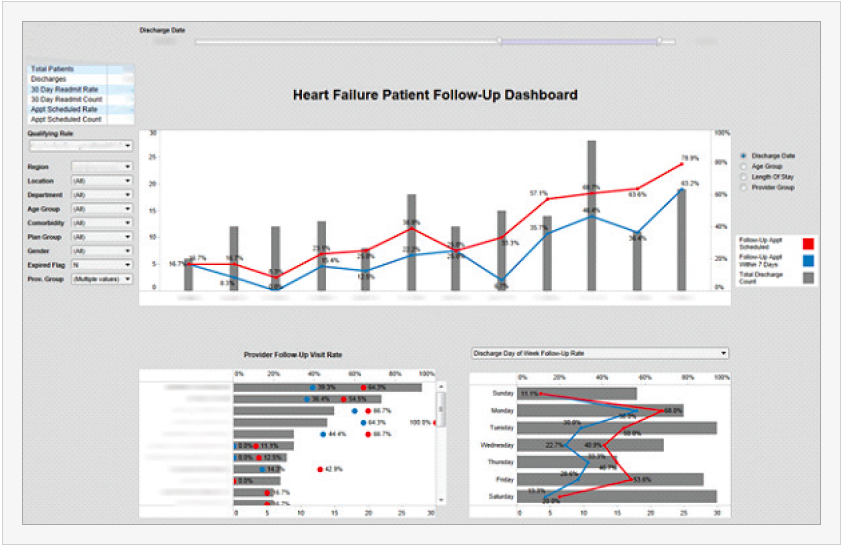
After establishing the baseline, the team chose their first intervention to help reduce readmission rates — to schedule a follow-up appointment within seven days of discharge with the appointment made before the patient is discharged. Establishing a baseline rate for this process was difficult because appointments could be documented in multiple locations, many of which were unstructured data fields. The clinical business intelligence team was able to work with the existing data to establish the baseline: 17 percent of the patients had documented follow-up appointments within seven days of discharge.
Working with Health Catalyst, the team defined a field in the EHR for documenting the appointment so that tracking appointments could be performed easily and consistently. They also worked together to provide training to clinicians. Collaborating with the clinicians and the analytics platform, the healthcare system has increased their follow- up appointments to 63 percent—a relative increase of 270 percent and an absolute increase of 46 percent — as illustrated in Figure 2.
“In the realm of cardiology, we’ve had mandates for many years now to gather data related to high-cost interventions like myocardial infarctions. We have well-established databases with clinical information about these interventions, and we have a team of analysts highly trained in evaluating that data and providing high-quality insights to our clinicians. But heart failure was different. We simply didn’t have data about heart failure.
As we kicked off this project, we knew that one of our challenges would be delivering to clinicians the level of sophistication and quality in the data that they’ve become used to. One of our great successes is that we’ve been able to achieve that goal—and to do so very quickly.”
– Cardiologist
The team will continue to measure and assess the impact of its quality interventions on 30- and 90-day readmissions. They will implement additional interventions, as necessary, to continuously improve the HF readmission rate. Potential interventions include pre-discharge medication reconciliation and post-discharge phone calls.
One of the healthcare system’s most important initiatives for managing their heart failure population will be the introduction of a HF risk stratification model. Health Catalyst and the team researched several existing HF risk stratification models, including the Acute Decompensated Heart Failure National Registry (ADHERE). They found that the existing tools were very good at predicating mortality scores; however, they were not as good when it came to predicting readmission rates. In addition, most of the tools were used at discharge and data was manually entered into the system.
The team wanted to rely on admissions — rather than discharge — data so that clinicians could receive an indication and make interventions while the patient, specifically those at highest risk, was in the hospital. The team is currently validating the model. Once the model is validated, they will develop a process for rolling it out system-wide.