Advancing women’s health is a key part of the nation’s healthcare quality improvement and population health management agenda. Mission Health has embarked on a journey to standardize its best practices and develop a more systematic method for collecting and analyzing data related to perinatal care. With an EDW serving as its analytics platform, and a newly implemented clinical improvement model, Mission is able to monitor performance on several evidence-based practices designed to improve maternal and newborn care.
Advancing women’s health, including addressing quality and safety issues related to labor and delivery, is a key part of the nation’s healthcare quality improvement agenda. Mission Health, North Carolina’s sixth-largest health system, recently embarked on a campaign to improve overall perinatal care including the appropriate use of, and supporting documentation for cesarean sections (C-sections). It has implemented an improvement program to assure that the use of C-sections adheres with emerging national best-practice standards, and supports reporting requirements. This campaign is an important component of the organization’s overall clinical improvement initiative,1 designed to promote standardization and eliminate unnecessary variation through the use of evidence based protocols and data-driven process improvement.
Like all healthcare providers in an industry moving toward value-based care, Mission needed to improve quality, reduce harm, manage complexity, eliminate waste, and operate more efficiently. Among the organization’s priorities were improving the quality, safety, and cost of labor and delivery care, including the appropriate use of, and supporting documentation for C-sections.
However, poor data quality and availability had previously restricted Mission from designing comprehensive performance improvement initiatives to address labor and delivery improvement opportunities. The process for acquiring data, validating it, and then creating reports was highly manual and inefficient.
To effectively implement and sustain labor and delivery improvement initiatives, the Mission team knew they needed to first create a more systematic method of collecting and analyzing data. They would also need tools for tracking compliance with standard evidence-based labor and delivery protocols.
Mission Health had already begun developing and implementing an initiative for optimizing care delivery processes system-wide, across the full continuum of care.2 Two key components of this initiative included:
Mission decided to apply a similar approach to improving its women’s population health. The team began by developing a C-section CPM that outlines specific tasks and metrics for the delivery process. These elements span the patient’s journey from pre-admission through hospital discharge. The CPM also includes tracking of multidisciplinary care metrics such as:
Mission then implemented an analytics application on the EDW platform to support perinatal performance improvement. This labor and delivery analytics application enables the team to identify opportunities for improvement in perinatal care across the system.
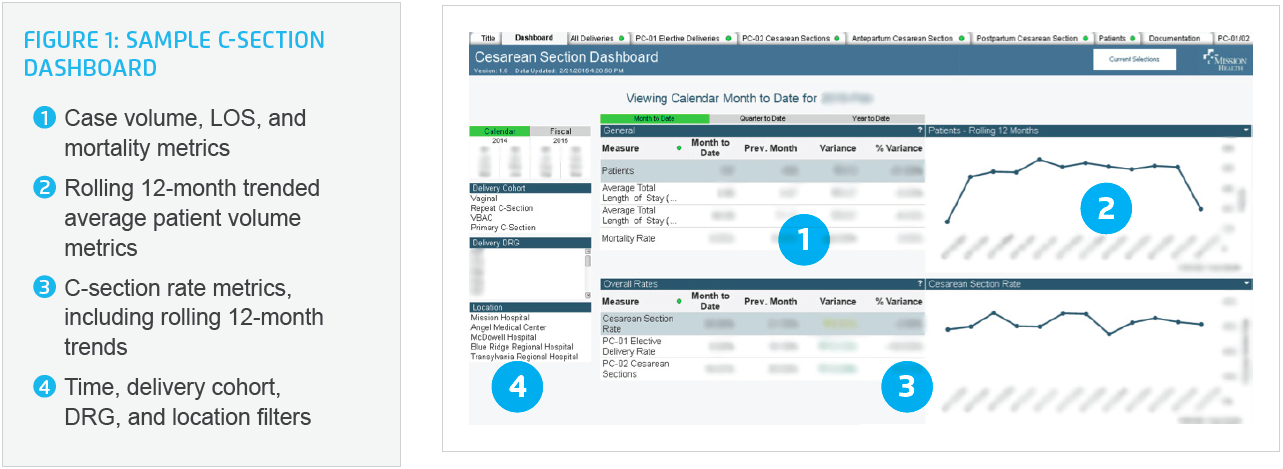
The application’s visualizations provide summary views and trends as well as drill-down capabilities to filter into greater detail on individual metrics. For example, the C-Section dashboard (see Figure 1)delivers an at-a-glance view in near real-time of key perinatal care metrics for a given time period including number of deliveries, C-section rates, length of stay (LOS) and mortality—all of which can be filtered by delivery cohort, DRG, and location.
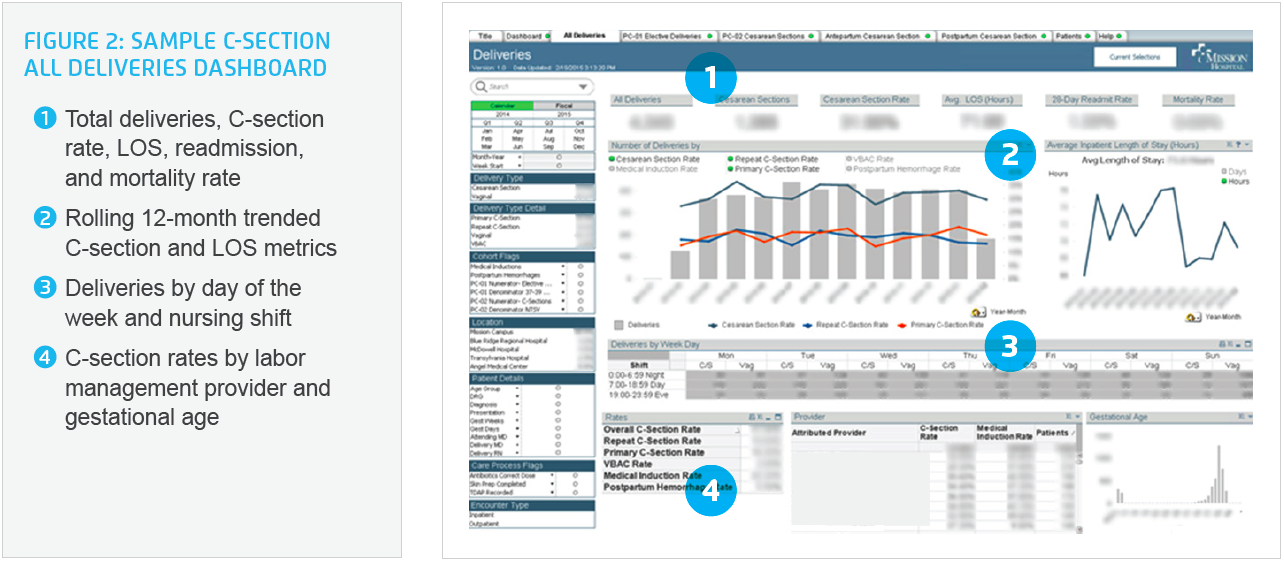
Similarly, the All Deliveries dashboard page (see Figure 2) provides an at-a-glance view of more specific delivery metrics for a given time period, including deliveries by shift and time of day to assist staff scheduling and C-section rates by patient risk factors such as gestational age at birth, and primary versus repeat C-section, C-section rates, LOS, readmission, and mortality. Time-series visualizations serve as a gauge as to whether metrics are moving in the right direction. The team is able to filter by delivery type, induction, patient demographics and risk factors, labor management provider group, and hospital location. With this information, the team can, among other things, monitor the perinatal care core measure for deliveries less than 39 weeks.
The following are the top results achieved to date through Mission’s perinatal care improvement initiative.
Mission Health has successfully implemented a clinical improvement model for labor and delivery—as it now has for several clinical programs throughout the enterprise. This model features strong senior leadership, a sound, data-driven improvement methodology, engaged care providers, ready access to highly reliable information, and a high degree of standardization with the ability for clinicians to vary care when appropriate.
Deployment of analytics tools for labor and delivery provides detailed visibility into the operations of one of Mission’s most strategic service lines. Drill-down and data visualization capabilities have enabled leaders to identify important trends and potential opportunities for improvement as well as hold caregivers accountable for adhering to evidenced-based practice.
The application is currently rolled out among “super user” clinicians who monitor the data and share feedback with the broader group of caregivers at Mission. As the C-section CPM is implemented across the entire health system, the super users have begun to vet the new evidence-based protocols with other labor and delivery clinicians. They report an enthusiastic response to the protocols, suggesting the potential for smooth clinician engagement as the initiative rolls out more broadly.
With this infrastructure in place, Mission is well positioned to track and improve compliance with emerging state and national best practice guidelines and quality metrics. The team is able to manage reporting requirements with minimal manual work and to rapidly initiate performance improvement strategies, when needed, in order to meet regulatory or contractual requirements—including a multi-million dollar contract currently in place. A key perinatal quality measure from The Joint Commission, Mission has sustained a zero early elective delivery rate through the 2015 calendar year to date.
Mission’s EDW infrastructure is alleviating the data timeliness, completeness, and quality concerns that had hampered previous initiatives to improve labor and delivery care. It is also significantly reducing the time spent manually collecting data and performing rate calculations. With the automation of data acquisition and robust visualizations, Mission anticipates a potential 20 percent-plus time savings of one equivalent FTE per month.
“Our ultimate goal is to use the analytics application to improve clinical care and operational performance system-wide. We are very excited about rolling out this wonderful tool more broadly among clinicians and staff. So far our clinicians have seen what we are doing to improve care and have given us very positive feedback.”
– Shannon Jaquess, Quality Improvement Advisor, Mission Health
Mission has begun to roll out the C-section CPMs and the labor and delivery advanced analytics application more broadly across the organization. The team will continue its efforts to engage clinicians and implement multidisciplinary collaboration. An important part of this effort will involve using data to increase transparency and thus drive further engagement and cultural change. Involvement of labor management providers has already built a level of trust that can be leveraged in the future as Mission focuses on improving labor and delivery care, including achieving the optimal NTSV (nulliparous, term singleton, vertex) C-section rate as national best practices are delineated. As its evidence-based processes mature, Mission plans to enrich the data set and implement new improvement initiatives by automating the acquisition of additional perinatal data elements.
The focus on labor and delivery is just one piece of Mission Health’s overall improvement strategy. Mission will continue to roll out its clinical program improvement initiative to other service lines, such as children’s, orthopedics, neurosciences/spine, and surgery/trauma. The organization will continue to expand its analytics capability by adding analytics applications running on the EDW platform to support quality improvement, utilization, and cost-reduction initiatives.
1,2. Clinical programs: Managing care across the continuum. (2015, January 7).