Colorectal cancer (CRC) accounts for $16 billion in healthcare costs and is the second leading cause of cancer deaths in the U.S. Thibodaux Regional Health System adopted evidence-based screening and treatment guidelines for colon cancer. However, it still needed to meet organizational goals for early diagnosis and colon cancer survival. By leveraging analytics for accurate data, the organization improved CRC outcomes and patient satisfaction.
Colorectal cancer (CRC) accounts for $16 billion in healthcare costs, and with 142,250 new cases annually, it’s the second leading cause of cancer deaths in the U.S. Healthcare organizations are striving to reach a win-win scenario with CRC—to save more lives with CRC prevention and detection and save billions of dollars at the same time.
Thibodaux Regional Health System had implemented evidence-based screening and oncology treatment guidelines for colon cancer, yet it still needed to meet organizational goals for early diagnosis and colon cancer survival. With support from the CEO and senior executive leadership, a collaborative approach to tackling CRC diagnosis rates, and a robust suite of analytics applications to deliver accurate data, Thibodaux Regional improved CRC outcomes and patient satisfaction.
Colorectal cancer (CRC) is the second leading cause of cancer deaths in the U.S., accounting for $16 billion in healthcare costs and 142,250 new cases annually. Sixty percent of deaths from colorectal cancer can be avoided with early screening to facilitate early treatment.1,2
Thibodaux Regional Health System, a nationally recognized medical center, is committed to providing high-quality, cost effective, comprehensive services.
Despite having implemented evidence-based screening and oncology treatment guidelines for CRC, Thibodaux Regional was not meeting organizational goals. The hospital lacked a standardized approach to facilitate the early detection of CRC, which caused a delay in diagnosis and treatment and increased the number of patients diagnosed with an advanced stage of CRC.
There were no standardized processes for CRC perioperative care, which extended the length of stay (LOS) and increased costs. Thibodaux Regional lacked actionable data it could use to focus on CRC prevalence and screening rates, operating room (OR) efficiency, and perioperative practices that optimize recovery after surgery.
Thibodaux Regional needed a comprehensive, data-driven approach to improve early screening, reduce perioperative costs, and improve survival rates.
With the support of the CEO and senior executive leadership, Thibodaux Regional established a colon care transformation team—an interdisciplinary team responsible for developing and implementing a CRC improvement plan.
Thibodaux Regional utilized the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications, including the Colorectal Surgery Analytics Accelerator, to monitor and analyze CRC screening and care, identifying specific opportunities to improve CRC clinical outcomes and reduce CRC care costs.
The Colorectal Surgery Analytics Accelerator provides data focused on colon cancer prevalence and screening rates, OR efficiencies, and perioperative practices that optimize recovery after surgery (see Figure 1).
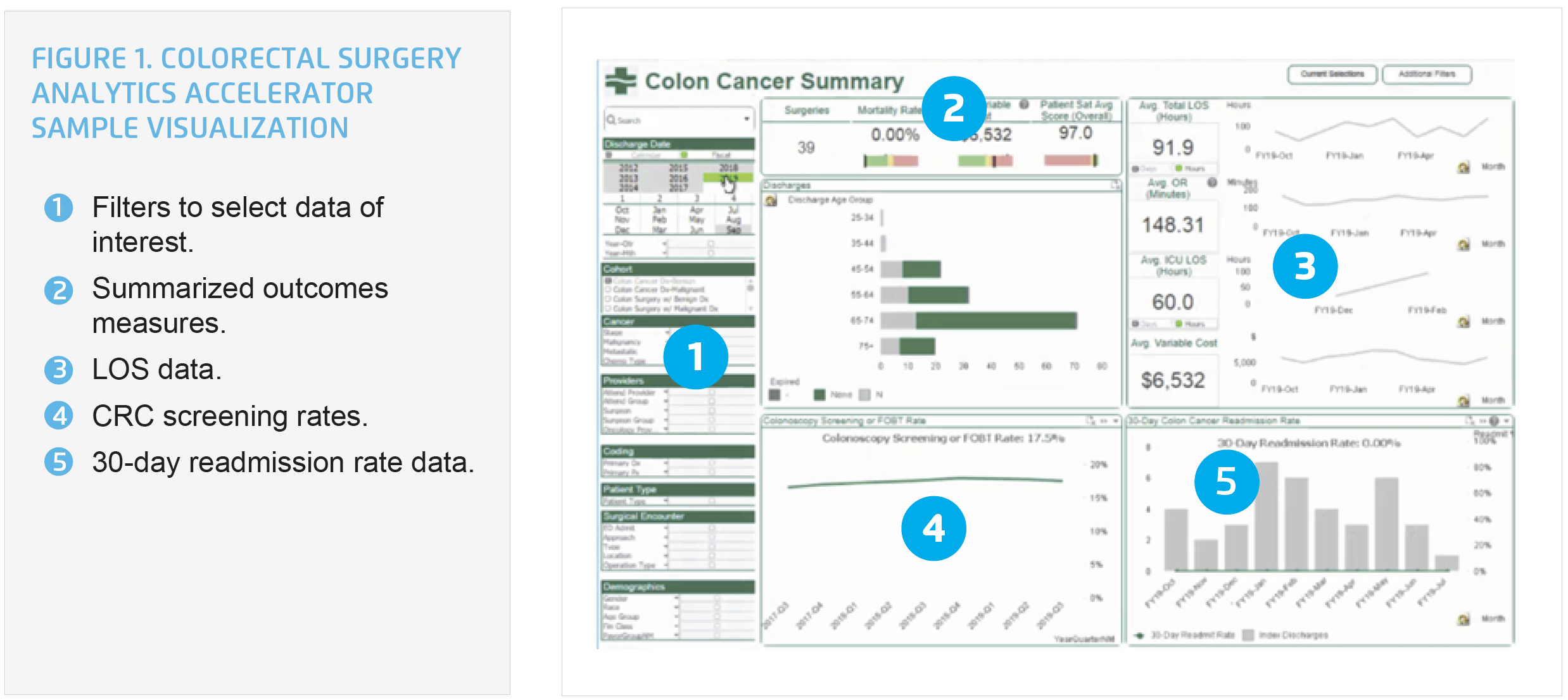
Using data from the analytics accelerator, Thibodaux Regional identified variability across CRC screening, inpatient care processes impacting perioperative care, and mortality rates. With that data, it subsequently prioritized its improvement efforts, focusing on improving initial CRC screening to increase survival rates and standardizing CRC care to improve patient outcomes.
To gain insight into the community population, physician leaders retrospectively analyzed colonoscopies for pathology, staging at time of diagnosis, and lymph node recovery rates (identifying the opportunity to improve lymph node recovery rates). Medical oncologists, pathologists, general and specialty physicians, and frontline nursing staff took ownership of the CRC improvement work.
To improve early screening and aid in the reduction of CRC, physician leaders provided education throughout the community and incorporated questions regarding recent screenings into the hospital’s admission questionnaire. They also developed educational materials addressing risk factors, such as smoking and sedentary lifestyle, and provided CRC screening and treatment options to patients.
Thibodaux Regional incorporated process changes to optimize recovery for patients undergoing CRC surgery, implementing enhanced recovery after surgery (ERAS) protocols and embedding the ERAS standards in its pre-, intra-, and postoperative workflows and associated order sets. Thibodaux Regional also optimized the process changes, order sets, screening, and educational materials by aligning them with physician and staff workflow.
The workflows include best practices and evidence-based standards for the following:
Thibodaux Regional leverages the analytics accelerator to monitor performance for both process and outcome measures, including protocol compliance, LOS, variable costs, 30-day readmission rate, postoperative complications, and mortality rate. It can now review data in aggregate or can drill down to view individual patient-, unit-, or provider-level performance data.
The colon care transformation team uses data from the analytics accelerator to drive unified care, identify opportunities for improvement, and identify success, providing the staff and physicians with regular feedback about performance to clearly link the impact of interventions to patient outcomes.
Thibodaux Regional’s data-driven CRC improvement efforts have raised the consistency and quality of care it provides to its patients, positively impacting clinical outcomes, and patient satisfaction.
“Having a team approach is key—everybody’s input matters. From bedside nursing to the physician to pathology, to be successful requires a team approach.”
– Ashley Becnel, RN, LSSGB, Quality Improvement Coordinator, Thibodaux Regional Health System
Thibodaux Regional will continue to use a data-driven approach to improve the care it provides to patients. The organization plans to use the analytics accelerator to evaluate the impact of specific interventions on patient outcomes and will use the data to further improve outcomes for patients with CRC.