UnityPoint Health identified that over 10 percent of inpatients received red blood cell (RBC) transfusions annually, costing over $12 million. A task force was formed to enhance blood management and establish best practices. It implemented decision support tools for transfusion ordering and used an analytics platform to monitor blood product utilization and predict needs. UnityPoint Health’s data-driven improvements in blood management have reduced unnecessary RBC transfusions and enhanced patient safety.
UnityPoint Health recognized that more than 10 percent of its inpatients received red blood cell (RBC) transfusions annually, at the expense of more than $12 million each year. The organization created a task force to develop and implement a plan for maximizing blood management, plus establishing best practices.
To support this initiative, the task force incorporated decision support to improve transfusion ordering in alignment with the transfusion standards. An analytics platform has also been leveraged, which monitors the utilization of blood products, including predictive modeling to risk-adjust blood utilization specific to patient case-mix, and data down to the ordering provider level.
Across the country, 14 million units of RBCs are transfused annually. An average of three units are used per transfusion, at the cost of $300 per unit.1,2 RBC transfusion can be life-saving, although sometimes it can also cause harm. This treatment is strongly associated with prolonged hospital stays as well as increased costs, morbidity, and early and late mortality.3
UnityPoint Health is committed to providing outstanding care across Iowa, western Illinois, and southern Wisconsin. Its network includes hospitals, clinics, and home care services, with over 6.2 million annual patient visits, providing a full range of care to patients and families using innovative advancements to deliver the best outcome for every patient, every time.
UnityPoint Health recognized that more than 10 percent of its inpatients received transfusions annually, costing the organization more than $12 million each year. One critical initiative identified to improve the quality of care and safety of RBC transfusion, and reduce cost, was blood management. These improvement efforts were hindered, however, by a lack of specific, actionable data, to generate insight into blood management improvement opportunities.
The organization needed a comprehensive, data-driven approach to improve the effectiveness of blood management. It also worked toward decreasing unwarranted variation to improve patient safety, conserve a valuable, limited resource, and drive down costs.
To improve blood management, UnityPoint Health created a task force, directing the team to develop and implement a plan to maximize blood management. The task force was instructed to establish a culture promoting best blood management practices and non-punitive process improvement.
UnityPoint Health focused its improvement efforts on engaging providers in transitioning to the American Association of Blood Bank (AABB) transfusion standards, and implementing decision support to improve transfusion ordering in alignment with the transfusion standards. The organization implemented:
UnityPoint Health provided its interdisciplinary team education, increasing awareness of the risks of blood transfusions, the changes in related guidelines compared to what many were taught during medical or nursing school, and the improved patient outcomes associated with the AABB guidelines. The organization also leverages the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications for its data and analytics needs, and uses the Blood Utilization Analytics Accelerator to monitor the utilization of blood products, including data down to the ordering provider level (see Figure 1).

The analytics accelerator is designed to monitor the effectiveness of UnityPoint Health’s blood management initiatives, and uses both historical descriptive statistics, and predictive modeling to risk-adjust blood utilization specific to patient case-mix.
The risk-adjustment model includes consideration of:
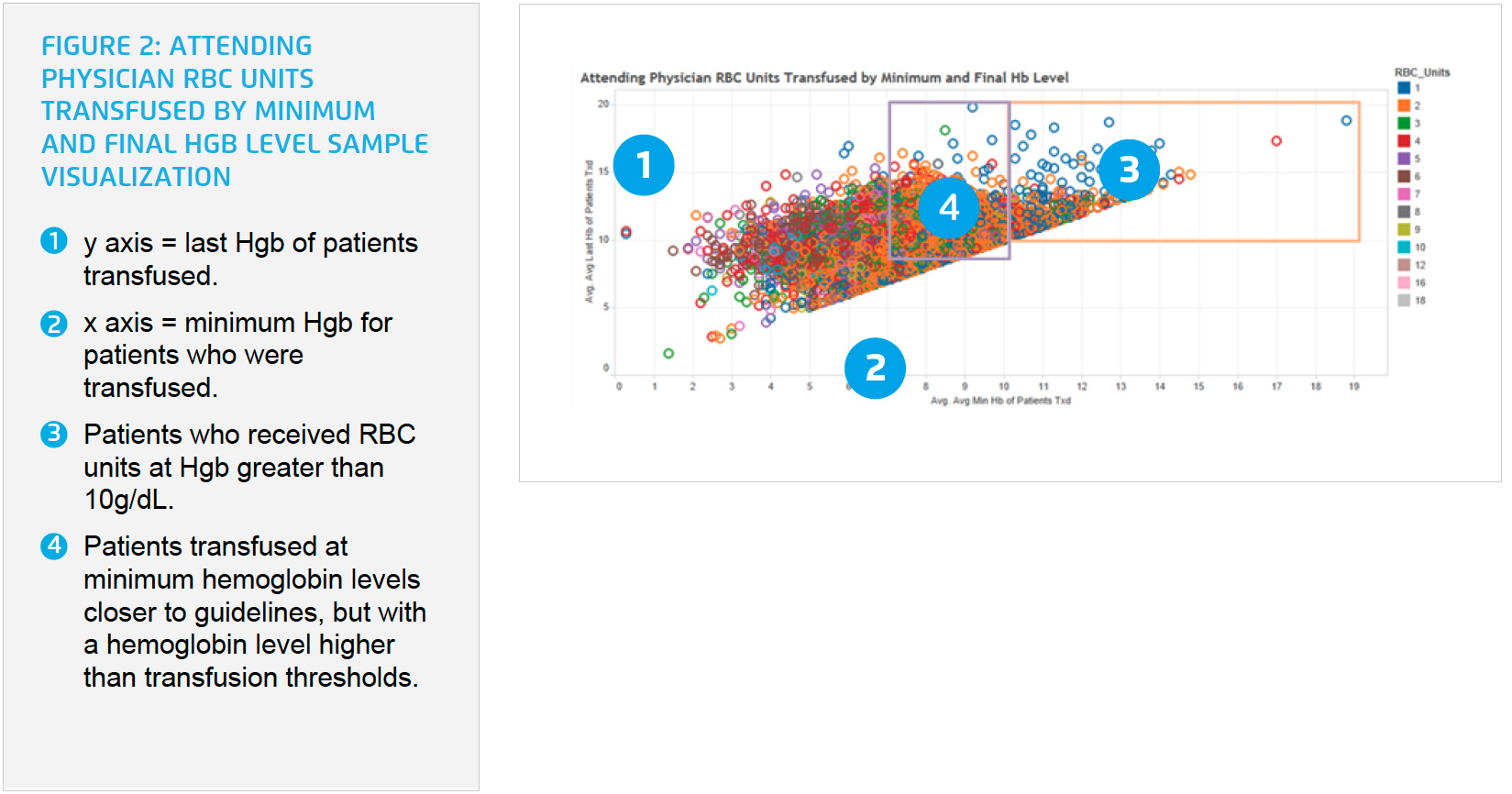
Using the risk-adjusted data in the analytics accelerator, UnityPoint Health is able to visualize utilization of RBCs, and is able to attribute variation in RBC transfusion to patient factors that necessitate higher utilization, or to variation in provider practice. The organization is then able to control for deviation in patient factors and isolate variation in provider practice to identify potential over-utilization of RBCs. Transfusion scenarios that may not have been appropriate can easily be identified and visualized. It can visualize patients who were transfused at Hgb levels far above the current guidelines, and also identify patients who were transfused at minimum Hgb closer to guidelines, but with a last Hgb that was much higher than transfusion thresholds (see Figure 2).
UnityPoint Health leaders can use the analytics accelerator to review individual patient cases that were transfused with RBCs without logging into the EMR. The data can be filtered by ordering provider, so all patients that contributed to a particular actual/ expected ratio can be viewed in one location.
The analytics accelerator data are updated monthly and available for hospital transfusion reviewers and providers giving them the ability to compare their transfusion performance with their peers. Leaders engage with providers to understand cases of overuse, identifying if the use was appropriate, and if not, working with the provider to change practices and adhere to the transfusion guidelines and most recent best practices, safeguarding the best possible patient outcome.
UnityPoint Health’s data-driven patient blood management improvements have helped improve patient safety by decreasing unnecessary RBC transfusion, ensuring patients receive care aligned with the most recent evidence. These efforts have also positively impacted financial performance across the system, including:
“The success of the UnityPoint Health blood management program reflects our commitment to continually improving patient safety while ensuring the best outcome for every patient.”
– Michael Kafka, MD, FACP Medical Director, Quality and Patient Safety
UnityPoint Health plans to expand its use of predictive analytics to continue improving the care it provides patients.