U.S. healthcare is shifting from procedure and visit approaches to a longitudinal view of patient care, supported by the Centers for Medicare & Medicaid Services’ “Bundled Payments for Care Improvement Initiative.” This initiative holds healthcare organizations accountable for 48 episodes of care, requiring the integration of diverse data sources to manage costs and variations. Mass General Brigham (formerly Partners HealthCare) successfully integrated hospital, provider, and claims information, enabling evaluation and comparison of clinical and financial performance.
For population health management to be meaningfully implemented, accountable care organizations must have access to information about the full scope of services provided to their patients, including cost and outcomes of care. Broader views of certain patient cohorts are also increasingly important. Healthcare organizations need to understand which cohorts drive the margins, costs and service utilization of their institutions in order to align resources with the appropriate patient services.
There is currently an active effort in the U.S. to shift healthcare from a procedure or visit focus to a longitudinal view of patient care grouped according to logical episodes that encompass all the major care delivered to a patient for a condition or related to a procedure. The Centers for Medicare & Medicaid Services (CMS) launched a “Bundled Payments for Care Improvement Initiative” to support this shift in approach. Under this program, participating organizations enter into payment arrangements that include financial and performance accountability for 48 episodes of care as defined by one of four models. The program has far-reaching implications, even for non-participating organizations like Mass General Brigham (formerly Partners HealthCare), New England’s largest health system.
As a delivery system long focused on care for conditions across inpatient, ambulatory and post-acute settings, Mass General Brigham recognized the value of looking at costs, margins and service utilization organized by episodes of care as defined under the Bundled Payments for Care Improvement Initiative Model 21. In this model, an episode of care includes all of the services a patient receives for a certain health event, beginning with a qualifying inpatient admission and ending 30, 60 or 90 days after discharge2. This approach also aligned well with a comprehensive set of tactics Mass General Brigham created to address population health, value-based purchasing and accountable care.
Along these lines, Mass General Brigham determined that developing a consistent and standard way to evaluate the clinical and financial performance for specific patient cohorts, such as those inherent in the 48 episodes of care, would provide key strategic information for making decisions. Mass General Brigham could use the data to identify promising opportunities to improve care delivery and outcomes, while reducing cost and waste.
To inform these decisions, Mass General Brigham required a solution that showed the cost and utilization of all aspects of care related to a particular clinical event, whether the care was provided within Mass General Brigham or outside of it. However, these deeply insightful views could only be possible by merging data from the hospital, providers, and patient claims—a combination that Mass General Brigham had not yet successfully integrated.
Data validity was a particularly important consideration. Mass General Brigham needed to be able to structure inquiries and analysis around consistent, standard clinical categories. It needed an easy way to consistently visualize relative performance of different groups of patients in two dimensions, cost and variation, and to look at different views of the same data—such as looking at costs, margins and utilization by provider, payer or sites of care. Most importantly, users had to trust the data they were seeing, and be willing to use it to identify areas of focus for clinical, financial, and operational performance improvement.
Mass General Brigham determined an advanced analytics solution was needed, particularly one that users could quickly learn to access and trust. To that end, Mass General Brigham worked with Health Catalyst to define an advanced analytics solution for providing the desired metrics and episodes analytics. To shorten the time to value, Mass General Brigham decided to base the application on the definitions and inclusion and exclusion criteria from the CMS 48 Episodes of Care as defined in Model 2, rather than defining their own groupers, and leveraged their existing development and deployment methodology.
For this particular analytics solution to be effective, it was critically important that prior to application design stakeholders identify what questions they would be asking about episodes of care, costs, margins, variation and utilization. Accordingly, Mass General Brigham brought together a group of engaged stakeholders to study different clinical and business use cases, and determine the appropriate analytic paths to the desired insights. By performing this detailed analysis of use cases using analytic paths prior to designing the application, developers were sure that the end product produced the desired stakeholder results.
These efforts also identified which databases and data sources should be integrated to provide the right information. In one use case analysis, for example, it became evident that plotting episodes of care against cost and the coefficient of variation was a key strategic visualization to support prioritization efforts. This in turn revealed the data sources (data marts) that were needed to supply hospital, provider and claims information. A series of use cases showed that Mass General Brigham needed a combination of multiple data sources to be able to assess variation in the experience of patients across inpatient and outpatient, primary and specialty care services, and continuing care (e.g. rehab, skilled nursing facilities, home care) environments.
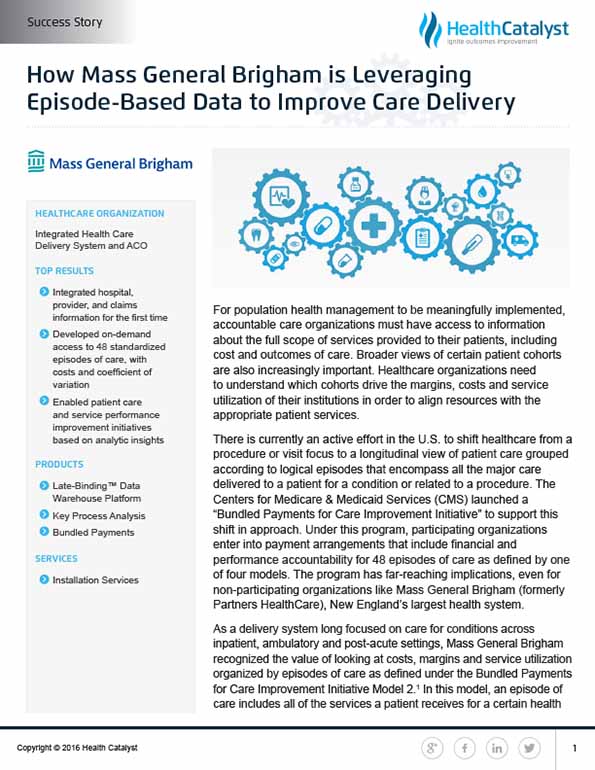
Mass General Brigham wanted the ability to look at all associated costs related to bundles/episodes, and then use this information as a foundation of decision support to optimize care delivery and resource allocation through well-focused improvement efforts. By using the Pareto approach, also known as the 80/20 rule, Mass General Brigham was able to identify the bundles/episodes that consumed the most resources and represented the greatest opportunities for cost reduction (see Figure 1). Cost is frequently a good proxy for variation in clinical practice, so identification of these opportunities frequently led to evaluation and improvement of clinical practice as well. This approach provides a visualization that is easy to use to identify opportunities for improvement at a high level.
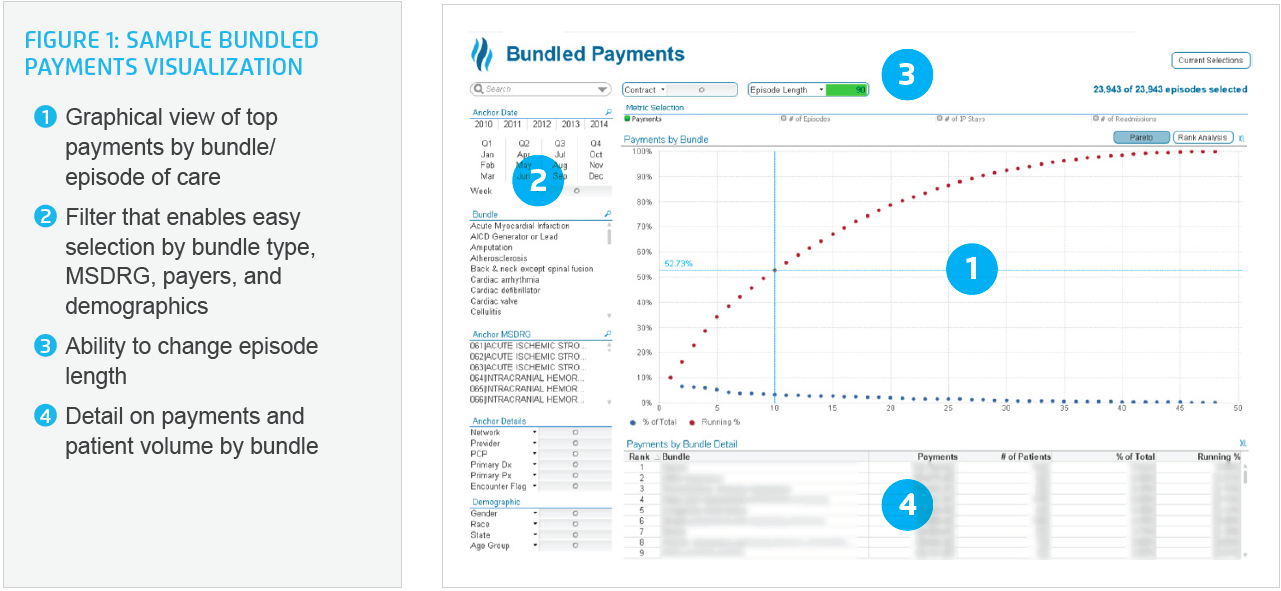
However, through the stakeholders’ use case analysis, they knew that to make well-informed decisions they also needed the ability to look deeper at specific episodes, or groups of episodes, and look at the information by payer, provider, sites of care, and at times even drill down to the patient level. To address this need, bubble chart capability was developed to allow multiple and different types of comparisons based on the filters selected. Cost is on the x-axis, and the coefficient of variation (the ratio of the standard deviation to the mean), is displayed on the Y-axis. This has become an important strategic concept for Mass General Brigham in determining the appropriate area of focus (see Figure 2). Using this visualization, bundles/episodes that are highly variable and resource-intensive are found in the chart’s upper right quadrant, making them easy to identify and further investigate.
The stakeholders also identified the need for specific financial information to guide well-informed decisions. Built into the application are graphs of the average spend per bundle across the service providers/sites of care, stratified by the service categories inpatient, outpatient, professional, additional, and others. Selecting two or more service providers allows users to compare average spend across service providers and potentially identify opportunities for improvement that could be enacted by standardizing care approaches, or the tests, supplies, and equipment used for a particular group of patients. This gives Mass General Brigham the ability to identify and eliminate unnecessary variation in the care routines of providers, while monitoring to see that patients do receive those critical best practice interventions that lead to improved outcomes.
Using the application gives Mass General Brigham the information needed to take action or drive decisions that will result in better care for patients, and thus better population health, with lower costs.
For the first time, Mass General Brigham has successfully integrated hospital, provider, and claims information—an accomplishment that’s made a broad impact on decision-making across the entire health system. The advanced analytics application pulls data from multiple data marts in a way that enables Mass General Brigham to easily compare and contrast information, while different views of the data answer questions about utilization, cost, and opportunities for improvement.
Having all of this information readily available in such a visual framework, has made it easy for Mass General Brigham to evaluate and compare clinical and financial performance for the 48 episodes of care and drill down into key business questions. Being able to view specific episodes of care graphed on the two dimensions of cost and variation has provided quick insight into their relative performance, and relative opportunity for improvement. Use of the CMS definitions to define the 48 bundles/episodes, in addition to saving development time, has paved the way for them to compare themselves to other providers, and to communicate effectively with payers.
In recognition that making good decisions requires more than just data, the health system has incorporated non-analytic aspects into their prioritization process to account for critical factors, such as the presence or absence of a strong clinical champion to drive change, or the operational implications of expanding or contracting services in a particular location.
All of these new initiatives and capabilities lay the groundwork for a data-driven culture. Indeed, Mass General Brigham can better drive patient care and service performance improvement initiatives based on these analytical insights.
“The real power of this tool was our ability to take claims, hospital billing, and physician billing data and add them all together around the patient episodes.”
- Sree Chaguturu, MD, Vice President, Population Health Management
Mass General Brigham is interested in analyzing episodes of care that CMS has not yet addressed, such as cancer bundles. While it will need to determine how to build groupers for oncology patients, an essential component of such an initiative is already in place: Mass General Brigham has excellent oncology champions.
More immediately, focus now turns to increasing adoption, implementing more improvements, and tracking outcomes and effectiveness. Mass General Brigham’s journey to a data-driven culture continues, and is well on its way to the use of advanced analytics across the entire organization.