Health systems attempt to measure an ever-increasing amount of clinical measures, these often miss the mark of what matters to patients. Patient-Reported Outcomes (PROs) are the missing link in empowering patients and helping to define good outcomes. This article walks through how patient-reported outcome measures (PROMs) can help identify best practices and drive system-wide quality improvement. PROMs can help health systems do the following:
• Serve as a guide for appropriateness and efficiency.
• Lead to better shared decision-making.
• Demonstrate value and transparency
This article also discusses the effect of PROMs on providers in a culture of “one more thing,” and tips for effective implementation.
 Download
Download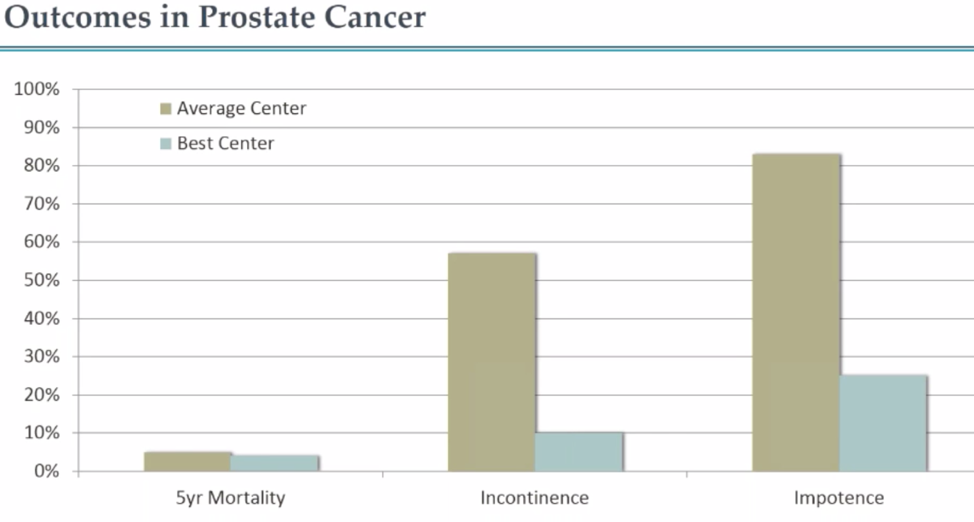
How do patients choose their doctors? This is the million-dollar question asked and explored by health systems’ executive teams and communication departments across the country. And, the answer might be different depending on who is being asked. Do patients use publicly available quality metrics, shop websites and articles, use their own personal healthcare network or PCP, ask friends and family, or use their insurance provider’s list? While these are the main choices available to consumers, each of these avenues is flawed in its own way.
One example is the personal vignette of a woman who was diagnosed with an aggressive form of breast cancer. Her friend, a cancer surgeon in a different state, vetted her available options with his oncology network. The surgeon recommended a physician with excellent outcomes, but the woman hated the physician’s bedside manner and ended up choosing a different doctor with much lower surgical outcomes than the recommended physician. If even surgeons can’t get patients–including friends and family–to the right providers, how can patients be expected to find the right provider and care for their needs? Patient-reported outcomes are the missing link in empowering patients and helping to define good outcomes.
Patient-Reported Outcomes (PROs) are defined by the National Quality Forum as “any report of the status of a patient’s health condition that comes directly from the patient, without interpretation of the patient’s response by a clinician or anyone else.” Most healthcare organizations consistently measure things like mortality rates, length of stay (LOS), readmissions, lab values, or other process measures. As clinicians and health systems seek to provide better care, they will only succeed if they can accurately define what qualifies as a good outcome.
Health systems attempt to measure an ever-increasing amount of clinical measures, these often miss the mark of what matters to patients. Not many physicians have been asked by a patient what their 30-day mortality rate is, for instance. What’s often overlooked are issues that impact a patient’s quality of life. Patients care about things like, “If I have my prostate removed, am I going to be incontinent?” or “Can I pick up my grandchild?” Patients care about symptoms, daily activities, functional status, and mental health. All these things are difficult for health systems to measure, which is where patient-reported outcome measures (PROMs) come in. PROMs provide the missing link in defining a good outcome by capturing quality of life issues that patients care about and which often cause them to seek out care in the first place.
A great example that highlights the importance of patient-reported outcome measures is extracted from a Michael Porter Harvard Business School Case Review looking at urology surgery outcomes. When comparing two hospitals, one thought to be average, one considered to be one of the best in the country, there’s very little difference in mortality, particularly with prostate cancer. Looking at the five-year mortality outcomes in Figure 1, the results are nearly identical between the two institutions. However, the second two measures show rates of incontinence and impotence, and there’s a marked difference between the two.
As a patient, of primary importance is “Am I going to live,” but the second question is, “What is my life going to be like?” This is where some outcome measures are much more important to a patient’s quality of life. If a patient knows there is a 50 percent chance of becoming incontinent or a 75 percent chance of impotence when undergoing surgery for prostate cancer, this will affect his decision-making process. Even though both institutions can keep patients alive, it’s the best center that employed techniques that have helped patients maintain a high quality of life and retain dignity and relationships. Even though these measures aren’t reported in traditional healthcare metrics, they are sometimes the ones that matter most to patients.
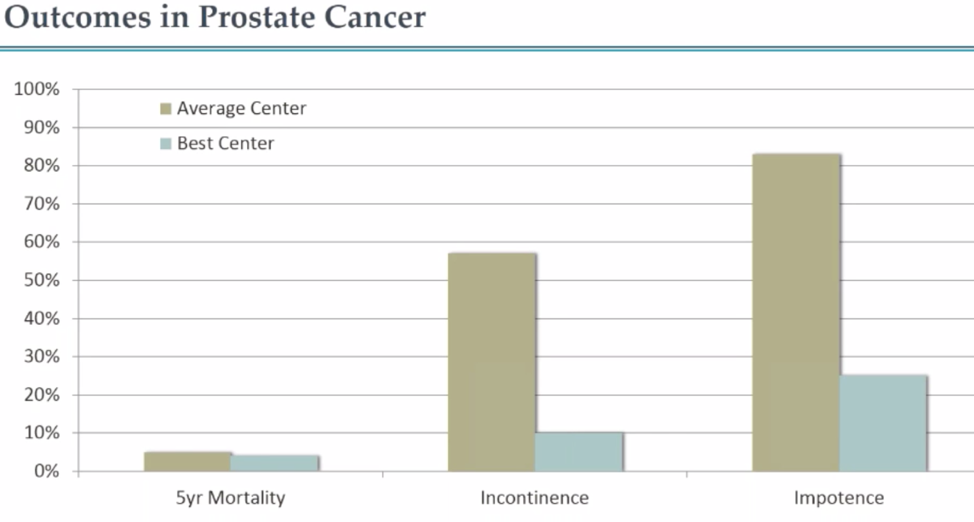
Rather than using variation by provider or mortality to discover value, health systems can use patient-reported outcomes like incontinence after prostatectomy as a metric for quality improvedent. An important thing to keep in mind about variation, especially in surgery is to be very thoughtful about case mix and know that each patient is not necessarily comparable to another. Physicians and surgeons should not be penalized for taking care of patients with greater comorbidities or with lower pre-op scores. When a health system plots and compares outcomes of faculty, looking for the lowest incontinence scores, they should consider the case mix, surgical technique, and any other extenuating factors to help manage and position the data with care. The goal is to identify best practices and drive system-wide quality improvement.
PROs can also help surface and guide appropriateness and efficiency efforts. Many different techniques used in the OR and they’re all attributed to very different costs. When looking at a measurement like physical function after different types of reconstruction, the data shows that the three main ways of reconstructing a hip are associated with very different costs. The most expensive surgery actually had the lowest PROMIS physical function scores, so keep in mind that the most expensive treatment isn’t necessarily the best one.
When it comes to cancer surgery, sometimes the options available to patients are incredibly morbid and they’re faced with terrible choices where they trade off mortality versus morbidity. Patient-reported outcome measures can serve as a valuable tool by telling patients the experience of those who have gone before them.
Another great example is a laminectomy. Data shows that whatever level of leg pain patients present with is going to be cut in half. If a patient wants to know how he’s going to recover from his laminectomy, he can look at the PROMs data and see that immediately after surgery, most patients have almost no leg pain, but around the three-month mark, some of that pain starts to creep back in. Now the patient has that expectation and doesn’t need to call the physician’s office wondering what happened. This is a key factor in appropriately setting patient expectations and guiding decision-making in terms of whether or not the patient feels the benefit is high enough to justify the surgery.
PROMs can even be helpful from the standpoint of office flow and mitigating phone calls about patient concerns that perhaps something went wrong with their surgery. This is important to note when thinking about getting already-overwhelmed providers to do “one more thing.”
As health systems progress toward improving care, reducing costs, and empowering patients, it can be difficult to know how to push past the landscape of “I can’t do one more thing” when it comes to clinician buy-in. Providers are being asked to do more and more with less and less. There are more regulations, a lot of which don’t make sense from a clinical perspective, and many providers are frustrated.
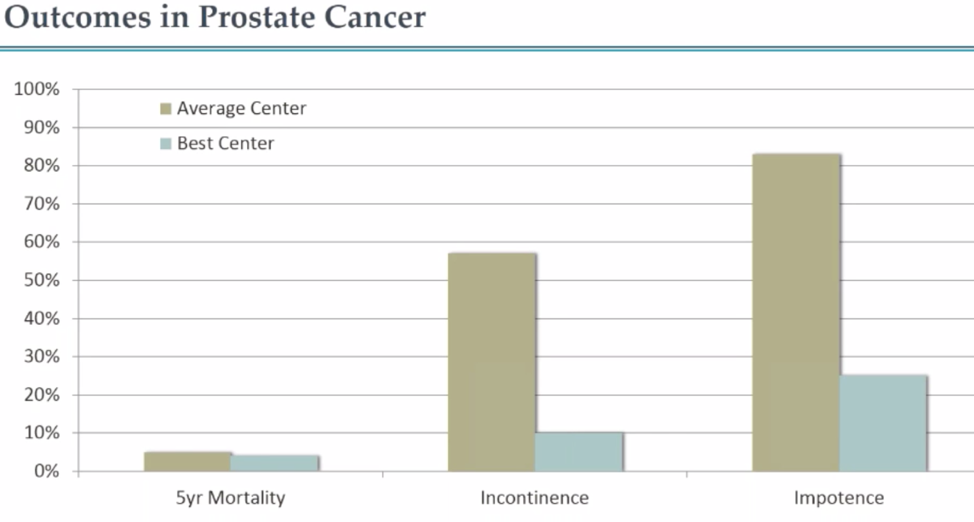
Even though patient-reported outcome measures can seem like a hurdle, the additional data can save health systems and providers time and enable deeper understanding and more personalized care. For example, providers can see the last two pain scores in the patient’s medical record since they came under the provider’s care, shown using an example patient in Figure 2.
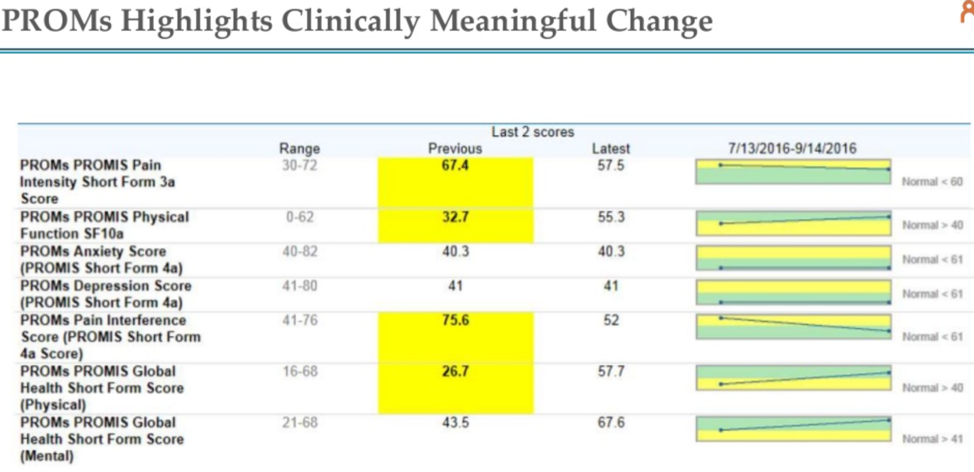
Using the example patient above in Figure 2, scores highlighted in yellow are out of range and abnormal. When this patient was initially seen, she had multiple domains that were concerning, including pain, physical function, pain interference with her day-to-day life, and global health (meaning how she was doing every day). Within this 2-month timeframe, the patient moved to within the normal range in every parameter. In a time when many providers feel like they receive a lot of negative feedback and it can be hard to quantify how well they’re doing, this type of feedback from PROs can be very rewarding for both providers and patients.
Perhaps one of the key benefits of PROs is to demonstrate value and transparency to patients. Partners Healthcare has created a forward-facing website called Care Decisions, that makes PROs data publicly available. The website shares data about heart disease, knee pain/arthritis, spinal stenosis, and prostate care that can help guide patient decisions.
As healthcare organizations begin to explore the power of PROMs, they start seeing the value in many areas, including improving personalized care, shared-decision making, quality improvement, appropriateness and efficiency, and transparency. The next question is how to actually implement PROMs. Effective implementation requires a series of specific steps to ensure success:
Whether to start implementation versus analysis first is a classic “chicken or egg” question. For data to show relevance, health systems need to implement PROMs. To implement PROMs, clinicians often want data about why it’s important. One thing to keep in mind is that a complete stop to the program can occur when physicians aren’t given the data from PROMs, especially as it’s looking at variation amongst providers. The key is to start small with someone who has faith in the program and then reward that faith by feeding their data back to that person in a timely fashion.
The other key to implementation is agreeing on which patient-reported outcomes to measure. With very rare exceptions, when asked more than 30 questions, patients stop participating. Other tips for successful implementation include:
PROs are the outcome metric of relevance for many conditions treated. They are the missing link in defining a good outcome by capturing quality-of-life issues that are often the reason patients seek treatment. The results often vary considerably among treatment options, providers, and facilities, providing patients with more decision-making power geared toward the things they care about most. Making patient-reported outcomes a focus of care also gives providers power to improve patient care and the health of populations.