By committing to transforming healthcare analytics, organizations can eventually save hundreds of millions of dollars (depending on their size) and achieve comprehensive outcomes improvement. The transformation helps organizations achieve the analytics efficiency needed to navigate the complex healthcare landscape of technology, regulatory, and financial challenges and the challenges of value-based care.
To achieve analytics transformation and ROI within a short timeframe, organizations can follow five phases to become data driven:
1. Establish a data-driven culture.
2. Acquire and access data.
3. Establish data stewardship.
4. Establish data quality.
5. Spread data use.

Health systems operate in a complex landscape of technology, regulatory, and financial challenges that demand efficiency and effectiveness in not only their clinical, operational, and financial domains, but also in healthcare IT and analytics. For many organizations, meeting these challenges may feel like attempting to summit Everest. The challenging ascent requires health systems to keep up with the growing use of artificial intelligence (AI) in clinical and operational decision support, the move to value-based care from fee-for-service, the changing aspects of care delivery, and the demanding and ever-changing regulatory environment. To effectively apply analytics to this expanding trove of healthcare data, organizations must be adept at analytics.
Many outcomes improvement efforts center around clinical, operational, and financial goals and associated metrics (e.g., reducing length of stay [LOS], reducing readmissions and ED wait times, and improving revenue cycle management). Analytics improvement efforts, however, address unique concerns in the healthcare continuum:
An effective analytics improvement strategy can enable tens of millions in savings at the start, not just from clinical or operational perspectives, but from an analytics perspective as well. Eventually, estimated savings could grow to hundreds of millions, depending on the size and makeup of the organization. Success depends on the organization establishing a data-driven culture and a willingness to actively and mindfully manage this change. This article explains how health systems can achieve analytics transformation, and the corresponding ROI, within a short timeframe.
Before health systems can dive into analytics transformation, they need to understand their organizational structures (and how those structures support analytics) and determine the number of roles involved in the transforming healthcare analytics. For example, during the data warehouse consolidation phase, the roles include project and change management, active leadership, infrastructure development, legacy application support, and analytics engineering. With the organizational structure defined, before launching into analytics transformation, health systems must conduct an internal analysis of three things:
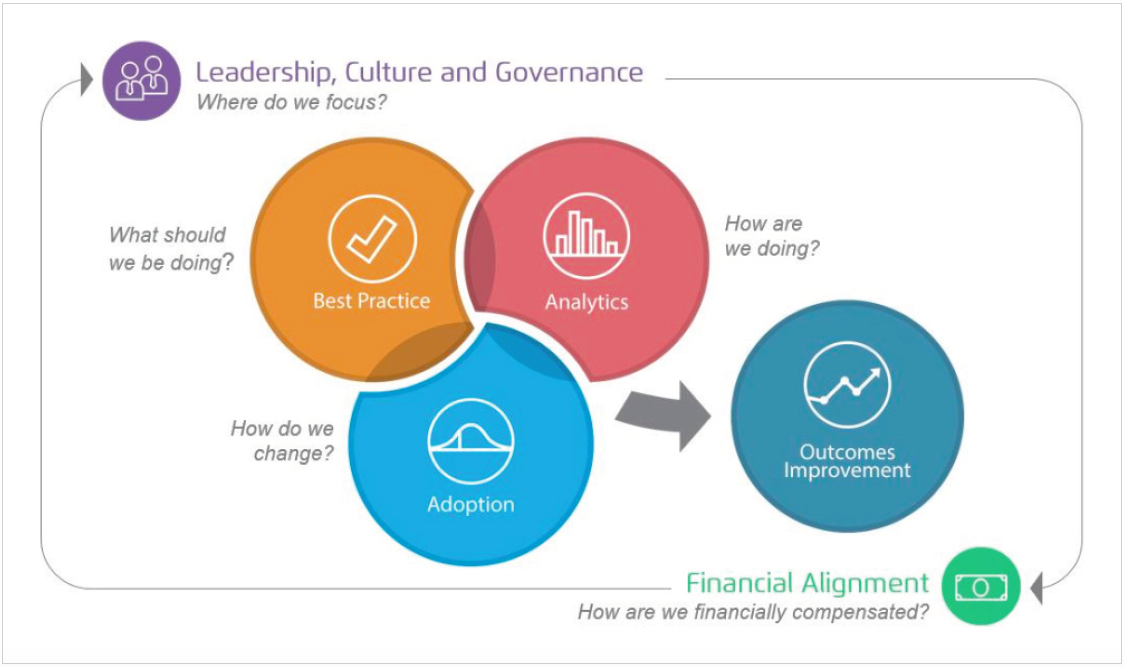
Figure 1 shows the core areas each organization needs to consider and become proficient in to become data driven. Each area has associated capabilities that need to be coordinated and in balance with each other; this is the foundation for comprehensive outcomes improvement.

By exposing and thoughtfully addressing the duplication of staff (or unnecessary licensing, hardware, and contractor costs), the analyses of full-time equivalents (FTE), costs, and current workload assignments will set the expectations and goals of the analytics improvement strategy for all participating. Now, health systems are prepared to navigate the five phases of becoming data driven.
There are five phases of becoming a data-driven organization:
When organizations accomplish these five phases, they can take the following steps toward their desired objectives:
Healthcare organizations and analytics partners share the responsibilities in each of the five phases of becoming a data-driven organization:
The health system selects members for the data governance committee (a subcommittee to an existing governance structure). The data governance committee creates a plan to organize the people, processes, and technology that will maximize the value of the organization’s data and resources that interact within the analytic space. The data governance committee then establishes its mission and charter (goals and purposes) and selects an enterprise data warehouse (EDW), business intelligence (BI) tool, training methods, data stewardship, and data access.
During phase one, the organization also establishes the importance of maintaining existing analytic activities through the transition. The organization is responsible—with partner support—for determining the strategic and business priorities and identifying legacy services that will migrate into the EDW during the transformation. Focusing on data and the processes to attain it allows the organization to begin to shift to a data-driven culture across the system.
In this phase, the health system integrates data from legacy systems, departmental systems, and other siloed data marts with the creation of the EDW. The data governance committee consolidates support of the EDW, BI tool, and methods and policies it selected during phase one.
During phase two, the data governance committee sustains current analytic activities as it transitions to the new platform, while managing exit strategies from old data marts. The organization can assess capabilities of potential analytics team members at this time, using tools such as skills surveys and functional assessments of legacy support team members, along with individuals who were initially integrated into managing the new EDW and BI space.
In phase three, the organization consolidates any functions that can be more cost effective when performed centrally. This may include team members who were previously report writers. Responsible data stewardship also means centralizing some analytic capabilities to support enterprise programs and performance improvement initiatives, while appropriately maintaining and accelerating analytic capabilities in key areas:
In phase four, the health system establishes data validation processes and engages data stewards and analytic team members to promote quality and literacy across all data systems, in both acquisition and logical representation. End users must have trusted and verifiable data to make decisions and change practice patterns. Organizations need pragmatic processes to correct data quality errors in the original source systems to establish trust in the usable data. They also need to establish data and metric definitions to ensure they’re using the appropriate data for the project.
Regulatory and reimbursement pressures are significant and increasing. Health systems need to consolidate and align measure work to maximize quality-based financial incentives and address regulatory reporting requires. Using analytics to support this effort will free time for clinical and analyst resources.
In phase five, the health system establishes processes to measure data access and use, and to identify additional user-requested data sources. With trusted data in hand and a willingness to make improvements across the organization, improvement teams must actively market the transformation to the entire organization, sharing the data efficiencies gained and yet to be gained. A roll-out plan for the new EDW is as essential as a project plan.
Health systems are successfully becoming data-driven when they make decisions from data rather than instinct alone, measure compliance against regulatory measures, reduce variation and waste across the system, and integrate risk management and predictive analytics into the healthcare workflow.
To effectively leverage the work from the five phases of analytics transformation, health systems must revise their existing IT framework or build a new one. This should always be under the guidance of the executive leadership to appropriately align resources and efforts that support the organization’s strategic plan. There are three common framework options:
Many leading analytics IT vendors recommend the hub-and-spoke IT framework (Figure 2) for organizations seeking to transform their analytics strategies, depending on the size and organizational structure.
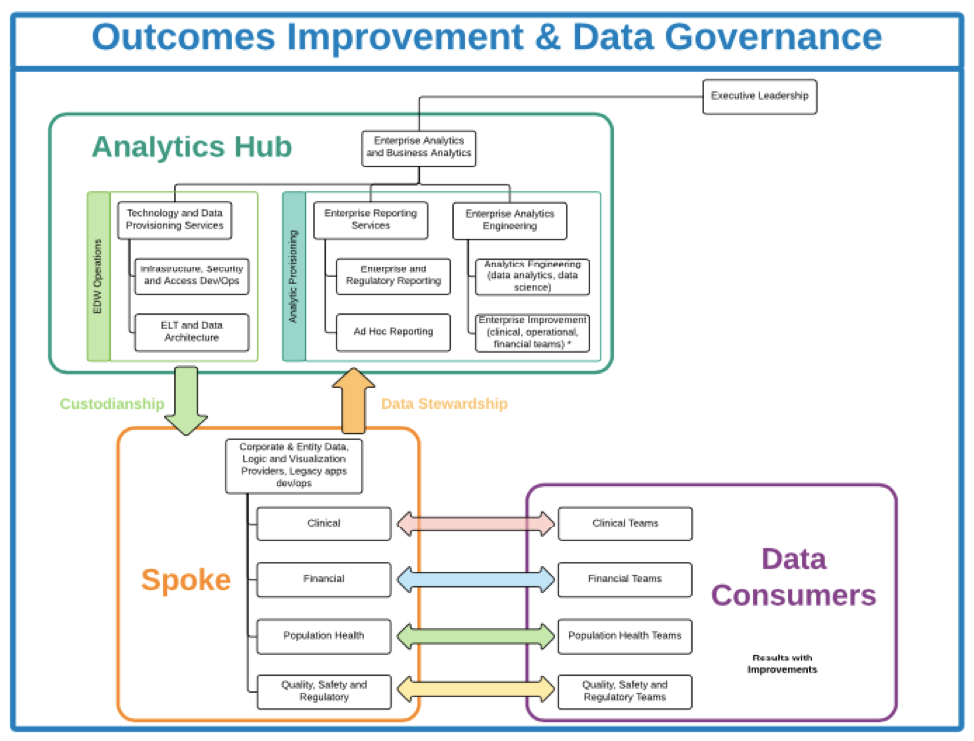
This main group structure represents the hub. Clinical, financial, and operational teams (as well as ad hoc reporting teams) represent the spokes. The hub-and-spoke framework allows centralization and deduplication of services in the hub. The teams in the spokes have access and control, which allows them to accomplish their work. The spokes interact with, and depend on, the hub, and data governance policies guide decisions throughout this structure creating a collaborative feedback loop.
Building the IT framework starts with executive leadership taking responsibility for data governance over the entire framework, both hub and spoke. Next, the executive leadership establishes an analytics governing body—an enterprise-wide analytics and business intelligence group that oversees four recommended groups of the IT framework:
A typical analytics transformation has a short time to value. The sample timeline in Figure 3 shows how healthcare organizations can go from base camp (phase one: setting the cultural tone of being data driven) to the summit (phase five: utilizing data) in less than 12 months. The size of the organization and its readiness for change may impact the timelines.
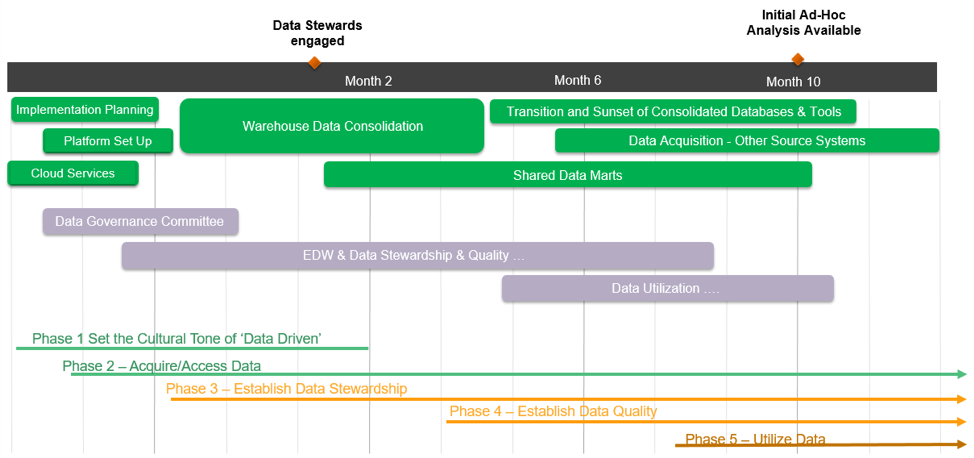
As the timeline shows, several technology projects can launch concurrently, some even as the organization is still establishing a data-driven culture. It’s important to note that, during year one, while the organization is focused on analytics infrastructure and improvements, it will accomplish other important goals, such as improving report writing and surfacing dashboards; it may not, however, realize substantial measurable improvements (e.g., reducing variation, creating efficiencies, and improving finances) until a year two or later.
Once health systems have worked through the five phases of becoming data driven and built an appropriate IT framework, they need experienced partners with the proven ability to meet the challenges of analytics transformation. The outcomes listed below demonstrate the types of improvement possibilities and ROI that can result from these effective partnerships:
Texas Children’s Hospital significantly reduced reporting costs using a healthcare EDW:
Partners Healthcare deepened its understanding to the market trends and business drivers of a complex healthcare organization:
Memorial Hospital avoided PQRS penalties and earned potential incentives with accurate submission of quality measures:
Service lines and activity-based costing revealed true cost of care for University of Pittsburgh Medical Center: Reduced cost by $42 million.
Faster data acquisition delivered speedy time to value at Orlando Health:
Machine learning, predictive analytics, and process redesign reduced readmission rates by 50 percent at the University of Kansas Health System:
Texas Children’s Hospital delivered systemwide performance improvement:
Mission Health used value to prioritize and guide analytics investments:
In each of these success stories, health systems carefully selected their summits, dedicated themselves to their training and preparation, and chose the right partners, or guides, to help them safely and successfully reach their goals.
Just as a mountaineering expedition begins at base camp and requires certain preparation, processes, equipment, and guidance to reach the summit, health systems can scale the tallest peaks of healthcare improvement and cost savings by following a plan (the five phases of IT and analytics transformation), including identifying an opportunity, choosing the right IT infrastructure, and forming partnerships that support the journey.
Transforming IT and analytics has a profound impact on an organization’s people, finances, and overall outcomes, which can optimize the business of healthcare to meet the challenges of value-based care.
Would you like to use or share these concepts? Download this presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/u7flgBa9jPu3m1