How to Avoid PQRS Penalties and Earn Potential Incentives with Accurate Submission of Quality Measures

- Successfully leveraged the EDW to avoid the 4 percent Medicare reimbursement adjustment from the PQRS and VM programs
- Team was able to avoid difficult and time-consuming manual data collection as well as identify opportunities to improve data quality
For several years, the Centers for Medicare and Medicaid Services (CMS) has been leading the shift from fee-for-service to value-based reimbursement by implementing initiatives that reward quality while controlling costs. One of the initial programs it created for this purpose is the Physician Quality Reporting System (PQRS). PQRS started as an upside-only program—a basic pay-for-reporting incentive where physicians earned a 0.5 percent incentive payment against their total Medicare Part B fee-for-service charges regardless of treatment outcomes.1
With the multitude of demands on their practices mounting, many physicians viewed PQRS reporting as burdensome and potentially optional. However, CMS has steadily transitioned the program to a focus on performance and outcomes with real consequences for nonparticipants. In fact, in 2015, CMS began to apply a negative payment adjustment to providers who do not satisfactorily report data on quality measures. Providers across the country who are unable to successfully meet PQRS requirements will collectively forfeit millions of dollars.
The new payment penalties lag by two years, and many physicians will feel the negative repercussions of unsatisfactory or nonexistent reporting done back in 2013. Those who chose not to report or whose 2013 reporting was unsuccessful will receive a 1.5 percent penalty in 2015. This penalty will increase to 2 percent in 2016 and beyond.
Physicians and the healthcare systems that employ them must proactively seek solutions to help manage quality metrics for Medicare. Memorial Hospital, one of the most comprehensive healthcare systems in Mississippi, is one organization that is streamlining the data-capture process to ensure that its physicians hit quality benchmarks, achieve Medicare incentives and avoid penalties.
THE CHALLENGE: 4 PERCENT OF MEDICARE REVENUE AT RISK
Memorial Hospital faced a significant problem when its PQRS reporting process was hampered by its transition to a new EHR system. Typically, an EHR vendor would provide PQRS metrics data for submission to CMS. However, Memorial learned that their new EHR vendor would be unable to do this for them for the 2014 submission. For Memorial’s group of more than 100 physicians, the bottom line impact per year of a PQRS penalty for not reporting is in the hundreds of thousands of dollars.
Although PQRS is a standalone program, the 2 percent penalty and the 0.5 percent incentive were not all that was on the line for Memorial. Failure to report for the 2014 PQRS program year would also result in a separate 2 percent cut under CMS’ Value-Based Payment Modifier (VM), a new program that will begin paying incentives or assessing penalties in 2016 based on 2014 data.2 Depending on the physician group’s performance on quality and cost measures as represented in its PQRS reporting, the VM program will result in a 2 percent penalty or up to a 2 percent incentive payment. In short, failure to perform PQRS reporting in 2014 would put a total of 4 percent of Medicare reimbursement at risk for Memorial.
Faced with having to report without support from their new EHR vendor, the Memorial performance improvement (PI) team was confronted with the prospect of doing the work manually. They would have to wade through the roughly 300 PQRS quality measures to begin to figure out which metrics to report on to preserve the Medicare revenue for their organization. The hospital could submit to CMS through a certified registry, but the team realized quickly that they would still need many chart abstractors to gather the necessary data in the needed timeframe. Team members would have to comb through each patient’s chart—and, depending on the measure, there could be between hundreds and tens of thousands of charts to review.
For example, Memorial identified approximately 700 patients under the hypertension metric, which includes patients 18-85 years old with a hypertension diagnosis whose blood pressure was adequately controlled. A manual process would require a team member to spend several minutes per chart to verify the diagnosis and to determine when the last blood pressure was recorded and what that blood pressure reading was. Significantly, other metrics like influenza vaccination would entail reviewing more than 100,000 charts.
SOLUTION: DATA INTEGRATION FOR PROACTIVE MANAGEMENT OF PQRS REPORTING
Memorial needed a solution that could be implemented quickly and save the PI team weeks or months of manual effort abstracting chart data in order to preserve Medicare reimbursement and avoid penalties. The hospital had recently deployed a healthcare enterprise data warehouse (EDW) from Health Catalyst to drive performance improvement initiatives. The EDW aggregates data from multiple EHR, financial, and patient satisfaction systems to create a consistent view of all of the hospital and clinics’ data. This aggregated data can then serve as a single source of truth across the enterprise. The PI team determined to use the EDW to fill its PQRS submission needs.
Memorial brought data from both the old and new EHRs for its 80+ clinics into the EDW along with data from its separate inpatient EHR system. The team also brought other data sources into the EDW, including professional billing data sources for the clinics and hospital, patient survey data that measures patient satisfaction, and general ledger data.
A particular strength of the late-binding data warehouse platform is that it does not require Memorial to develop a detailed data model upfront, which gives the hospital maximum flexibility in how to use the data over time as new use cases present themselves. Thus, when the urgent PQRS reporting need arose, the PI team was easily able to define business rules and registries to address specific PQRS requirements.
Memorial initially studied ten measures knowing they would eliminate some because they were either not feasible or would not meet success criteria. The team ultimately gathered data for six measures across the following three PQRS domains:3
- Effective Clinical Care
- Stroke patients discharged on antithrombotic therapy
- Use of aspirin for CABG/PCI/AMI patients
- Controlling high blood pressure
- Aspirin at ED arrival for AMI patients
- Patient Safety
- Current medications documented in the medical record
- Communication and Care Coordination
- Reminder system for mammogram screenings
Cohorts were created to capture patients that met the criteria for each measure. The team gathered data from the EDW using capabilities that enabled them to drill down into the record for patients in the cohort who met the criteria. Figure 1 summarizes sample data for hypertension, indicating whether the recommended clinical action was performed, and, if not, whether an acceptable reason was documented (e.g., a contraindication). Rather than reviewing each chart manually, the team was able to assess just the exceptions and confirm that a documented reason was recorded.
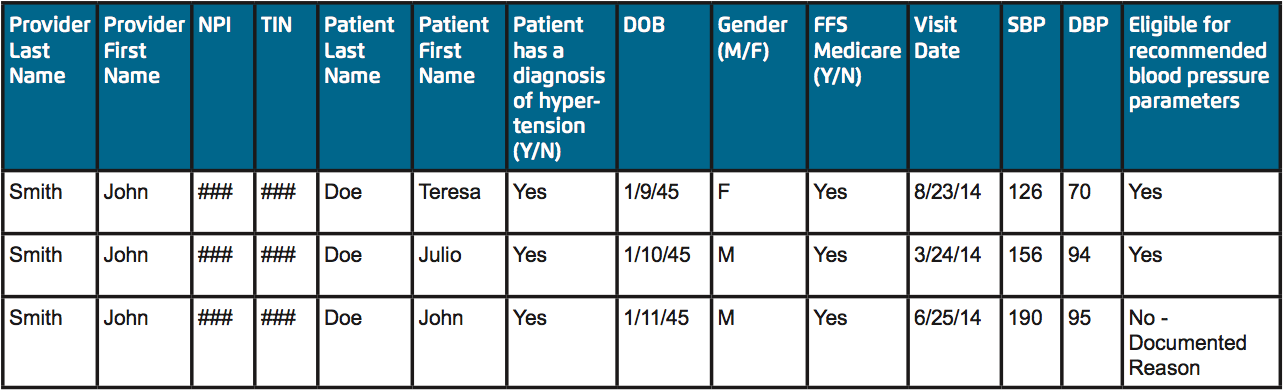
The team pulled ICD-9 or CPT codes from the EDW to serve as the denominators: the number of eligible cases meeting inclusion requirements for each measure. They also pulled the numerator data from the EDW to indicate the clinical action that was performed. Although a certified registry would be required to calculate the official metric, Memorial was able to roll this data up to make a preliminary calculation of its performance on the metric (see Figure 2).
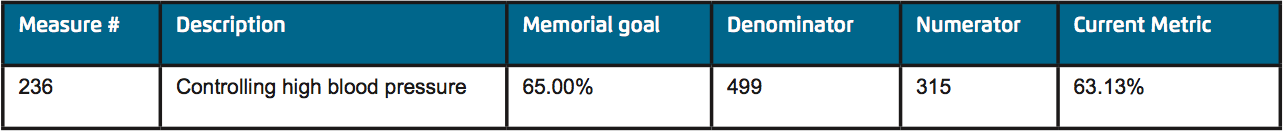
This calculation enabled the team to proactively understand how they were performing and what improvement opportunities existed. In fact, the performance on the ten measures they selected is also being monitored to support their ongoing population health initiative.
RESULTS
Memorial successfully leveraged the EDW to submit the necessary data to a certified registry to avoid the 4 percent Medicare reimbursement adjustment from the PQRS and VM programs. Meeting this reporting requirement saved the organization several hundred thousand dollars.
In addition to safeguarding Medicare reimbursement, the streamlined process enabled by the EDW saved team members significant time and effort. The team avoided difficult and time-consuming manual data collection that would have required them to spend weeks or months reviewing thousands of patient records. The hypertension measure alone, with just 700 patients, would have taken the team a week and a half to complete. The EDW delivered an efficient, automated process that kept chart reviews to a minimum for exceptions only.
Furthermore, during the process of reviewing the exceptions for the various measures, the team identified opportunities to improve data quality. For example, physicians and nurses were often using free- text fields to record important data (such as aspirin administration or cancer staging) rather than the intended discrete fields in the EHR. The team is now able to track and provide feedback on
these measures proactively, which they expect will further improve performance going forward.
“The ability to quickly use the EDW to create a solution to an otherwise extremely time-consuming process has made me very excited about the power and flexibility of the EDW. I look forward to seeing what the EDW will help us achieve in future performance improvement projects.”
– Dean Pearson, RN Director of Quality & Performance Improvement
WHAT’S NEXT
Memorial successfully avoided the 2 percent penalty and will learn in the fall of 2015 whether the 2014 submission has also qualified for a 0.5 percent incentive payment.
The team looks forward to executing on numerous performance improvement initiatives now that they have improved access to data and advanced analytics. For example, the clinics will use the EDW to proactively identify patients who are behind on their preventative screenings. This will enable them to improve population health and demonstrate compliance with measures to private health plans. Other planned improvement initiatives will focus on finance, aimed at reducing the time required to generate inpatient hospital bills and at analyzing and addressing claim denials. The hospital aims to use the EDW to track and improve documentation practices with the goal of ultimately reducing accounts receivable days.
References
- Centers for Medicare & Medicaid. (2014). Physician quality reporting system.
- Centers for Medicare & Medicaid. (2014). Value-based payment modifier.
- Centers for Medicare & Medicaid. (2014). PQRS measures codes.
ABOUT HEALTH CATALYST
Health Catalyst is a mission-driven data warehousing and analytics company that helps healthcare organizations of all sizes perform the clinical, financial, and operational reporting and analysis needed for population health and accountable care. Our proven enterprise data warehouse (EDW) and analytics platform helps improve quality, add efficiency and lower costs in support of more than 50 million patients for organizations ranging from the largest US health system to forward-thinking physician practices.
For more information, visit healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.