Delivering high-quality, cost-efficient care to specific patient populations within a service line is nearly impossible without a sophisticated costing methodology. Activity-based costing (ABC) provides a nuanced, comprehensive view of cost throughout a patient’s journey and reveals the “true cost” of care—the real cost for each product and service based on its actual consumption—which traditional costing systems don’t provide.
With the true cost of care at their fingertips, healthcare leaders can identify at-risk populations earlier—such as pregnant women diagnosed with gestational diabetes mellitus—and more quickly implement effective interventions (e.g., more scrupulous monitoring and earlier screenings). Health systems that leverage the actionable insight from ABC further benefit by implementing the same, or similar, process/clinical improvement measures across other service lines.
 Download
Download

This report is based on a 2018 Healthcare Analytics Summit presentation given by Paula Lounder, Director, UPMC Corporate Finance, Women’s Health Service Line Finance Lead; Hyagriv Simhan, MD, MS, Executive Vice Chair, Obstetrical Services, UPMC; and Beth Quinn, MSN, RNC-MNN, Program Director, Women’s Health Services, UPMC: “Integrating Clinical Improvement and Activity-Based Costing Identifies Pathway to Healthier Moms and Babies.”
With gestational diabetes mellitus (GDM) affecting up to 10 percent of pregnancies in the U.S. every year, health systems have a vested interest in identifying women at risk for the condition as early as possible. GDM—hyperglycemia, or high blood sugar, during pregnancy—not only affects a large population but also increases cost for organizations and compromises care for not one but two patients, the mother and the baby. Furthermore, the mother’s high blood sugar affects the baby’s, exposing newborns to risks including overgrowth, trauma due to large size at delivery, metabolic consequences, hypoglycemia, jaundice, and increased chance of cesarean section delivery.
For healthcare organizations today—whether for-profit or not-for-profit, in an urban or rural area—the biggest challenges in delivering quality healthcare are sustainability and cost. Because GDM affects two patients, doubling health risks and cost, GDM is potentially a significant opportunity area for improvement. And, with mounting pressure to deliver better care with fewer resources, health systems face a larger threat that is often overlooked in the journey to meet these new standards of care: inaccurate, siloed data. Comprehensive, actionable data—derived through an activity-based costing (ABC) system—improves healthcare delivery by laying the foundation for long-lasting clinical and administrative improvement.
Rather than rely on traditional, outdated costing systems, healthcare organizations can leverage data to improve healthcare delivery with ABC solutions, a costing methodology that assigns a cost to each product and service based on its actual consumption. With ABC applied to a specific service line (e.g., maternal-fetal medicine [MFM], more commonly known as care for high-risk pregnancy), service line leaders and providers can identify a patient’s risk for certain conditions earlier, improve patient outcomes, and decrease cost overtime.
Although improving clinical care processes might seem like an obvious focus for improving GDM, insight from ABC spurs the real change. This sophisticated costing approach allows service lines, such as MFM, to understand the nuances of cost across every activity within a high-risk pregnancy and effectively manage these costs at a granular level, versus the limited traditional cost accounting approach that provides only siloed data at a high level.
Proper implementation and process changes are critical for success in an advanced ABC landscape; however, the importance of collaboration cannot be overstated. In a collaborative approach, multidisciplinary leadership works with stakeholders from not only the clinical arena but also operations, finance, and information technology; each team brings a different perspective from their unique discipline. In some cases, organizations may need to restructure teams or create new ones to foster an environment for successful ABC (particularly if current team structure is based on antiquated costing systems).
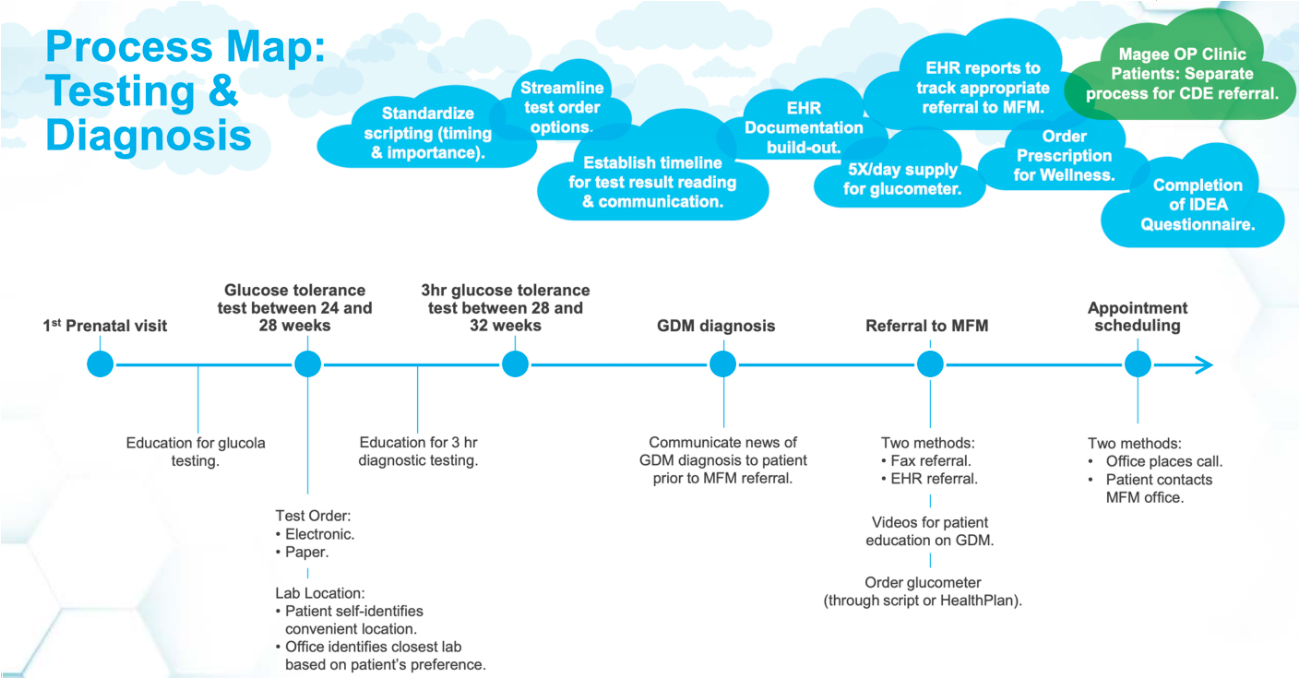
For example, when the University of Pittsburgh Medical Center (UPMC) decided to leverage ABC in its GDM improvement efforts, the health system built a new team around ABC. The organization’s MFM leadership created a multidisciplinary team that leveraged the actionable analytics from the new costing system to create a reliable process map (Figure 1), including sustainable solutions.
Data-derived improvements included how to engage frontline staff earlier, identify institutional champions, and communicate process changes to avoid duplicate work. The diversity of thinking and collaborative efforts, based on accurate data, also empowered UPMC to achieve standardization and consistency in its MFM department and across its system of 30-plus academic, community, and specialty hospitals.
A service-line management approach combined with an ABC system give organizations easy access to integrated clinical and financial information for specific patient populations, allowing clinicians to immediately and more easily identify populations at risk (e.g., expectant mothers with GDM) and define appropriate interventions.
Ideally, OBGYNs would identify risks for and signs of GDM early and immediately refer patients to MFM providers for diagnosis and management. Effective management would include reliable postpartum follow-up with a six-week checkup and a diabetes screening to prevent Type 2 diabetes.
However, early identification and intervention is only possible when health systems understand the complete picture of cost across the continuum of care for a patient. The ABC approach combines data from disparate sources, fostering better communication between the clinical, financial, quality, and IT teams and giving all sides an accurate, comprehensive view of cost for specific services and episodes of care within the service line. With ABC methodology, health systems see the “true cost” of care at the patient level—insight traditional costing systems can’t provide.
ABC generates the true cost, or actual cost, of GDM by allowing for every contact the patient has at the healthcare organization throughout her pregnancy and after delivery. This true cost includes primary costs (e.g., administrative costs and provider costs) and the cost of secondary support systems that are often unaccounted for.
In the case study at UMPC, ABC allowed the health system to capture each aspect of a woman’s nine-month prenatal care experience, including regular OBGYN visits, ultrasounds, lab work, delivery, post-delivery inpatient stay, care for the new patient (the newborn), any testing during the inpatient stay, and postpartum care.
By revealing quality data at the patient level, ABC helps organizations generate patient lists by physician, facility, procedure, or diagnosis. ABC also allows all teams across the system to easily sift through large amounts of actionable data and present findings much faster than with traditional costing. Improvement teams can write queries to automatically identify at-risk populations, eliminate waste and costly inefficient processes, and immediately intervene for at-risk women.
Aligning cost and quality through ABC allows health systems to target specific patient populations and thoroughly review subpopulations of larger groups to create more targeted preventive interventions.
The new cost data empowered UPMC to tailor care to the subpopulations within the MFM group, rather than delivering the same care to all women experiencing a high-risk pregnancy. For example, the data revealed that women within the MFM group who experienced two or more conditions—aside from being high risk—incurred nearly a quarter of all GDM expenses. With that data, UPMC implemented a different set of care standards that addressed the other health conditions earlier and watched them more closely throughout the pregnancy. UPMC also implemented other interventions in its diagnostic and screening processes, based on this new insight, that clearly defined best practices when caring for a high-risk pregnancy.
By merging cost and quality data, ABC revealed the following areas UPMC had not previously targeted because the old costing system didn’t identify them as opportunities:
Gaining executive sponsorship and clinician engagement is also imperative in creating a new pathway to ABC success. When leaders, both clinical and non-clinical, understand the benefits of the sophisticated ABC approach—as it reveals supply and labor costs, assigns cost to multiple activities within a department, and uses a fluid cost mechanism—they can mold the cost strategy and its features to fit the health system’s unique needs.
Once the ABC foundation is laid, the team leading the change must collaborate and create an environment in which a flexible, iterative approach—based on reliable, actionable data from the new ABC model—can be successful. With buy-in at the executive level and clinical champions on the forefront, team leads are empowered to deviate from the standard course and roll out practices to support the new strategy. Leadership must also ensure the continued merging of finance, quality, and operations data and fight the urge to fall into old patterns that might feel easy and more familiar.
At UPMC, the support and positivity of its leadership team led to more effective results. As the team fine-tuned their approach to treat women with GDM, they were careful to make sure the new processes were sustainable and scalable across other service lines throughout the system.
As organizations implement the ABC approach and see reduced costs and improved clinical outcomes, they have tremendous opportunity to spread the wealth. Relying on ABC to understand data across an entire service line, such as MFM, allows leadership to take advantage of economies-of-scale cost savings by implementing similar changes for other service lines.
For example, leaders can roll out the same, or a similar, standardized education plan they used within one service to all providers and hospital administration serving the OB population. Leadership can also scale new interventions, based on the ABC data, across other service lines, including best-practice alerts within the EHR, standardized education plans across other hospitals and clinics, and process improvements to ensure consistency and a seamless experience for patients and their families.
UPMC’s improved neonatal outcomes and better practices for high-risk pregnant patients were due to many factors (leadership support, collaborative environment, etc.), but, by offering cost insight at a detailed level, the ABC approach, combined with leadership support, was the perfect recipe for success within the high-risk pregnancy population, and now other service lines. The GDM initiative illustrated the value of tying detailed cost data closely to a clinical improvement project, engaging stakeholders early for assistance with multiple levels of intervention, and identifying other areas in which to repurpose these new principles.
Clinical solutions can seem straightforward and even easy to apply, but the reality of delivering better care while utilizing fewer resources is nuanced and complex, requiring a range of experts throughout the brainstorming and problem-solving phase—but only after ABC methodology is in place. With the power that comes from easy-to-access, reliable data at a granular level, healthcare organizations can leverage data through ABC to prioritize problem areas, eliminate waste, and make a plan that tackles all touchpoints of the pregnancy journey, leading to decreased costs and improved outcomes for mothers and their newborns.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download the presentation highlighting the key main points.