Up to 50 percent of hospital deaths in the U.S. are linked to sepsis, prompting Piedmont Healthcare to adopt innovative quality improvement methods. The health system established a "core and spread" team structure and used a sepsis prevention analytics application to enhance care. Piedmont's approach to improving sepsis outcomes, tying outcomes to interventions, and using nurse-driven protocols have led to sustained practice change, increased engagement from all staff levels, and improved patient outcomes.
Up to 50 percent of all hospital deaths in the United States are linked to sepsis.1 That statistic was not lost on Piedmont Healthcare, a system of six hospitals and more than 100 physician and specialist offices across greater Atlanta and North Georgia. Sepsis accounted for half of Piedmont’s mortality rate, despite years of progress in sepsis care.
Piedmont leaders recognized that they needed an innovative quality improvement methodology to spread best practices and sustain improvement, supported by an accessible source of timely, reliable, and actionable information. They therefore implemented a “core and spread” team structure to promote enterprise-wide adoption of best practices. The health system also deployed a sepsis prevention analytics application to deliver performance insight to all levels of the organization, and discovered a high correlation between better patient and financial outcomes and the number of bundle elements the patient received. Being able to tie outcomes to interventions, along with the incorporation of nurse-driven protocols, resulted in sustained practice change and greater engagement from physicians, nursing and frontline staff, all the way to the Board level.
Time is literally of the essence when treating sepsis. Every hour a patient in septic shock doesn’t receive antibiotics, the risk of death increases by 7.6 percent.2
Health systems could reduce that mortality rate considerably by identifying the onset of sepsis in their patients more quickly. In fact, experts estimate that if U.S. providers as a whole achieved earlier sepsis identification, they would save 92,000 lives per year. Furthermore, they would reduce annual hospital days by 1.25 million and hospital expenditures by more than $1.5 billion.3
To help health systems save lives, the Surviving Sepsis Campaign has developed guidelines and best-practices standards, such as three-hour and six-hour care treatment bundles and early alerts for the presence of sepsis. These evidence-based standards have proven effective in improving sepsis outcomes—including lowering sepsis mortality.4
Piedmont Healthcare has long recognized the importance of the work of the Surviving Sepsis Campaign. Over the past decade, the health system has sought to achieve widespread adoption of the campaign’s best-practice bundles in order to improve clinical and cost outcomes of patients with sepsis in their facilities.
With nearly 50 percent of Piedmont’s hospital mortality resulting from sepsis, however, Piedmont leadership knew there was more work to be done. They therefore recognized that a new approach was required to address this high-stakes challenge.
Leaders at Piedmont decided to form a new kind of improvement team that would focus on decreasing mortality and length of stay (LOS) for sepsis patients.
Members of this new team knew that standardizing and changing clinical practice can be difficult in large, complex organizations. In their experience, quality improvement initiatives did not always deliver on sustained outcomes.
Finding ways to achieve adoption of best practice across multiple hospitals and to hardwire hard-won processes into practice in order to sustain improvements had proven to be a significant challenge. In the past, Piedmont had educated its clinicians on sepsis best-practice interventions (including the three-hour bundle), but education alone had not brought about the hoped-for changes in practice.
The new team would have to implement an innovative quality improvement methodology to design and execute on the sepsis initiative, supported by an accessible source of timely, reliable, and actionable information. Piedmont needed sepsis outcome and performance data that could be shared with stakeholders across the organization—from executives to physicians and frontline nurses, managers, and quality professionals—to sustain practice changes and to improve outcomes.
The Surviving Sepsis Campaign had already laid the groundwork of identifying the evidence-based practices that Piedmont should implement to improve outcomes. It was up to Piedmont, however, to change its model of engagement and execution if it was to succeed in sustaining changes to clinical practice.
Piedmont is in the midst of what it calls a “quality revolution.” It is laser-focused on how team members design and execute quality improvement as part of their journey of enabling a cultural shift to continuous improvement, accountability, and transparency. This revolution is fueled by the health system’s “core and spread” team concept, an approach to improvement and adoption that was first embraced by the sepsis team.
The core consists of an inter-professional team of experts who are passionate about improving care for patients and who believe they can make a difference. Having the right people on the team, including a strong project or program manager is critical to success. Each team member must be committed to the work, carry his or her weight, and embrace the vision.
This strong, enterprise-wide core team assesses and develops evidence-based best practices and then makes recommendations that are then shared with the larger spread team. This broader team troubleshoots the recommendations, identifies gaps, and comes forward with an improved proposal and with ideas about how to operationalize the recommendations.
The spread team focuses on implementation and execution. Team members develop a solutions package that can be operationalized. They then play an evangelical role in the organization, helping clinicians understand the recommendations and encouraging them to put them into practice. Part of the spread team’s work is also to find ways to push key information about performance to frontline staff.
In addition to the enterprise-wide core sepsis team, each hospital has its own sepsis team consisting of a physician champion, nurse champion, and team members who also meet and drive the recommended changes in their own institution. These champions are critical to moving the work forward in their own areas. For example, Piedmont’s emergency department (ED) nurse and paramedic champions helped develop improvements in some elements of the ED process measures. Champions may have discussions with under-performing peers and conduct peer reviews, supported by data to help change practice.
Piedmont’s sepsis team realized that to improve on the health system’s old model of quality improvement, it needed information about what interventions were the most effective, as well as the ability to visualize progress on outcomes and to give clinicians feedback on their compliance and performance.
To accomplish this, team members implemented a robust analytics application from Health Catalyst that gives them a highly accessible source of timely, reliable, and actionable information. This Sepsis Improvement Application supports Piedmont’s improvement work by tracking sepsis clinical outcomes and compliance with best practices and guidelines, providing accurate, near real-time feedback on performance.
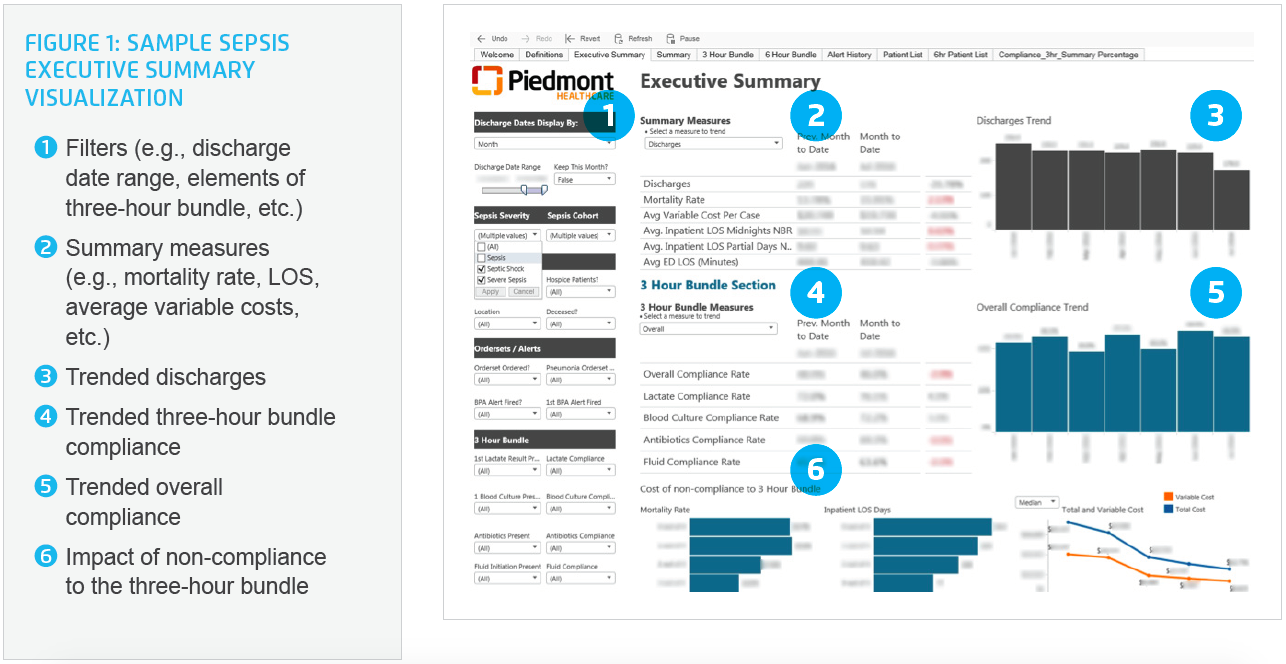
The application’s interactive features enable the sepsis improvement team to quickly and precisely show executives, managers, and frontline staff exactly how well the system as a whole, any given hospital, or an individual is adhering to the best practice three-hour bundle, responding to early sepsis alerts, and how this performance directly impacts LOS, mortality, cost, and patient outcomes (see Figure 1).
As part of this process, Piedmont standardized and aligned metrics and data across the system. The result of this effort was that everyone across the enterprise was speaking the same language (in terms of data and measures) for the first time, enabling them to learn from each other with confidence that comparisons were relevant and valid.
With a functioning sepsis improvement team in place, supported by strong analytics, Piedmont was ready to dive into the work. Armed with the evidence that lives could be saved with early identification of sepsis in the ED and the immediate initiation of the three-hour bundle, the sepsis team looked for ways to hardwire these best practices into clinical processes.
Team members analyzed root causes and ED workflows that might explain any failure to adopt the three-hour bundle. The insights they gained led them to embrace an inter-professional team approach, involving physicians, nurses, paramedics, and quality professionals. Because they wanted to make it easy for clinicians to do the right thing, they not only created evidence-based sepsis order sets, but they also improved the nursing and physician workflows to support early screening and implemented nurse-driven protocols.
Piedmont set out to aggressively screen for sepsis in the ED, knowing that minutes count when it comes to treating sepsis and that early screening of sepsis patients in the ED was the key to improving bundle compliance and lowering mortality rates. By screening every patient for sepsis, using a well-designed evidence-based sepsis order set and early sepsis alerts, the Piedmont team was able to change care and outcomes for patients with sepsis.
Nurse-driven protocols and early identification of sepsis patients have proven instrumental at Piedmont in driving faster initiation of the three-hour bundle. If a patient comes in the door and meets criteria, the best-practice alert (BPA) fires, and the nurse initiates the three-hour bundle based on a nurse-driven protocol. ED nurse champions, armed with near real-time data on performance, worked with their peers to increase the timeliness of response to BPAs and consistent use of the nurse-driven protocol in the ED. With the Sepsis Improvement Application, they can easily see how they are doing and how they are improving—and then share that information with others.
The three-hour bundle, focused on intervention in the ED, contains several elements designed to identify sepsis and to help clinicians intervene as soon as possible. One of those elements is fluid resuscitation to avoid progression to septic shock. At Piedmont, the increased use of the three-hour bundle, and its earlier initiation, resulted in more patients receiving fluid resuscitation. Increased utilization of this intervention in particular appears to correlate to the reduction in mortality. Piedmont continues to reinforce the appropriate use of fluid resuscitation with ongoing education efforts, peer-to-peer conversations supported by accurate data, and increased bundle compliance.
The sepsis team’s most compelling discovery was that the more elements of the bundle the patient received, the greater the reduction in mortality, LOS, and cost. In fact, patients that received all four elements of the three-hour bundle had twice the reduction in mortality (plus greater decreases in LOS and cost) than those that did not receive the bundle at all.
Showing physicians the hard evidence of the impact on outcomes for patients who received the bundle versus those that did not was an eye-opener, and became the driving force that moved their compliance rate up and sustained the changes in practice. When physicians saw sepsis performance data for their own patients, how many bundle elements they received and their outcomes compared to others, it changed practice like nothing else could. They could immediately see the impact on mortality rates, LOS, and variable direct costs.
Data visibility and performance feedback is a powerful driver of change that heightens an appreciation of the impact of individual behavior on outcomes in a very concrete way. The ability to share performance information with physician leads, executives, and nurses in many forums is the power that continues to drive the initiative and enables Piedmont to promote, reinforce, and sustain practice changes.
As a result of this robust quality improvement structure and focused interventions to improve early recognition and use of the three-hour bundle, Piedmont improved its overall bundle compliance by 32.3 percent, with an 18.6 percent improvement in the number of patients receiving the calculated fluid target.
This, in turn, has led to the following impressive improvements in high-level outcomes for patients:
It is important to note that mortality rate, inpatient LOS, total cost of care, and variable cost all improve when clinicians administer even just one of the bundle elements but are best for those patients that receive all four bundle elements.
The Sepsis Improvement Application makes it easy to visualize the compelling impact of not using the bundle elements (see Figure 2). The negative consequences for severe sepsis and septic shock patients that receive none of the bundle elements include:

While lowering cost was not one of Piedmont’s initial goals, the health system’s leaders believed that delivering high-quality, best practice care would result in improvements in the total cost of care—and this has proven to be the case. They believe that when an organization focuses on the right things and the right care, the cost curve will take care of itself.
“Being able to show clinicians that our sepsis patients survive at a much higher rate when we adhere to the three-hour bundle has convinced them that focusing on this issue really does save lives. Having entity-specific data on hand has renewed our passion for improving sepsis care.”
– Dr. Chad Case, Medical Director of Critical Care
Piedmont plans to continue to drive its sepsis mortality rate down by implementing and monitoring process and outcomes measures using its proven quality improvement model. Team members are beginning work on improving compliance with the six-hour bundle for sepsis patients, which will expand the initiative’s focus to include the ICU and inpatient setting.
The new quality improvement structure, supported by analytics, has proven very successful and continues to evolve to support Piedmont’s outcomes improvement work. Piedmont will expand its “core and spread” team structure to other quality improvement initiatives. Leaders also plan to explore innovative ways to push the right data to frontline staff to help them deliver better care and evaluate their performance on key metrics.




