In the U.S., over 1.5 million people are treated for sepsis annually, and one in four people with sepsis die. Read how Allina Health utilized its analytics platform to identify opportunities for improvement and develop evidence-based processes for sepsis identification and treatment.
In the U.S., over 1.5 million people are treated for sepsis annually. One in four people with sepsis die, making improving early identification and providing patients with timely treatment a top priority. Hospitals and health systems continue to look to improve outcomes for patients with sepsis.
Allina Health, a not-for-profit healthcare system of 12 hospitals and 90 clinics, all serving patients throughout Minnesota and western Wisconsin, previously implemented a rapid process improvement project using a three-part bundle focused on the early identification of sepsis. However, sepsis mortality rates remained higher than desired. After turning to an analytics platform to replace its burdensome manual review process, Allina Health was able to identify opportunities for improvement and develop evidence-based processes for sepsis identification and treatment.
In the U.S., over 1.5 million people are treated for sepsis annually, and one in four of the patients die.1 In an effort to better understand and reduce preventable sepsis mortality, the Centers for Medicare and Medicaid Services (CMS) identified publicly reported measures, including evidence-based 3-hour and 6-hour bundles for sepsis care, defining the timing of specific treatments and assessments for patients recognized as having sepsis.2
Historically, the gold standard for diagnosing sepsis was systemic inflammation response syndrome (SIRS). In 2016, the Society of Critical Care Medicine and the European Society of Intensive Care Medicine published a new clinical definition of sepsis based upon organ dysfunction, with the recommendation to use a sequential organ failure (SOFA) score as an index.3
The core of hospital sepsis improvement efforts relies on using bundles, a select set of elements designed to simplify the complex care processes required to effectively manage patients with severe sepsis. Implementing bundle elements reduces variation in care, allowing improvement teams to create a reliable system that reduces sepsis mortality.4
Allina Health, a not-for-profit healthcare system, is dedicated to the prevention and treatment of illness and enhancing the greater health of individuals, families, and communities throughout Minnesota and western Wisconsin. Allina Health cares for patients from birth to end-of-life through its over 90 clinics, 12 hospitals with over 109,000 inpatient admissions, and 336,000 emergency department visits annually. The health system focused on improving sepsis outcomes as an opportunity to provide better care to its patients.
As sepsis emerged as a national health topic, Allina Health implemented a rapid process improvement project using a three-part bundle focused on early identification of sepsis, yet mortality rates remained higher than desired.
Upon further investigation, Allina Health identified that key components of sepsis care varied widely across the system, including:
The electronic screening tool and alert system in the EMR Allina used were not effective, as they were not located within the clinicians’ workflow. Alerts were triggered when documented patient findings met the inclusion criteria for sepsis care, yet nursing documentation for sepsis was located in a different portion of the EMR, delaying timely sepsis identification and implementation of evidence-based care.
Allina Health lacked meaningful performance data that could be used to evaluate performance. Because documentation of sepsis was not standardized, it was difficult to obtain meaningful data that could be used to guide improvement efforts. To understand performance, Allina Health had to conduct burdensome manual case review, delaying feedback about performance. Even after performing manual case review, the health system was largely unable to give its providers the data they wanted, as it was unable to share provider-specific bundle compliance and could not tie the use of bundle elements to patient outcomes.
To improve its sepsis outcomes, Allina Health needed to better understand its performance and improve the consistency of care provided to patients with sepsis.
To exceed its previous sepsis performance and improve the outcomes for its patients with sepsis, Allina Health elevated the status of the improvement efforts to an ongoing program, convening an improvement team, whose members include physician leadership, nursing leadership, quality specialists, and analysts.
To improve the consistency of care, Allina Health developed and validated standard sepsis order sets, building the order sets in the EMR. Allina Health developed seven sepsis bundle elements that closely mirror the CMS core measures, incorporating decision support tools within the EMR to support timely delivery of the bundle elements, including:
Having established the systemwide standard of care for patients with sepsis, Allina Health developed a robust communication and implementation plan, informing providers and nursing staff of the seven sepsis bundle elements, including inclusion criteria, and the recommended treatment interventions. At-the-elbow support and coaching was also offered to clinicians providing care to patients with sepsis.
To further support improvement efforts Allina Health identified that additional clinician expertise was needed, creating a formal sepsis program coordinator role. The sepsis program coordinators are registered nurses (RN) with both clinical expertise and performance improvement skills. The sepsis program coordinators monitor performance and facilitate process improvement efforts at the point of care while ensuring protocols are in alignment with current best practices.
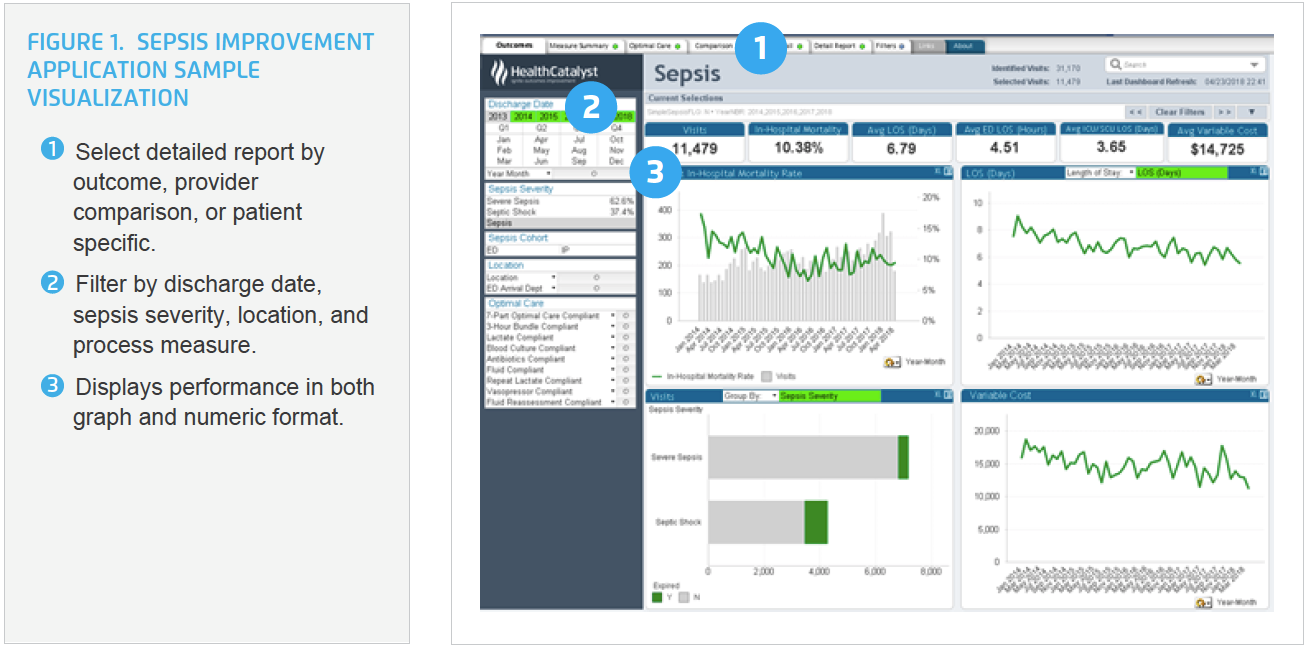
To gain insight into sepsis performance that could be used to drive improvement, Allina Health leveraged the Health Catalyst® Data Operating System (DOS™) Platform, implementing the Sepsis Improvement Application. The analytics application is designed for clinicians, medical directors, operational directors, and clinical program guidance teams in the emergency, intensive care, and inpatient units. The analytics application provides near real-time actionable data to help improve early recognition of sepsis, early intervention for severe sepsis, and early therapy for septic shock to reduce mortality, morbidity, and cost (see Figure 1).
With the new insight provided by the analytics application, Allina Health conducted a deep dive into its data, discovering that more than 85 percent of its patients with sepsis arrived through the ED, leading to additional, focused educational efforts for ED clinicians including:
A systemwide standard sepsis alert was built within the EMR driving interventions in alignment with ED workflow and documentation, including:
Using the analytics application, Allina Health is able to monitor performance in near real-time including, patient volumes, acuity, mortality, LOS, and costs at the individual patient, physician, nurse, and unit level. Formal feedback on sepsis improvement performance is provided on a monthly basis using peer to peer conversations, department meetings, and standard letters, enabling the ability to provide meaningful information on how the bundle use impacts patient outcomes.
By applying this comprehensive, data-driven approach for early identification and reduced variation in sepsis care, Allina Health’s multi-year improvement journey has realized substantial improvements in the outcomes for patients with sepsis, including:
Allina Health achieved these notable improvements while the number of patients diagnosed with sepsis increased by more than 30 percent, reflecting an improvement in the timely recognition of sepsis.
“Sepsis is evolving, and change is difficult. Physicians value data that demonstrates how changes in their workflow impact patient care. For example, showing physicians that the use of the sepsis order set decreases variability and improves outcomes has increased use of the sepsis order set. Providing relevant data and individual provider feedback are the tools we rely on to educate and engage physicians to change behaviors.”
– Sandy J. Fritzlar, MD, Emergency Medicine Physician, Medical Director of the Allina Sepsis Program
Allina continues to monitor performance and provide feedback as part of the ongoing sepsis improvement program, engaging its clinicians in meaningful dialogue to sustain and further improve upon patient outcomes, as well as further refine processes as new evidence is available.




