Children's Hospital of Wisconsin (CHW) focused on reducing hospital-acquired conditions (HACs) like CLABSIs and pressure ulcers through systematic changes, emphasizing staff education and a new governance structure. The organization's comprehensive HAC reduction plan led to measurable improvements in care quality and cost reductions, addressing significant challenges in patient safety.
Hospital-acquired conditions (HACs)—such as central line-associated blood stream infections (CLASBIs) and pressure ulcers (PUs)—cause harm and adversely affect patients’ lives, while also increasing hospital length of stay (LOS) and total hospital costs. In fact, each case of CLABSI alone costs up to $55,000 to treat and makes health systems vulnerable to reimbursement penalties.1
Children’s Hospital of Wisconsin (CHW), a nationally ranked pediatric center with two hospitals and a surgery center, recognized that reducing the rate of HACs in its facilities would require major systematic changes. CHW’s approach to transforming care to prevent HACs included cultural changes with an emphasis on staff education and engagement and a new governance structure to support the initiative. These changes were powered by high-tech tools and quicker access to new types of data that CHW didn’t have in the past.
The hospital’s implementation of its comprehensive and collaborative HAC reduction plan has resulted in measurable quality of care improvements and cost reductions
Children’s Hospital Of Wisconsin is one of the nation’s top pediatric hospitals, ranked nationally in nine specialties by U.S News & World Report and fourth in the country by Parents magazine. Founded in 1894, CHW consists of two hospitals and a surgery center, with services that include primary care, urgent care, emergency care, community health services, foster and adoption services, child and family counseling, child advocacy services, and family resource centers. The hospital’s vision is “healthiest kids in the nation.”
In alignment with its focus, CHW developed and implemented an urgent plan to reduce the incidence of hospital-acquired conditions (HACs) across the organization. HACs are undesirable situations or conditions affecting patients that arise during a stay in a hospital or other similar facility. Among other issues, HACs include central line associated blood stream infections (CLABSIs), catheter-associated urinary tract infections (CAUTIs), venous thromboembolisms (VTEs), pressure ulcers (PU), falls, medication errors, and readmissions.
HACs cause harm and adversely affect patients’ lives, while also increasing hospital length of stay (LOS) and total hospital costs. For example, a recent study reported that children with CLABSIs had an increased average LOS of 19 days, with an associated increased cost of more than $55,000 when compared with patients without a CLABSI.2 Another study found that VTEs resulted in 8.1 additional inpatient days and average excess costs of $27,686, while CAUTIs imparted 2.4 additional inpatient days and average excess costs of $7,200 compared with controls. The study incidence analysis demonstrated 32 VTE, 130 CAUTI, and 3 PU incidents per 10,000 at-risk patient discharges.3
Because of the adverse impact of HACs on patients and increased costs, the Centers for Medicare & Medicaid Services (CMS) and other payers have begun penalizing hospitals for HACs that could have been prevented by following evidence-based guidelines. Although pediatrics has largely been excluded from this trend, the prevention of HACs has become a top priority for forward-thinking organizations, such as CHW, who are driven by the desire to decrease harm, improve patient quality, decrease inpatient LOS, and reduce costs.
In 2012, CHW started taking some steps that would better position them for a data-driven solution to addressing and preventing HACs. In November 2012, the health system implemented an electronic health record (EHR) system. Due to the need for easily accessible data, the HAC improvement work could not start in earnest until after the EHR was implemented.
In addition, in 2012, CHW joined the 110+ member Children’s Hospitals’ Solutions for Patient Safety Network (SPS).4 SPS, a CMS approved hospital engagement network5 is tasked with urgently reducing and then eliminating serious harm in pediatric member hospitals. SPS is focused on preventing readmissions and 11 specific HACs, including CLABSIs, VTEs, and PUs. The objectives for each HAC initiative are to develop and use evidence-based bundles, measure the process of compliance with those bundles with the goal of 90 percent compliance, and most importantly, to reduce HACs by specific percentages each year. Upon signing on with SPS in 2012, CHW’s executive team and its governing board committed to the organization’s vision and goals for pediatric patient safety, with a major emphasis on reducing HACs. As a member of the SPS network, the hospital’s leadership embarked on its comprehensive initiative to reduce HACs of all types starting in 2013. CHW’s vision, strategy, and HAC prevention framework were driven by the SPS vision and strategy.
While CHW had improvement teams in place for many years to address specific HACs, prior to this initiative there had been very little, if any improvement, due to poorly accessible data and a lack of cultural buy-in to the improvement process. CHW leaders knew that major changes would be needed, including the creation of the right environment and infrastructure to support their renewed efforts to reduce HACs across the health system.
Key criteria contributing to CHW’s success have included not only a clear vision and support from the board of directors and senior leadership, but also:
CHW recognized that it needed to look at creating a new, more effective governance structure around safety in order to be successful. From the top of the organization, support for the SPS goals spread to vice presidents and ultimately to the front line, resulting in a strong focus on the SPS evidence-based care bundles and reliability across the organization.
A quality cabinet reporting to the chief executive officer was created to govern the overall improvement efforts. The three areas the cabinet oversees include patient experience; care delivery and health outcomes; and an enterprise safety team (EST), which governs patient safety. The EST is an interdisciplinary team that uses SPS as a framework to guide CHW’s safety journey. The team prioritizes and oversees all patient safety-related work related to the SPS patient safety goals. The EST has identified the organization’s top risks of harm and oversees the teams working to reduce those risks. All teams working on individual HAC reduction programs as defined by the SPS patient safety initiatives ultimately report to the EST.
One of the impediments to progress on HACs prior to the SPS collaboration was a lack of readily accessible data to support improvement efforts. Historically, much of the necessary data to improve HACs was not being captured, and a time-consuming, labor-intensive manual process was required to gather the data and prepare it for analysis. Because this process often took six to seven weeks, true real-time data was not available.
CHW’s first step towards providing ready access to data, was the implementation of an EHR system. Once the EHR was in place, CHW set out to determine what data needed to be measured in order to improve and monitor progress in reducing HACs. To move further towards automated, real-time reporting, a significant effort was made to capture this data in the EHR as a byproduct of work and to eliminate “one-off” reports. However, CHW determined that the EHR was not going to give them what they needed to effectively address HAC reduction.
Ultimately, CHW determined that the Health Catalyst Analytics Platform built using the Late-Binding™ Data Warehouse architecture was the best solution for its needs. This enterprise data warehouse (EDW) is agile and flexible, allowing data to be integrated directly from operational and clinical source systems into the EDW. Some of the major advantages of this platform and related analytics solutions include:
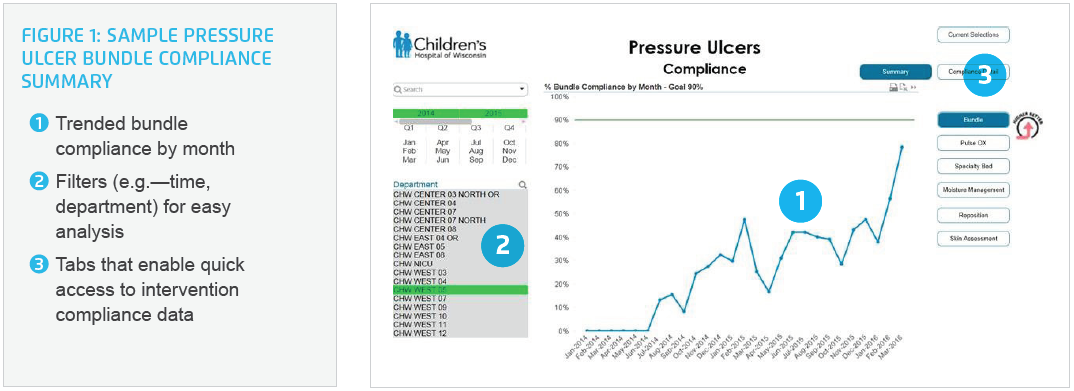
Once the EDW was in place CHW turned to the development of analytics applications to specially address the needs of their organization and reduce HACs. As part of the development process, application designers worked closely with end users to make the applications flexible enough to keep up with improvement teams as they progress and work on new interventions. CHW believed the people that are asking for and using the data need to be at the table in order to believe the data.
CHW found that as staff received access to reliable, actionable data, they soon became eager for ever-increasing amounts of data to improve bundles and prevent HACs. Physicians have quickly embraced the value of data, and they want to make sure that the right data are being captured as care is delivered—for example, surgical procedures.
Core to CHW’s plan was the establishment of a highly collaborative, team-based approach. This relationship centered slant involved the creation hospital HAC teams that are co-led by a physician and nurse and consist of multidisciplinary members, including front-line nurses who serve as HAC champions and guide the front-line teams. All members of the HAC teams are trained to use the HAC apps, to educate staff with unit-specific data to increase compliance with the SPS evidence-based bundles thereby decreasing HAC events.
To support the unit level educational efforts, increase engagement, and accelerate adoption of a data-driven approach to HAC reduction, CHW provided analytics education as well. They had a dedicated trainer on the analytics team responsible for creating the appropriate education/training materials for end users (classroom style, at-the elbow videos, etc.). They also put clinical super-users in place who provide at-the-elbow training for end users.
CHW leaders recognized early on that transparency and standardization were crucial. The organization therefore adopted a policy of being very open with data, with a strong commitment to standardization. From a data transparency perspective, it was critical that people understood the data and knew data was there to support improvement efforts and would not be used in a punitive fashion. From a consistent care delivery perspective, it was important to achieve a systemwide commitment to standardized processes and measurement as a means to reducing HACs.
While there was some resistance, on both fronts initially, particularly with existing teams that felt the processes they had in place addressed the needs sufficiently, both of these hurdles were overcome through leadership involvement and education. Within a year CHW achieved system-wide acceptance and commitment to standardization, transparency, and a data-driven approach. The organization has embraced data, and standardization has been achieved on the management of central lines as well as charting and documentation.
A cultural transformation was critical to ensure that each of the elements put in place to prevent HACs would evolve into permanent, standard operating procedures. In addition to having the EDW and new analytic tools to support improvement efforts, leadership support from the top of the organization including the quality cabinet, to the front-line HAC teams, were key to the cultural shift. Equally essential was physician acceptance and the collaboration of different clinical units across the organization.
With their newly implemented analytic tools, new team structures, and a solid commitment to transparency and standardization, CHW has created a data-empowered culture that will drive continued improvements.
During the cultural shift that was required to make the HAC prevention program successful, CHW had a powerful tool at its disposal to counter any resistance: As soon as outcomes data became available, the proof of the program’s effectiveness was in the numbers.
In the two years since the HAC prevention program was implemented:
A strong organization-wide commitment to reducing HACs has been achieved with 5,000 employees having completed error prevention training.
$1.6 million savings has been realized as a result of a 30 percent reduction in the overall number of HACs.
Elimination of serious harm to patients through reduction in several specific HACs including:
“We’ve changed our culture one person at a time. When it comes to improving patient safety, the entire organization has become one big team.”
– Holly O’Brien, RN, Safety Program Manager
In pursuit of realizing zero harm, CHW will continue progress on current HACs and expand the program to include additional ones—including unplanned extubating and peripheral intravenous infiltrations and extravasations (PIVIEs).
Other initiatives will include:
An overarching goal is to realize an 80 percent decrease in the serious safety event (SSE) rate by December 2017. If the progress so far is any indication, CHW is well on its way to meet—and possibly exceed—that objective.