Almost four trillion dollars is spent on healthcare each year in the U.S., with most expenditures going to patients with chronic health conditions. Patients with chronic health conditions have a high rate of unnecessary visits to the emergency department (ED) and unplanned hospital admissions. UnityPoint Health sought to reduce costs by identifying patients with chronic health conditions at a higher risk for overutilizing healthcare services. By leveraging its analytics platform and augmented intelligence (AI), UnityPoint Health has been able to efficiently identify patients that could benefit from enrollment in its care management program.
More than 90 percent of the $3.8 trillion the U.S. spends annually on healthcare is for people with chronic health conditions.1 Care management is key to decreasing unnecessary healthcare utilization, improving clinical outcomes, increasing quality of life, and lowering healthcare spending. 2
UnityPoint Health recognized patients with complex chronic health conditions were overutilizing healthcare services, particularly when transitioning from hospital admission to an ambulatory care setting. Yet despite having access to large volumes of data, clinicians lacked timely insight into care provided across acute and ambulatory settings.
UnityPoint Health needed to be able to effectively identify patients with high or rising risk of worsening health conditions that often result in non-urgent ED visits or unplanned hospital admissions. Such visits and admissions limit the ability of its care management teams to intervene and provide the care patients needed. The organization desired to integrate AI into its analytics processes to predict which patients could benefit from enrollment in its care management program. The care management program enables care managers to intervene and prevent unnecessary healthcare utilization and reduce spending.
UnityPoint Health established a framework for care coordination across acute and ambulatory care settings with integrated care management programs that share common goals and tools across the organization. The organization leverages the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications to establish a single source of truth across its disparate systems and gain powerful insight into patient characteristics and healthcare utilization patterns. The analytics team and acute and ambulatory clinicians collaborated to develop and enhance the organization’s analytics tools, leveraging data to decrease unnecessary healthcare utilization and ensuring data are shared across care settings for care management program optimization and expansion.
UnityPoint Health uses numerous AI tools that incorporate chronic health data, social data, the probability of admission, and readmission risk after discharge from the hospital to risk-stratify patients and predict which patients are at high or rising risk for unnecessary healthcare utilization. The AI tools enable care managers to identify patients and prioritize them for care management engagement effectively. UnityPoint Health utilizes the following tools for efficient care management:
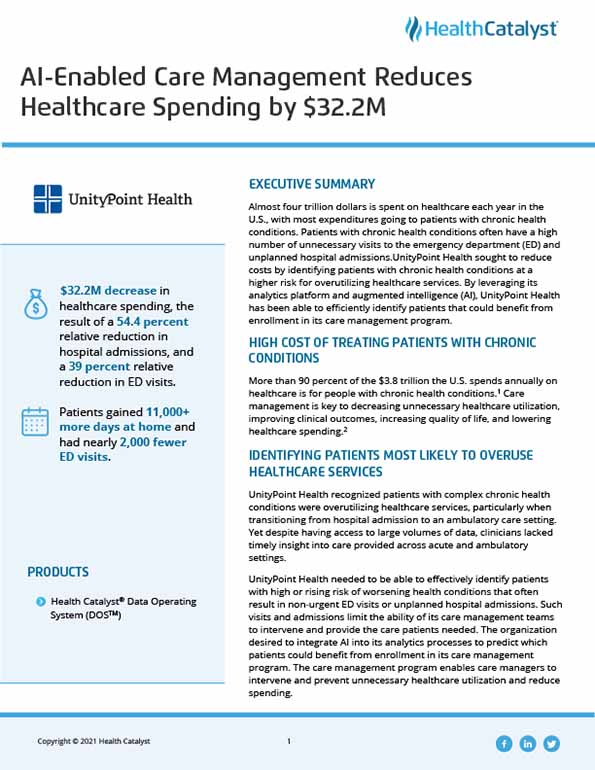
In the 30 months since the care management program’s inception, UnityPoint Health has substantially decreased healthcare utilization and the costs of care for patients who complete the program. The organization has reduced healthcare spending by more than:
"Our successful partnerships leverage the strengths of clinicians and analysts. The team was empowered to build and enhance analytic tools that support the most vulnerable patients, reducing unnecessary utilization and decreasing healthcare spending by more than $32M."
- Rhiannon Harms, Executive Director Strategic Analytics, UnityPoint Health
UnityPoint Health will continue its efforts to enhance and refine the care management program and plans to expand the use of AI and analytics to improve the care provided to its most vulnerable patients, improving outcomes while reducing unnecessary healthcare utilization and costs.