Like other hospitals, Thibodaux Regional Medical Center faced a myriad of new government regulations that made hospital bill collection efforts more burdensome. To improve its discharged not final billed (DNFB) process, the organization automated and streamlined its billing system, utilizing analytics for actionable insights that lead to improved documentation and reimbursement.
A hospital’s core mission is to provide the best care possible. To continue to do so, however, hospitals must be paid promptly. Discharged not final billed (DNFB) cases—where bills remain incomplete due to coding or documentation gaps—represent an ongoing challenge for hospitals around the country. Ineffective management of this caseload can lead to crippled cash flow, mounting accounts receivable days (A/R days), and frustrated staff.
Thibodaux Regional Medical Center, a 185-bed community hospital in Louisiana, like other hospitals, faces a myriad of new government regulations that have made hospital bill collection efforts more onerous. For example, Thibodaux had difficulty adapting to the Centers for Medicare and Medicaid (CMS) reimbursement and auditing practices that required more specific physician documentation to support billing and coding.
Thibodaux’s leaders recognized their inadequate manual DNFB process left hospital staff overburdened and put at risk the necessary cash flow to best serve patients. The hospital automated and streamlined this process, to relieve the burden on physicians, provide an integrated view of data, optimize visibility and workflow, and reduce lower reimbursements due to missing documentation. The hospital leveraged analytics to provide actionable feedback to continuously improve the process.
Hospitals today are subject to a dizzying array of regulations and reporting requirements from public and private health payers. This makes recovering reimbursements in a timely fashion tougher than ever. For instance, if physician documentation is not present to support every treatment code perfectly, they risk financial penalties from government health programs.
On the other hand, hospitals need to quickly submit bills for payment to avoid holding up needed cash for operations. This growing tension has caused many hospitals to struggle with unmanageable DNFB caseloads, representing scores of cases where incomplete bills linger at the hospital long after the patient goes home. Ineffective DNFB management processes increase A/R days and diminish cash flow. Backlogs can represent several days of revenue—a significant amount for most hospitals.1
One challenging regulation for hospitals is the CMS recovery audit contractor (RAC) program, which was developed to prevent CMS from overpaying or underpaying hospitals for services. The RAC program enables CMS to go back to hospitals and demand repayment for any overpayments it identifies through billing audits. The ultimate goal of the program is to prevent future improper payments at hospitals around the country.2 This demonstration program ran from 2005-2008 and the full impact of the program was not felt by many hospitals until 2010-2012 as the program was phased in.
Thibodaux, like many hospitals, imposed stricter coding documentation requirements to assure it would be accurately paid for claims and avoid any overpayment claw backs. This resulted in an exponential increase in the volume of DNFB accounts, created a huge billing bottleneck as a growing number of charts were held for documentation deficiencies. Thibodaux’s DNFB load spiked from $200,000 per month to $12 million per month.
The hospital’s staff were overburdened with clearing cases, and there was no light at the end of the tunnel because they had no visibility into trends or issues that might help improve the process in the future.
Thibodaux’s leaders recognized that their backlog was a crisis and their manual process was unsustainable. They needed to find a way to speed up reimbursements and improve cash flow without sacrificing coding accuracy. They sought a solution that would quickly reduce the drain on staff resources, automate and standardize the process, and leverage analytics to provide insights that would improve the process in the future.
The hospital looked to best practices such as creating a dashboard, reviewing accounts regularly, and tracking the caseload over time—all recommended by the Healthcare Financial Management Association (HFMA)3—to help resolve DNFBs and decrease A/R days.
Thibodaux’s DNFB caseload had reached 500 per month, with about a third of patients discharged without a completed bill. These accounts could not be billed either because documentation to support all the necessary codes to draft a final bill was missing, or because the coding was incomplete, despite thorough documentation.
The medical center’s healthcare information management (HIM) staff were using a manual, weekly process to identify DNFB accounts. This process required at 8-10 hours and occurred only once a week, resulting in delays in receiving claims and staff frustration. Once accounts were identified, it would take days to gather the cases and examine each one to determine the specific deficiencies.
Staff faced additional lags even after the documentation was complete because when missing documentation had been provided, the system did not alert coders to give them the green light to finish coding and send bills for payment. Furthermore, the volume of cases was growing because the delinquency rate—the percentage of overall discharges with missing documentation—had grown to a range of 34 to 38 percent.
HIM staff were facing slowdowns as they waited for documentation on the one hand and urgency to complete bills quickly on the other. If the clock ran out, the accounts would become unbillable and forfeit all reimbursements.
The failure of the manual system to efficiently resolve unbilled accounts also hurt doctors, who were already overburdened with documentation demands. Physicians were sometimes saddled with as many as 30 cases to correct at a time. Due to delays, the patients may have long been discharged and doctors struggled to remember important details needed to fully document each case. Many times, the deficiencies in documentation required dictation and the reports had to go to transcription, causing additional breakpoints for coders. Meanwhile, hospital administrators continued the practice (at at a much higher frequency) of threatening doctors with disciplinary action if the charts were not completed on time. It was an unworkable situation for coders, providers, and administration.
One of the biggest difficulties with Thibodaux’s manual process was an inability to prioritize the oldest cases in order to make sure the clock didn’t run out for CMS reimbursement. This inability to see information impacted the efficiency of both the transcriptionists and the coders. The system also couldn’t highlight the highest-value cases to help maximize revenue. Without an effective reporting tool that enabled it to quickly identify high-priority cases, the medical center struggled to improve both the delinquency rate and the time to final bill.
Finally, without near real-time data, HIM team members were unable to analyze why the accounts were not coded. They could not look at patterns, trends, and root causes of delays or use data on uncaptured revenue to proactively motivate physicians to speed up documentations.
Thibodaux had already implemented a late-binding enterprise data warehouse (EDW) from Health Catalyst, but the hospital hadn’t applied the EDW to resolving its DNFB process woes. Thibodaux was able to leverage the clinical, financial, operation, claims, and other data aggregated in the EDW by deploying a DNFB analytics application on top of the data warehouse. This application, the HIM Documentation Workflow Analyzer, eliminated the manual process and integrated DNFB data into the hospital’s dashboard and workflow.
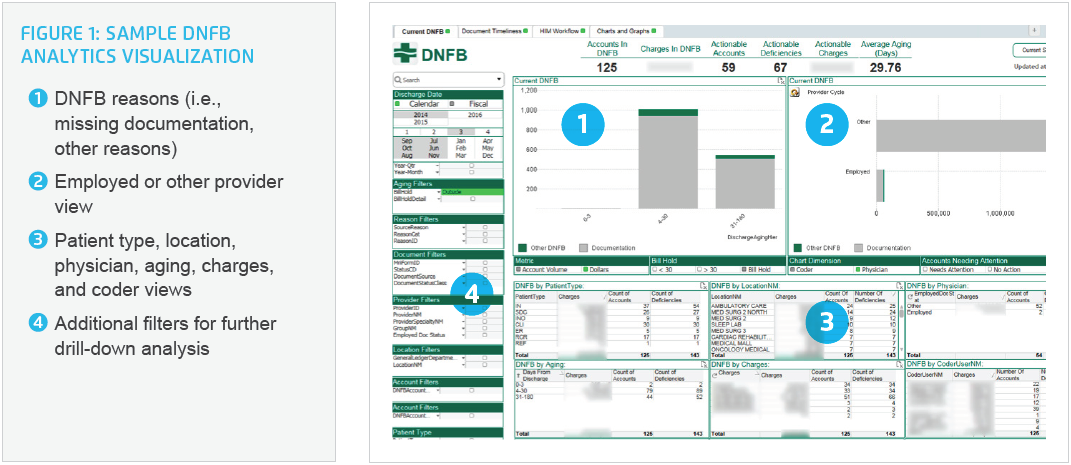
The application gives HIM team members quick and easy access to the information they need to effectively manage the entire process. They can view data by age, by payer, by reason, by patient type, by location, and by physician, enabling them to identify areas for improvement that were previously hidden (Figure 1).
This new visibility streamlines the process so coders now have the time needed to fully code each account, virtually eliminating the need to downcode cases due to missing documentation or elapsing billing time limits. HIM managers now receive very few emails about writeoffs due to accounts not being coded.
Doctors now have a greater ability to complete documentation requests in a timely fashion due to the ability to identify and track accounts more quickly and effectively. The physician portion of the caseload, representing the backlog of reports needing documentation, dipped sharply in July after the automation of the process. One clear reason: Instead of a weekly deluge of 30 reports to document—some of them related to long-discharged patients—doctors now receive more frequent, focused, and helpful information from HIM. Physicians are typically receiving one or two cases at a time, and these cases are more likely to be for patients who have just been released from the hospital, making it easier for doctors to remember and document details.
Since the physician portion is the biggest component of DNFB cases, reducing the backlog with doctors has an immediate and significant effect on the overall caseload, improving billing and decreasing days in accounts receivable.
The automated process also enables continuous improvement. For instance, physicians are better able to identify their own patterns of missing documentation. This has led to improved charting and report completion both before and after the patient is discharged. From the administration side, the integrated view of account data now allows HIM to identify individuals responsible for holding up the billing process. Since HIM can quickly quantify the dollar impact of each delay, this serves as a motivator for doctors to complete cases more quickly.
Improved visibility and more frequent access to data have transformed the workflows of stakeholders across the hospital. Leadership has access to summaries that deliver a clear view of delinquency rates, A/R days, and other key operational metrics. This gives them the tools they need to better predict and manage cash flow in a new way. Transcriptionists and coders can quickly prioritize cases based on the age of the account and the dollar value it represents. Instead of arriving at work unsure of where to start, coders open the application and are immediately greeted with cases ready to code. And for the first time, all staff working to clear cases can look at the dynamic report anytime, instead of once a week or every other week. This allows Thibodaux staff to quickly recognize trends or problems and pivot to better manage the backlog of accounts.
Thibodaux’s new analytics tool helps it identify patterns of deficiencies such as missing orders, discharge summaries, transfer papers, and history and physicals. At one point, hospital leaders found one department with significantly higher DNFB rates than others and were able to work with the department to identify and resolve process issues surrounding missing reports/information coming from the ordering departments that were contributing to their high DNFB rate. This new problem-solving capability is transforming the billing process at Thibodaux and reducing much of the pain for administrators, physicians, and staff.
Thibodaux Regional Medical Center has shown that, in less than a year, a DNFB management overhaul focused on automation and analytics can improve finances, operations, and morale. The new DNFB process has freed up HIM staff to focus on high-impact interventions, has reduced the documentation burden on doctors, and has optimized efficiency for coders. As a result, Thibodaux today finds itself in a much better cash flow position.
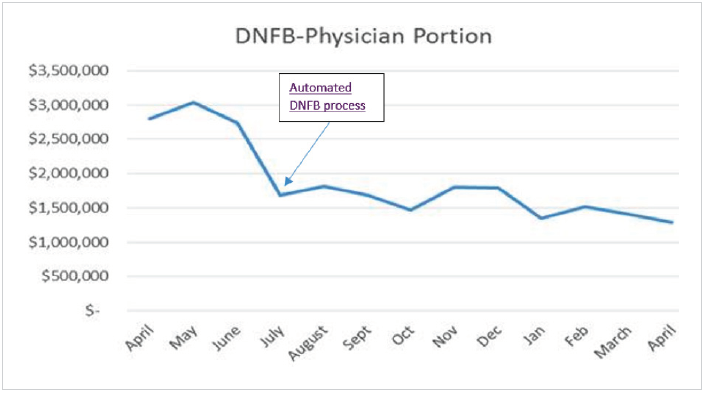
The transformation of the DNFB process has also improved morale for doctors and staff previously burdened by an avalanche of belated documentation requests. Doctors are now receiving charts daily, when they still remember the discharged patients, and are completing documentation more quickly. This has cut the physician portion of DNFB dollars in half (Figure 2).
As a result, within five months, hospital administration stopped sending reprimand letters to physicians for overdue documentation. At the six-month mark, the medical center began to leverage analytics to uncover new insights about trends and the types of missing documentation, leading to focused interventions with specific departments and providers.
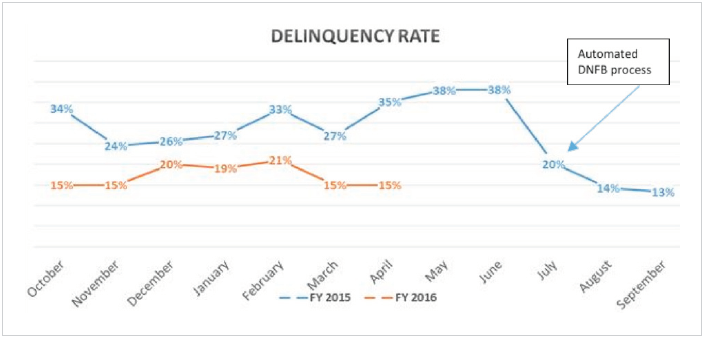
Another dramatic change has been a 50 percent reduction in the hospital’s delinquency rate (Figure 3). Thibodaux’s rate of overall discharges in DNFB status hovers around 15 percent, versus a high of 38 percent the previous June, before the automated process was implemented.
In summary, Thibodaux has made impressive improvements in several key metrics in less than one year:
Thibodaux has eliminated a cumbersome, manual DNFB process that tied up crucial revenue and unnecessarily burdened doctors and staff. The hospital continues to apply these learnings to improve the DNFB process.
"In the past, we had to rely on medical staff leadership to assist us in getting missing documentation and driving the delinquency rate down. But now, with our analytics solution, we are catching documentation gaps so early that we can intervene quickly. We don’t even have to send reprimand letters to physicians anymore.”
– Bernie Clement, Chief Information Officer
Thibodaux is well on its way to minimizing its DNFB caseload in order to ensure sufficient cash and available staff resources to deliver the best care possible. The hospital now plans to deploy similar process improvements and analytics to improve other business processes, such as coding around case mix index.
One of biggest changes for Thibodaux is that it can now quickly get bills out the door. Now, by submitting bills that fully reflect the rich array of services patients are receiving at the community hospital, Thibodaux may discover that its case mix index—which measures how sick a hospital’s patients are—is higher than previously reported. This is important because hospitals with a higher case mix index may be entitled to larger reimbursements from payers.
Following the success of the DNFB process transformation, Thibodaux plans to do an analysis on accurate coding and documentation and the impact on the case mix index. Hospital leaders will also continue to optimize processes and monitor patterns and trends to ensure that their billing advances are sustained over the long term.




