Clinical variation can be frustrating for patients and their families, and it can also lead to significant costs for healthcare systems. Texas Children’s Hospital aimed to address this by creating evidence-based clinical standards. To evaluate the effectiveness and usage of these guidelines, the organization implemented an analytics platform to effectively analyze evidence-based order set utilization.
Clinical variation can be frustrating for patients and their families, often leaving the impression that healthcare team members are not on the same page and don’t agree on the plan for the patient’s diagnosis or treatment. It is also costly—the Institute of Medicine estimates that $265 billion (30 percent) of healthcare spending is waste that directly results from clinical variation.
To reduce unwanted variation, Texas Children’s Hospital invested considerable resources to develop clinical standards tools, including evidence-based order sets; however, demonstrating the effectiveness and utilization of those guidelines, pathways, and order sets had been daunting. To that end, Texas Children’s deployed an analytics platform from Health Catalyst to aggregate and analyze the data needed to perform both of these critical functions.
In 2009, the United States spent $2.5 trillion in healthcare, with an astounding 30 percent of those dollars attributed to wasteful spending. Of the wasteful spending, unwanted clinical variation was found to be a major contributing factor, with $265 billion attributed to unnecessary services or missed opportunities for preventative care.1 Since then, there has been a sustained call for efforts to reduce such expensive waste of healthcare resources. A primary strategy is to use evidence-based clinical guidelines—which comes with the additional benefit of bringing clinicians up to speed on the latest research to guide care to deliver optimal outcomes.
Individually, it can be practically impossible to capture such knowledge. Today there are more medications, treatment options, and medical knowledge than ever before—but, even as early as 1991, a study in the Journal of American Medical Association estimated that to stay current with the general body of knowledge, a general internist would need to read 20 articles a day, 365 days each year.2 As such, healthcare organizations like Texas Children’s, ranked the best children’s hospital in Texas and among the top four in the U.S., place great value on ensuring their clinicians have access to the most recent evidence.
As part of its vision to deliver team-based, high-quality care, Texas Children’s applies evidence-based practice (guidelines, pathways, summaries) in consideration of the individual child’s needs and the family’s preferences and values. This story focuses on how Texas Children’s validates if these guidelines actually improve outcomes and the return on investment of its evidence-based practice program.
Texas Children’s strives to deliver a care experience that is evidence and consensus-based, consistently delivered across the continuum of care, without needless variation. Yet because there is less clinical research involving infants, children, and adolescents than there is in adults, delivering this care and correlating it with outcomes are particularly challenging for children’s hospitals.3 Research with adult subjects cannot be automatically extended to pediatric patient populations. Additional discussion and discernment often are required to determine appropriate use in younger patients.
Texas Children’s has an Evidence-Based Outcomes Center (EBOC) to assist with these and other decisions. Indeed, the EBOC provides a strong infrastructure for developing consensus- and evidence-based guidelines and the order sets to support them. However, there was no real way to determine which order sets and interventions were contributing to better outcomes.
Supplying clinicians with data about outcomes—a key component of reducing clinical variation—was another challenge. It was difficult to extract related information from the electronic health records (EHR) system while key data points, such as direct variable costs, didn’t exist in the EHR at all. Outcomes analysts needed weeks or months to obtain and verify all the needed data from multiple sources; correlate the findings across different data points; and then review and revise the reports until they were ready for distribution.
Monitoring order set utilization and impact on patient outcomes was, from a human resources standpoint, practically impossible. There simply were not enough hands on deck to gather the necessary data from various sources and analyze it against all the different patient cohorts.
With these challenges as the backdrop, Texas Children’s identified a number of requirements:
Texas Children’s didn’t lack for data to evaluate its various evidence-based care programs, but it did need an efficient way to access the data and present it into useful findings. To that end, Texas Children’s implemented an analytics platform from Health Catalyst. The foundation was built on a late-binding data warehouse platform that aggregated data across the healthcare enterprise.
Two powerful analytics tools for extracting usable findings from this data were Health Catalyst’s Population Explorer application for tracking and analyzing population metrics, and the Key Process Analysis (KPA) application to identify the top cost-driving clinical cohorts with the largest degree of clinical variation. These technologies effectively equipped Texas Children’s with the capabilities to use data they already had to evaluate evidence-based care—sustainably and at scale.
Texas Children’s interfaced the Population Explorer application to pre-defined registries and a starter set of 50 metrics associated with individual patient populations. Available data includes case counts, order set use, readmission rates, revenue, LOS, and resource utilization such as medications, imaging, and lab tests. Then, using automated data provisioning and sorting, Texas Children’s was able to stratify each metric by multiple demographic, geographic, clinical, and financial filters.
Texas Children’s over-arching objective was to evaluate order set utilization on outcomes—which the hospital categorized as LOS, direct variable cost, and 15-day readmission rates. These outcome categories were then used as the basis when comparing patients who had care ordered via an evidence-based order set against those patients whose care did not include the use of evidence-based order sets. Some key assumptions included:
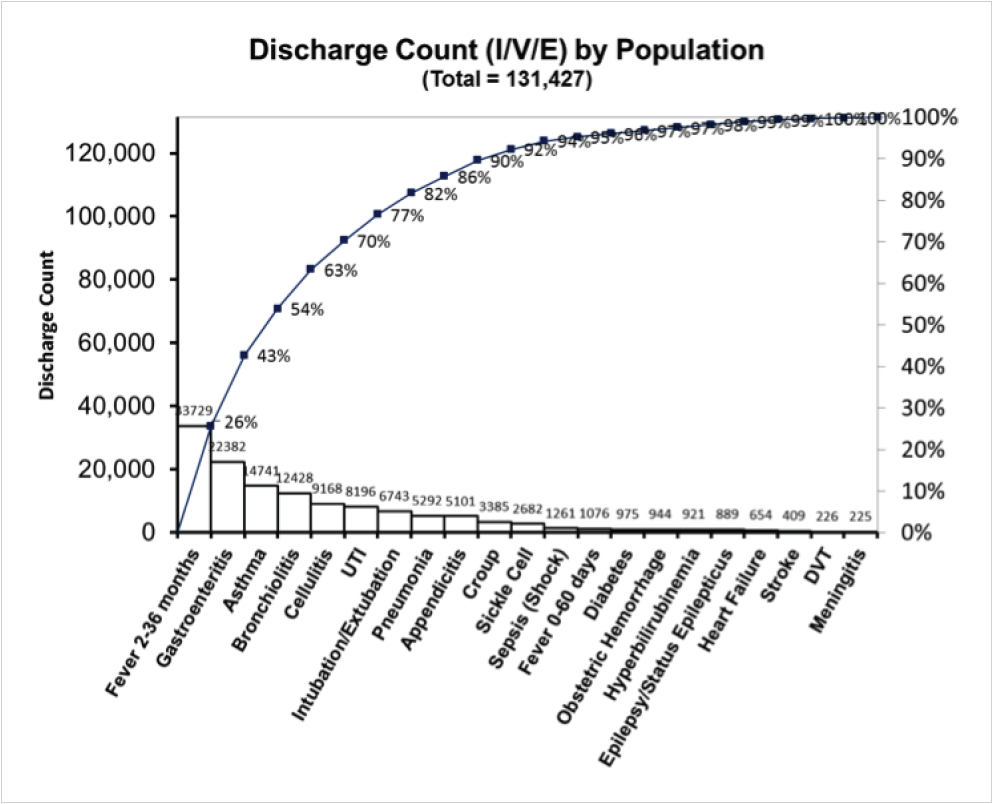
Having established the patient populations of interest, their outcomes, and the timeframe for analysis, Texas Children’s used the analytics platform to complete a comprehensive retrospective analysis of three patient categories: inpatients (I), observation patients (V), and emergency center patients (E). Within these three categories, Texas Children’s analyzed 21 distinct patient populations, plus an aggregated analysis of all 21 patient populations. Whereas this type of analysis was impossible previously, Texas Children’s completed this comprehensive, extensive analysis in only three months.
For the first time ever, the EBOC at Texas Children’s was able to efficiently analyze EHR order set utilization, and the impact of EHR order sets utilization on LOS, direct variable costs, and 15-day readmission rate, calculating an ROI and benefit cost ratio (BCR) for the EBOC and clinical standards (see Figure 1).

As a result of the evidence-based order set utilization in the 21 analyzed high cost/volume, complex conditions like diabetes, sickle cell, and sepsis (see Figure 2), Texas Children’s has been able to demonstrate that its evidence-based order sets have a significant and positive impact.
“For years, we would look to the evidence and implement important changes in practice with the goal of improving outcomes, but we lacked the ability to get any data about our performance. We couldn’t evaluate if the changes were incorporated into practice, and couldn’t evaluate if the changes were having a positive impact on outcomes. We now have a data platform that can be made widely accessible and works. It is now wonderfully simple.”
– Terri Brown, MSN, RN, CPN Clinical Specialist
With such results at hand, Texas Children’s EBOC team will work toward a goal of improving usage rate for all available order sets. To achieve this, Texas Children’s will use content expert teams and the EBOC to develop and refine clinical standards to align with the current, evidence-based body of knowledge. Additionally, through 2016 and 2017 the EBOC will focus on the enhancement of clinical decision support in the EHR, with a particular concentration on potentially preventable events. This initiative will include work to improve diagnostic accuracy and therapeutic effectiveness, and reduce test over-ordering.
Now that providers can actually see the impact of order set utilization on patient outcomes and cost, Texas Children’s is confident that order set usage rate will increase. To help drive that increase and understanding, the data and insight gained from the advanced analytic application will be pushed out to physician section chiefs, designated quality liaisons, practice administrators, and nursing leaders. Finally, Texas Children’s is rapidly expanding access to Population Explorer to give more pediatric clinicians the tools to reduce clinical variation—and improve outcomes for the most vulnerable patient populations among us.