ACOs must report data annually to assess quality performance, impacting shared savings eligibility. Read how Mission Health implemented a proactive, data-driven approach to measure and evaluate performance, enabling the organization to sustain and further improve its performance across multiple ACO measures.
On an annual basis, Accountable Care Organizations (ACOs) are required to accurately report data that is used to assess quality performance. This is necessary in order for the ACO to be eligible to share in any savings generated. Improvements in measure performance are often linked with ACOs that have offered providers the skills, tools, and data required to understand and track their own performance, as well as that of their peers.
Mission Health, based in Asheville, North Carolina, is the state’s sixth-largest health system, spanning the 18 counties of western North Carolina. Mission formed one of the largest ACOs in the country, Mission Health Partners (MHP), providing services for nearly 90,000 patients. Mission’s primary care practices are the largest group within MHP and desired to lead the region with population health. While MHP had previously achieved success in improving its ACO measure performance, it sought to increase its quality scores even higher. Without access to transparent, actionable data, leadership was unsure if improvements would be sustained, let alone if existing workflows could lead to new improvements. After developing a comprehensive plan that included a massive expansion to data access, Mission practices were able to sustain initial improvements, identify new opportunities, and improve population health quality even further.
These improvements have contributed to MHP being recognized as one of the best ACOs in the nation, with the organization recently earning a MIPS quality score of 49.9 out of 50 points. The organization has saved Medicare over $11 million beyond its target, despite having one of the lowest spending benchmarks in the nation. In addition, Mission recently achieved a 5-star rating from CMS for its two largest hospitals. Mission has been named one of the nation’s Top 15 Health Systems—one of only two hospital systems in the U.S. to receive this award for the sixth time in the past seven years.
Each year, ACOs are required to accurately report data that is used to calculate and assess its quality performance. In order to be eligible to share in any savings generated, an ACO must meet the established quality performance standard that corresponds to its performance year.1 Quality is assessed based on thirty-four individual measures of quality performance, spanning four quality domains: patient experience of care, care coordination/patient safety, preventive health, and at-risk patient populations.
Organizations who offer providers the skills, tools, and data to understand and track ACO measure performance have experienced more engaged provider support and involvement with improvement efforts.2
Mission formed one of the largest ACOs in the country, MHP, providing services for nearly 90,000 patients. Covering 58,000 Medicare beneficiaries, it includes almost 1,200 physicians spanning the 20 counties of western North Carolina. Mission’s community medicine practice has over 87 physicians and advanced practitioners providing care in 19 clinics across the region.
While MHP had previously achieved success in improving its ACO measure performance, the coming year brought even higher benchmarks than ever before, and Mission practices were eager to obtain actionable information as promptly as possible to engage patients.
Provider and staff access to the data needed to monitor performance effectively was limited. Some clinics only received data on their performance as a group aggregate at the end of the month. Other clinics only had one user with access to the data, but reliance on one person inadvertently led to the delayed communication of measure performance, decreased awareness about how to use the analytics application, and limited understanding of how to use the data available for improvement efforts. A lack of direct access to the analytics application made some providers skeptical of the data, citing concerns over its accuracy. Though there were many high performing providers in the system—because of the lack of transparency—other providers were under the impression that the performance goals were not attainable and could not identify which colleagues could help provide targeted coaching.
Various stakeholders desired different levels of information about performance, and Mission practices initially lacked the structure and data required to communicate performance in a timely manner. Mission needed a comprehensive approach to engaging providers in ongoing improvement efforts in order to sustain and further improve its performance.
Mission developed a comprehensive plan to drive further improvement, ensuring its patients receive the right care at the right time. The organization developed an extensive approach to engaging providers in a meaningful way, aiming to improve ACO measure performance and patient outcomes. Its efforts focused on improving data transparency, providing ongoing communication and education, and sharing the responsibility for improvement.
To support the monitoring and managing of actual performance against the Centers for Medicare and Medicaid Services (CMS) required measures for ACOs throughout the year, Mission utilized the Health Catalyst® Data Operating System (DOS™) Platform and leveraged the ACO MSSP Measures analytics application that it had previously implemented. It expanded access to the analytics application, ensuring physicians, advanced practice providers, registered nurses, medical assistants, practice managers, and executives all had access to the analytics application.
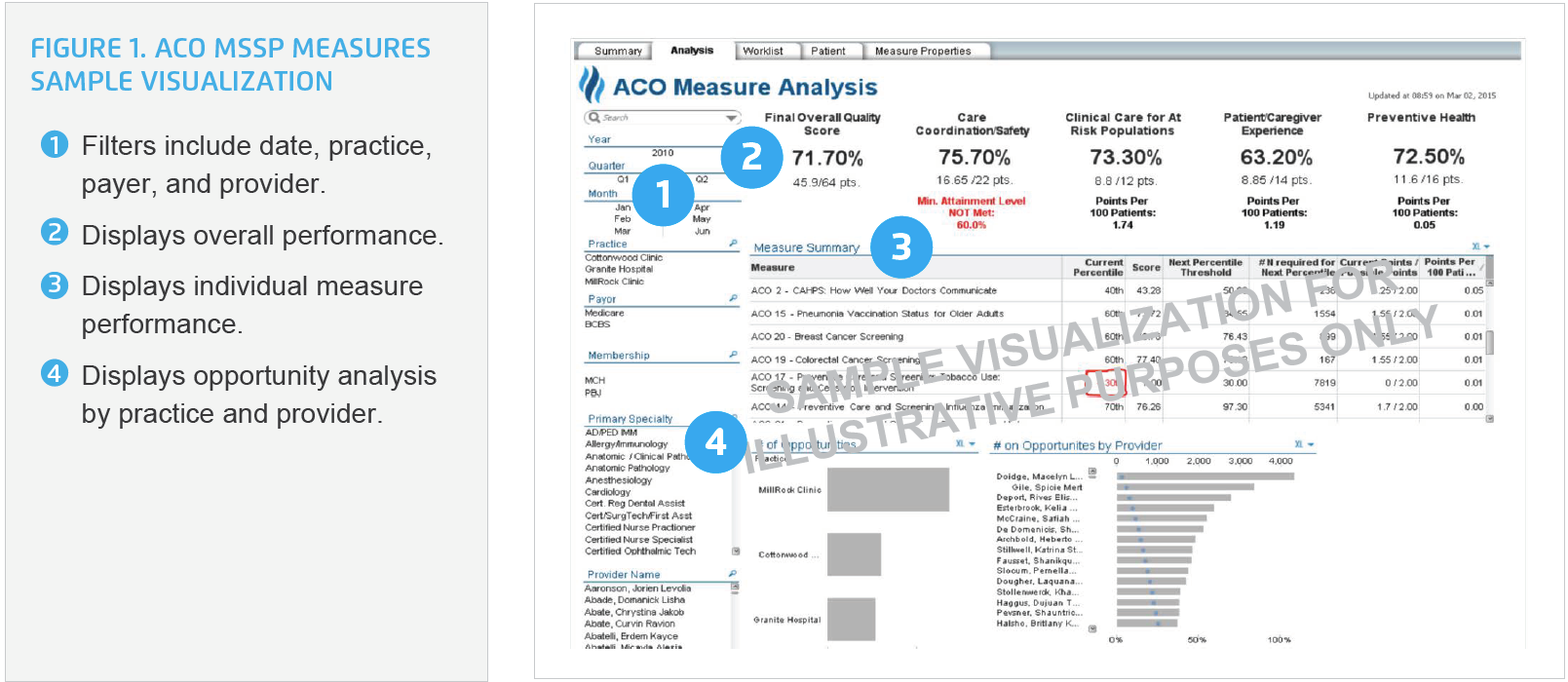
Providers and practice managers now have the ability to measure their individual and clinic performance, allowing them to drill down into each measure at any time, identifying inefficiencies and opportunities for improvement prior to the required reporting deadlines. This represents a critical advantage given the dollars tied to an ACO’s performance against the CMS measures (see Figure 1).
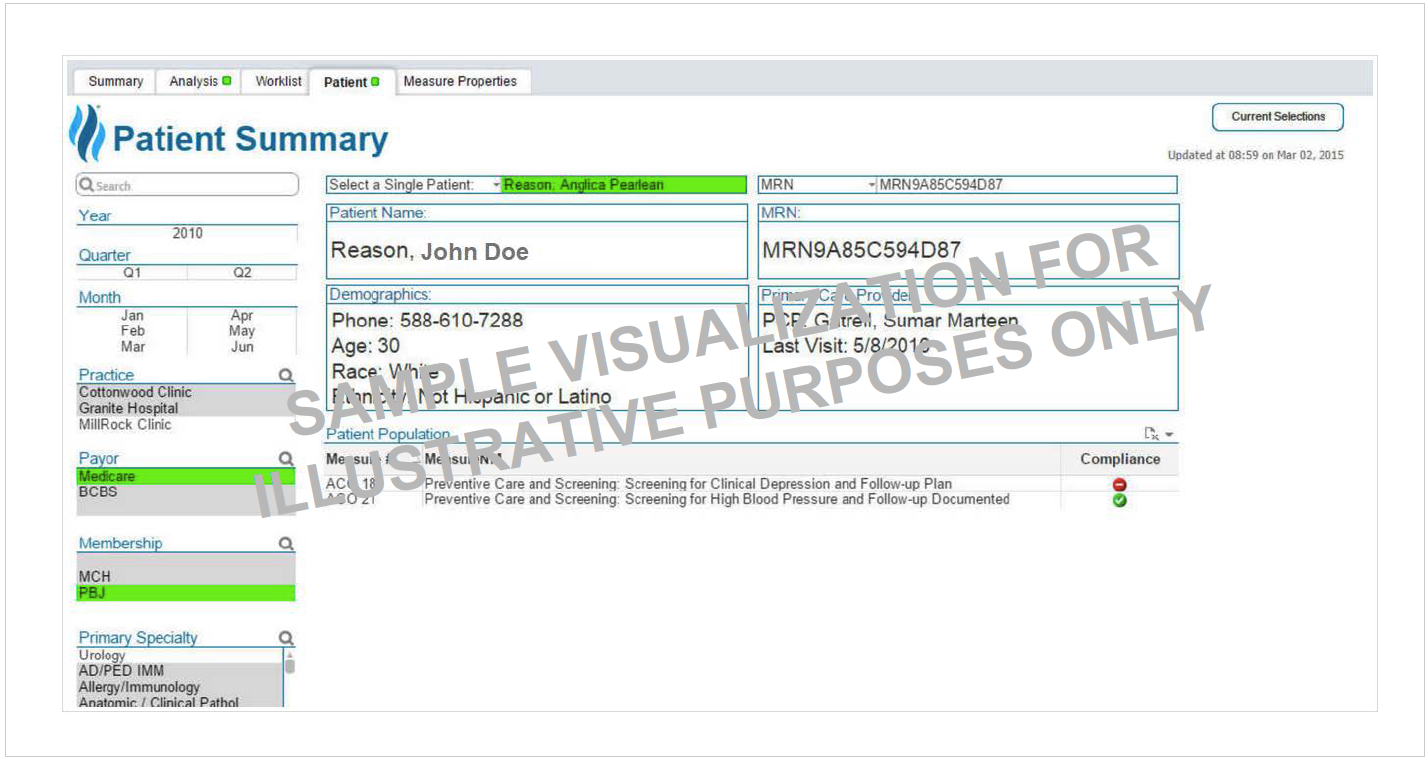
Providers and medical assistants use the analytics application before the patient is seen to identify which measure opportunities have not yet been addressed and ensure the right care is provided while the patient is in the office (see Figure 2).
By using the analytics application, targeted visualizations of performance are generated to meet specific audience needs, addressing performance and improvement efforts, including:
Personalized education is offered to all providers who use the analytics application, including a demonstration on how to use filters to visualize the data of interest, how to create bookmarks for frequently accessed information such as individual performance data, and how to view a comparison of the provider’s individual performance against that of their peers.
The analytics application is used to identify potential knowledge gaps. For example, one clinic noticed that compliance for BMI counseling and follow up was very low, despite the providers having provided the appropriate counseling. Clinicians and leaders used the analytics application to conduct a deep dive into the data and discovered documentation was not saved correctly, negatively impacting measure performance despite the patient having received the right care. Mission was able to correct the error, clarifying the source of the documentation for the measure and the correct procedure for saving documentation prior to reporting measure performance.
Data-driven education has helped improve confidence in the data, allowing leaders to use the analytics application to evaluate the effectiveness of the education on performance, enabling timely feedback to providers, and the ability to adjust the education plan if it is not resulting in the desired outcomes.
Mission used a team approach for engaging providers, refining standard workflows, protocols, and documentation, all with the goal of ensuring that patients receive the right care and that all care provided is documented correctly.
Providers, medical assistants, and practice managers use peer-to-peer learning to share ACO measure expertise within their clinics and with other clinic practices which helps to create a culture of shared responsibility for improving patient outcomes. Providers are now able to see which of their peers have achieved the highest performance, so that they may reach out to gain insights that can be used for continuous improvement.
The visualizations from the analytics application are shared during weekly office meetings. This gives providers the ability to review each measure, compare performance to the previous week, and use an iterative cycle to validate data and improve performance prior to reporting internally or externally. Key stakeholders, including executive leaders, now have access to the data they need to monitor and manage organizational performance and obtain meaningful, timely data.
This proactive approach including widespread adoption of analytics and shared responsibility for ACO measure performance has allowed Mission to sustain and further improve its performance. By expanding access to the analytics application, utilization has tripled, and 369 health system users currently access the tool. These improvement efforts have helped Mission achieve:
Improved preventative care and screening, including:
Improved preventative health and clinical care for at-risk populations:
Improved cardiovascular measures, including:
These improvements have contributed to MHP being recognized as one of the best ACOs in the nation, with the organization recently earning a MIPS quality score of 49.9 out of 50 points. The organization has saved Medicare over $11 million beyond its target, despite having one of the lowest spending benchmarks in the nation.3 A focus on providing the right care to the right patients at the right time is positively impacting patient lives and bringing satisfaction to the care team.
By using the analytics application, Mission identified that breast cancer screening performance was lower than desired. As a result, Mission practices focused improvement efforts on increasing patient awareness about the importance of mammograms—proactively reaching out to patients who had not yet completed a mammogram. During one patient’s visit to the clinic, the care team identified that the patient had not yet received the recommended mammogram. The team successfully scheduled the patient for a mammogram the same day, which revealed that the patient had early breast cancer. Without access to patient-specific data in the analytics application, lifesaving treatment would have been delayed. This example highlights how ACO measures and shared responsibility for improvement impact patient outcomes.
“Sharing data with providers has inspired adoption of best practices. Combining transparent analytics with our clinics’ spirit of creativity in patient outreach is improving outcomes and saving patients’ lives.”
– Christina VanRegenmorter, MSSW, PMP, Manager of Provider Quality Reporting, Mission Health System
Mission is focused on continuing its high performance as one of the best ACOs in the nation. The analytics application is being used at specialty practices that are not required to report ACO measures, such as neurology providers, and those providers are actively using the analytics application to identify patients who could benefit from improved blood pressure control, fostering the spread of best practice preventative care to improve patient outcomes.