
$2.3M in cost savings
in 12 months, the result of a 9.1% relative reduction in PMPM costs


Transform value-based care insights into actionable and timely patient interventions with the Health Catalyst Population Health Suite™.
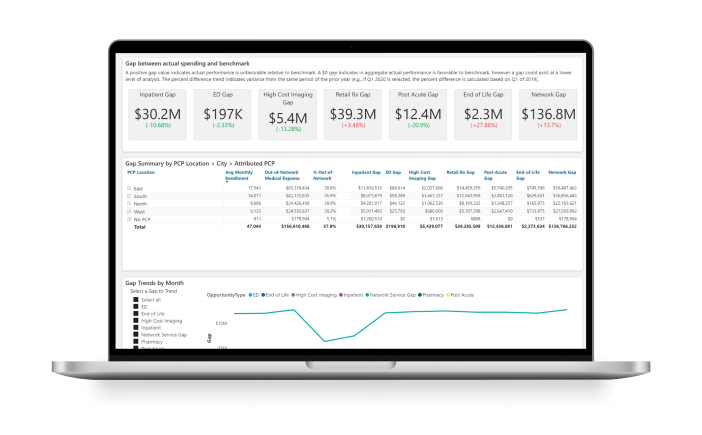
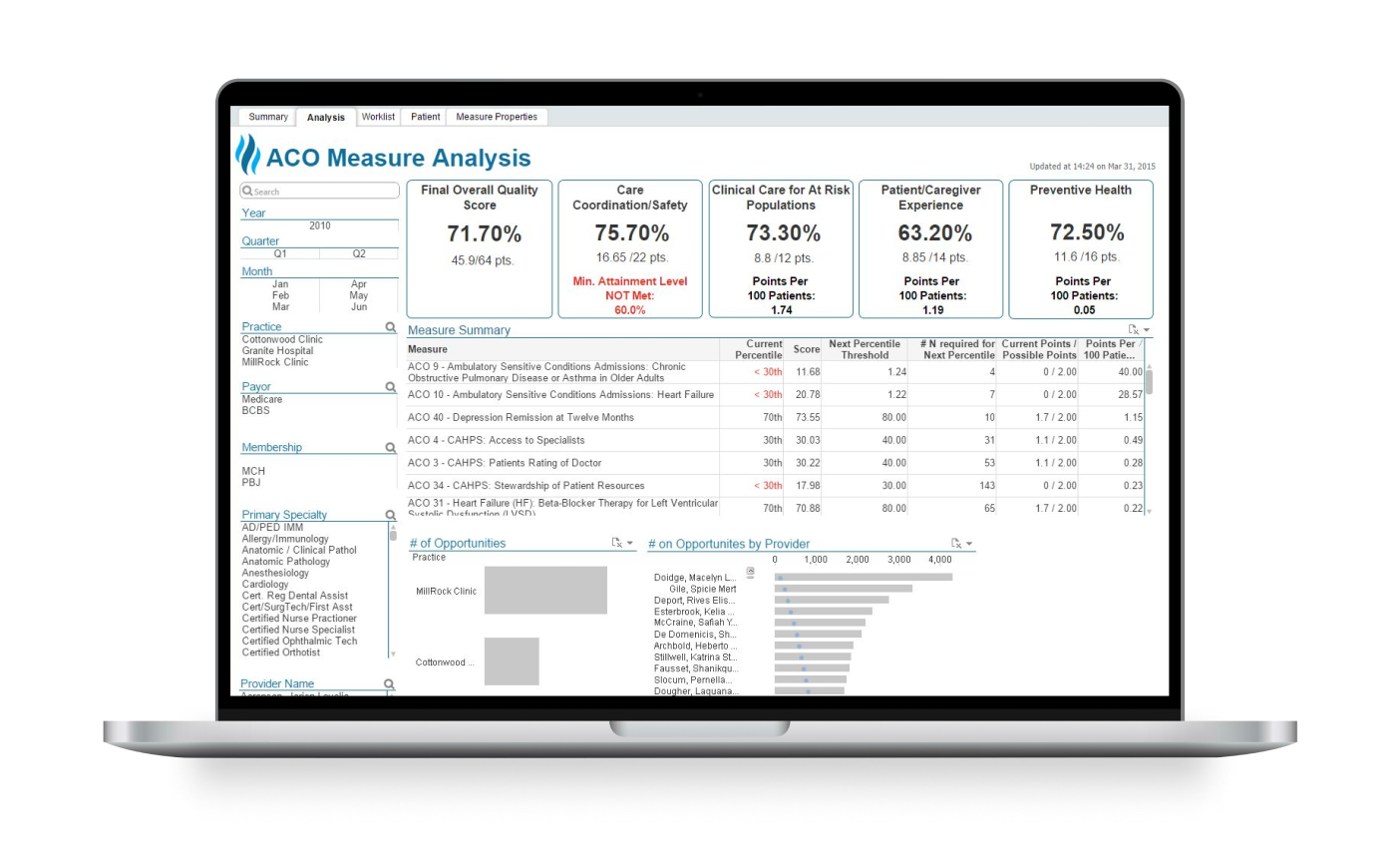

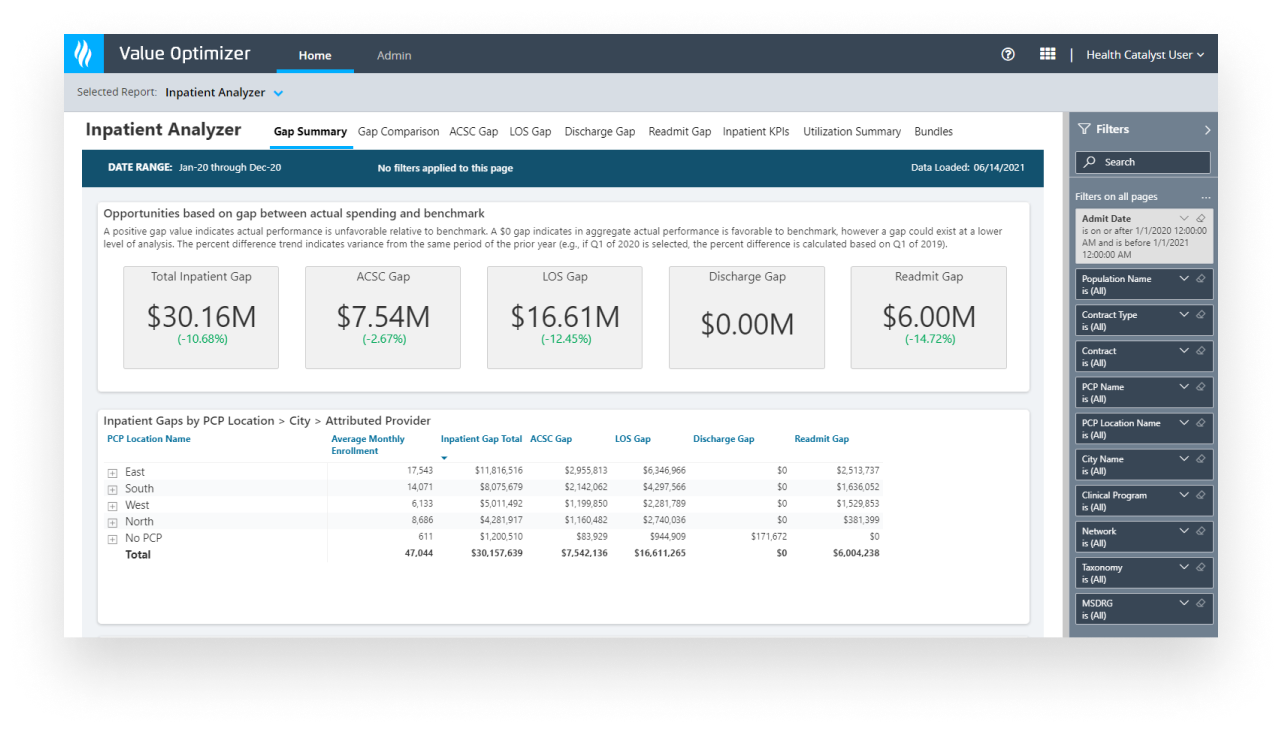
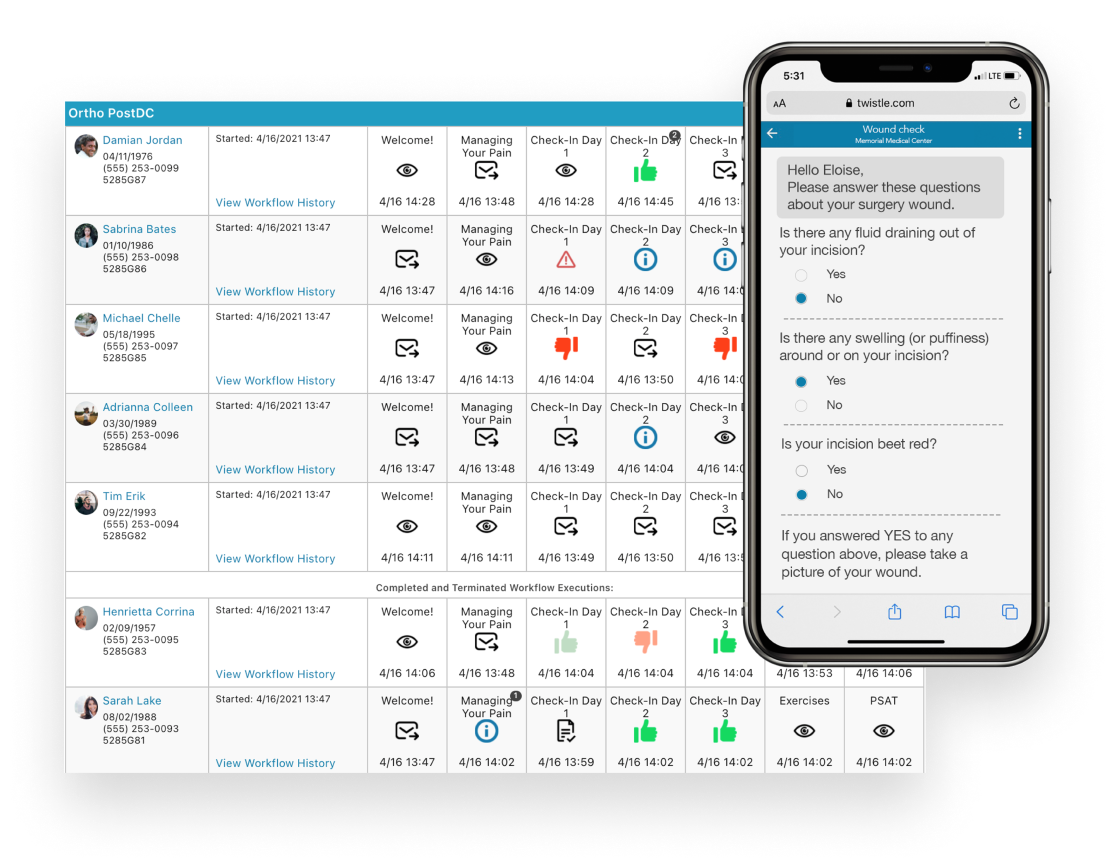

Our Population Health Strategic Consulting team can help you tailor analytics to meet your organization’s unique population health needs.

in 12 months, the result of a 9.1% relative reduction in PMPM costs






This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.