6 Proven Strategies for Engaging Physicians—and 4 Ways to Fail
The United States leads the world in healthcare spending, devoting almost 18 percent of its gross domestic product to healthcare costs—and that percentage is slated to continue rising. But this financial burden is not sustainable. In an effort to reduce the overall strain on the government, CMS has tasked healthcare systems to provide higher quality care, decrease costs, and improve outcomes as rapidly as possible.
Making significant improvements is not an achievement organizations can do without physician engagement, though. They need physicians to be on board. Why? The reality is that physicians play a large role in the complex mechanisms of healthcare delivery. From providing frontline care to filling leadership positions, physicians drive 75 to 85 percent of all quality and cost decisions. That’s a mighty large percentage, which translates to significant financial losses if physicians are disengaged and don’t participate in improvement initiatives.
A survey by Gallup highlights the importance of engaged physicians: for one hospital alone, there was a 26 percent increase in productivity for engaged physicians over disengaged physicians. In other words, one engaged physician adds an average of $460,000 in patient revenue per year. Not a source of revenue to ignore when many health systems only have about two
percent operating margins to work with these days.
4 Barriers to Physician Engagement
To obtain high levels of physician engagement, it is important to understand why some physicians are reluctant to participate in the quality improvement process.
First, because of recent regulatory changes, physicians are preoccupied with concerns about losing their autonomy and seeing a drop in income levels. They are also struggling with increased patient loads and dealing with the onslaught of new regulations and requirements—all without any guidance on how to survive the new value-based care environment. A McKinsey report highlights four other key concerns and barriers:
- Physicians feel overwhelmed and ill-equipped to implement change. They also lack an understanding of how their behavior contributes to healthcare waste and inefficiency.
- Hospitals and payers believe that employing physicians is the primary means of securing alignment. Instead, a holistic approach by combining multiple alignment levers (e.g., personal autonomy, clinical autonomy, colleagues, IT department) would be more effective.
- Organizations have the misconception that compensation is one of the most important drivers for physicians.
- Physicians have a poor understanding of the risk-based payment model along with being risk-averse.
Because of the many uncertainties facing physicians, it’s easy to understand why so many feel anger and sadness right now. More information about the various stages of grief physicians are experiencing can be read in this Harvard Business Review article.
Encouraging Physicians to Play a Positive Role During Times of Change
So how does a health system encourage physicians to play a positive and constructive role to drive cost and quality improvement initiatives? One key method is for the organization to send the message they want to focus on improving patient care. An objective like this has more value to physicians than goals to reduce costs and improve standardization and waste.
In addition, physicians and the healthcare system must share a noble purpose. Hospital administrators must acknowledge the journey will be difficult and there will need to be sacrifices along the way. Administrators must also convey their willingness to support the physicians for the long haul, provide clear expectations about why change is necessary, and give physicians time to agree with the rationale for the change. In addition, it’s important physicians receive clear messages about what is expected from them during the change process.
Dos and Don’ts for Effective Buy-In Strategies
While there are different types of strategies an organization can use to encourage physician buy-in, some have proven to be successful while others simply don’t work.
Strategies that don’t work
- Inspirational speeches. Speeches can be great for a kick-off but the words from the speech will soon be forgotten.
- Appointing physicians to key leadership positions. This isn’t necessarily the wrong approach, but if a health system puts a physician in a leadership position, he or she needs to be trained. Without this training, the physician won’t be able to effectively organize everybody else around them and be a compelling leader.
- Financial incentives. Sure, physicians want to be paid for their time, but by and large, physicians are an altruistic group of folks. Plus, if the sole encouragement to improve care is financially motivated, that’s not the best approach.
- Sharing of best practices. While it’s good to share best practices, it can be overwhelming to share each and every best practice that comes along, especially when caregivers are already so busy providing patient care.
Strategies that do work
Having great leadership and creating a focus on a shared vision are critical components to encouraging physician buy-in. Rather than viewing healthcare’s problems as just that—problems—they should be seen as challenges that can be overcome. To do this effectively, someone needs to come along, point out the vision, and then lead the physicians in the right direction.
In addition to great leadership, physicians also need to see the organization as a partner, a partner they can believe in. A partner that will help them. A partner that will not only work to improve the lives of their patients, but all of the lives the organization comes into contact with, including the lives of the physicians. According to research by Gallup, a healthcare partner like this will foster physician engagement by giving physicians the following: confidence the health system can be trusted to deliver on its promises; the belief the health system will act with integrity and treat them fairly; a clean and efficient facility they can take pride in; and a workplace they can be passionate about.
6 Steps to Gain Physician Buy-in
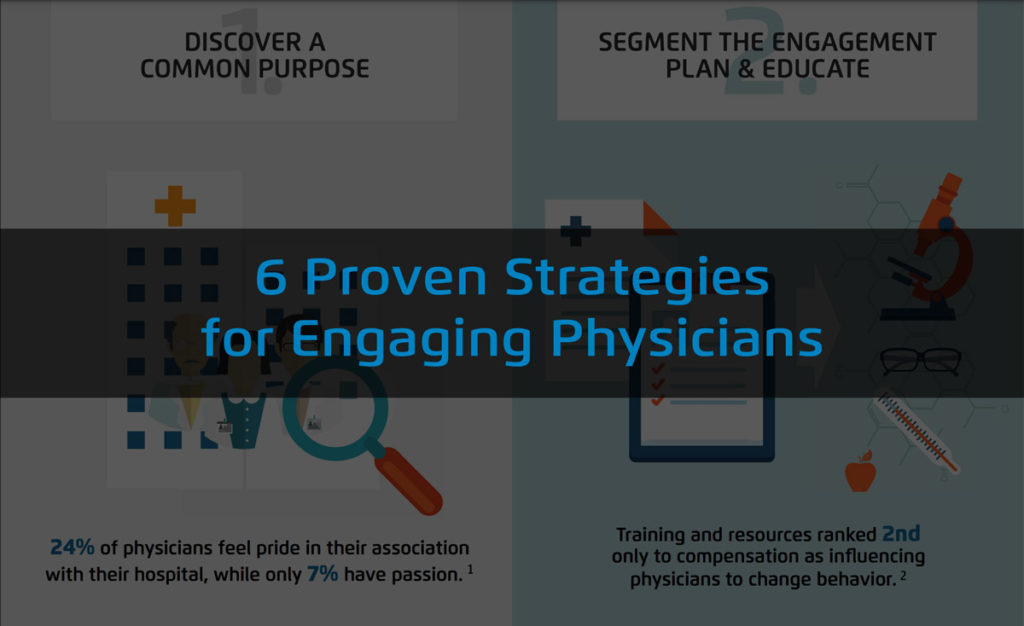
Without a plan, a strategy to gain buy-in can be difficult to achieve. The Institute for Healthcare Improvement put together a framework of six elements to encourage physician buy-in for a shared quality agenda. The framework covers the following objectives and explains why they are important:
- Discover a common purpose. This forces cultural shift where everyone in the organization begins to think as a system instead of in silos. But not all systems are ready for such a significant shift, which is why it’s helpful to first complete an Improvement Readiness Assessment.This is a systematic analysis of an organization’s ability to achieve and sustain performance improvement based on a three-system approach. The results may show there’s a lot of mistrust that needs to be overcome before the entire organization can unite under a common purpose.
- Adopt an engaging style and talk about rewards. Identify early adopters, the real physician leaders, and present this new leadership role as a career opportunity for them. This makes it easier to talk about other rewarding efforts they could expect to see, such as a clinician or administrator promotion track and the maintenance of certifications. And then communicate candidly and often.
- Reframe values and beliefs to turn physicians into partners, not customers. Include physicians in the decision-making process. For example, let physicians lead the planning phases and the teams that are responsible for implementing specific quality improvement initiatives. Then charge them with building the quality program and prioritizing improvement efforts. Also, engage their intellect. Children’s Hospital of Wisconsin engaged their physicians by using an analytics application called the Key Process Analysis application. The application enabled the neonatology group to dive deep into their data to isolate certain conditions where there was truly variation in care versus variation inherent in the patients they were taking care of. But the physicians needed to be allowed to participate in that dialogue together and go through the data to validate it themselves.
- Segment the engagement plan and provide education. Go ahead and identify champions for the quality improvement initiative. Find the frontline folks who are seen as leaders in terms of the care they provide. Then educate them about the goals for the improvement efforts. Also, provide them with the support and training they will need to gain quality improvement skills.
- Use “engaging” improvement methods by using data. One of the key pieces to increasing physician buy-in is to use data sensibly and focus on system performance objectives first. Then make it easy to try an improvement effort that doesn’t need to be perfected in the beginning. Physicians are perfectionists. But if the health system can show the benefit to making improvements in a safe manner, even if the improvements haven’t been perfect yet, physicians will realize that quality improvement is an iterative process. With this approach, physicians learn it’s okay to fail, but fail quickly, so they can learn and make adjustments to improve. For example, North Memorial Healthcare adopted an enterprise data warehouse (EDW) with visualization capabilities to enable physicians to get near real-time answers to their clinical quality improvement questions. The physicians could then see how their decisions affected length of stay (LOS) and how specific changes in clinical processes would improve LOS. By accessing the data, it was easier to convince the physicians to make the needed changes.The bottom line with this approach: the more physicians can be made to feel that change is their idea, the faster they’ll get on board.
- Show courage and provide backup all the way to the board. Let physicians know the CEO will take their improvement plan suggestions to the board for approval, and the board and CEO will understand this is a physician-led initiative.
Developing an Action Plan for Your Healthcare Organization’s Cost and Quality Improvement Efforts
Improving the delivery of care and reducing costs are critical in today’s world of value-based care. But achieving these improvements requires physician buy-in because their decisions drive the majority of quality and cost outcomes. It’s critical to create a shared vision that aligns the health system and the physicians. Then provide the administrative support, data analytics and reporting, and the training necessary to do meaningful improvement work. Listen to their concerns and address them. Actions will always speak louder than words, so make your actions speak wonders to your physicians as a way to develop a relationship of trust. Once you have their trust, you’ll get their buy-in and enthusiasm to move forward with quality improvement efforts that will benefit everyone. This will enable the organization to achieve success during an era of massive changes to its industry as a whole.
Are you also facing physician engagement challenges as you implement quality improvement efforts? What have you done to improve these vital relationships?
Presentation Slides
Would you like to use or share these concepts? Download this presentation highlighting the key main points.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

