

With increasing national costs, inconsistent quality outcomes, and an exploding wealth of health data, health information exchanges (HIE) are at an inflection point when it comes to value-based care.
This is evident on the stakeholder side with growing demand for technology to reduce reporting burdens and support improved performance. The same holds true for streamlining internal processes, which often involves HIE staff decoding large amounts of data between stakeholders and evaluating the data’s quality and completeness. A good example of the two-way demand is HIE readmission analytics, which leverages technology and delivers it in an innovative way for hospitals to evaluate quality performance and optimizing their improvement strategies. For HIEs, it is the easy decision because it has great marginal utility – meaning with minimal investment, you can provide tremendous value.
Decreasing readmissions remains critical for three convincing reasons:
Costly Impact. They are costly to the system with $4.4 billion dollars being attributed to readmissions. Proponents of cost prevention strategies are well intentioned but value-based care programs that aim to decrease readmissions are designed for interoperable organizations. The truth is that no health care setting – payers, providers, hospitals – is entirely interoperable.
System Ineffectiveness. A growing body of evidence suggests that nearly 25% of readmissions are preventable. Experts believe readmissions are the result of many confounding variables like ineffective hospital discharge processes, coordination issues between providers and poor education strategies. “Retakes” in care delivery are impactful to a system that is looking to orient to proactive, precision medicine.
Value-based care alignment. As readmissions is a targeted area of performance, there is wide usage of this measure in various value-based programs, including NCQA’s Health Plan Accreditation/HEDIS, CMS’s MIPS and Hospital Readmissions Reduction Program to name a few. Performance metrics and payment adjustment provide the infrastructure for hospitals to improve. In healthcare, where the priority constantly evolves, performance metrics hold leadership, providers and teams to objectives that keep them focused on improving performance in the right areas.
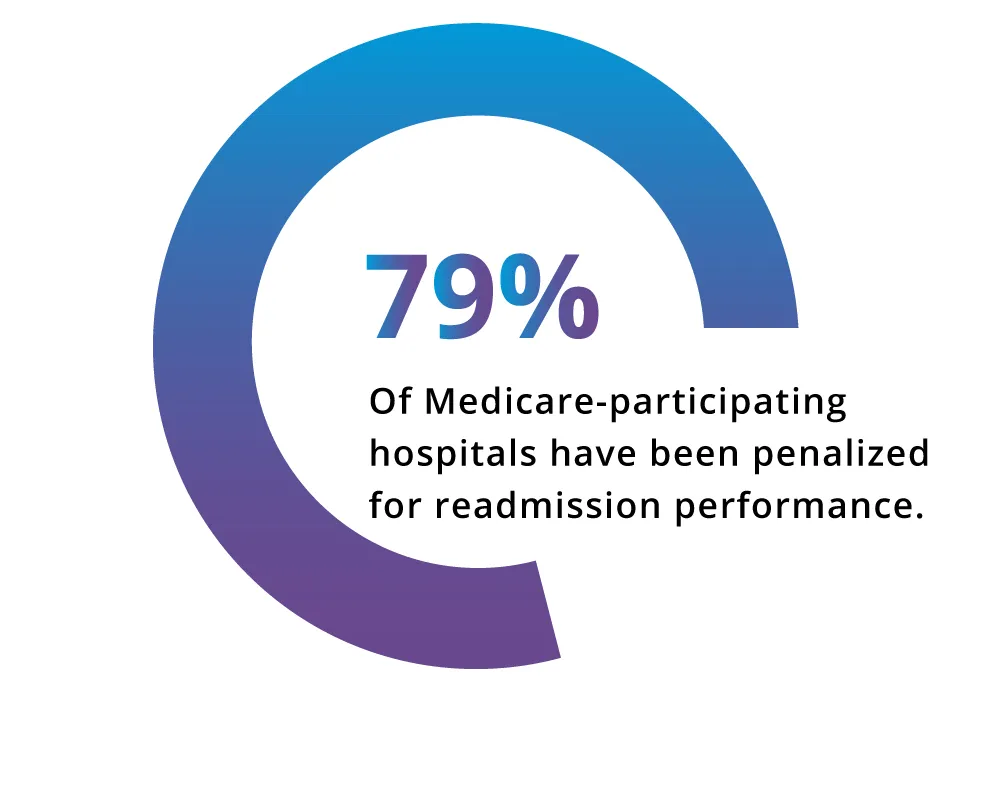
Performance can always be better
HIEs have unique positioning to support hospital systems with readmission reduction:
To appropriately risk stratify a patient, we need all, if not most of the health data associated with that patient. Often, there is a good proportion of patient data missing when viewed only from the hospital’s dataset. One commonly used tool used to predict the rate of readmission within thirty days of discharge is the LACE Index for Readmission. The tool’s algorithm considers a patient’s length of stay, acuity of admission, comorbid conditions and emergency department visits. With a limited view of only one’s health system data and the dependency on emergency room visits, this tool may not truly capture the risk a patient poses to returning to the hospital. HIEs can fill this gap by providing a comprehensive views of health and utilization across care settings to assure teams are focused on the highest risk patients and apply appropriate interventions (primary care follow-up visit, medication adherence, etc.).
Speaking of comprehensive views, many health care teams struggle to understand the magnitude of their readmissions and the drivers of poor performance. Tracking data provides information to spot trends and determine the impact improvement cycles are having on readmission rates. It is incredibly difficult to make a well-informed decision and make meaningful improvement when it is known that not all patients return to the same facility to receive care.
For those readmissions that bounce back to the same facility, there is an opportunity to interview patients and use this information to improve care processes and analytic algorithms to prevent future occurrences. For readmissions that seek care at a different facility, there is the opportunity to coordinate with the facility and the patient to prevent communication and care gaps.
Readmissions is a systemic problem. Having a representative view of performance is foundational to analyzing trends and making well-informed decisions regarding how to improve care. While we have discussed the hospital-perspective of readmissions, you can improve the velocity at which you deliver value to other stakeholders such as payers, clinics, ACOs, CINs as they participate in value-based contracts that motivate them to decrease readmissions as well. Readmissions analytics is just one of a suite of population health analytics that KPI Ninja offers to help you deliver value to the diverse set of member organizations and create sustainable revenue streams.
References
Psotka, M., Fonarow, G., Allen, L., Maddox, K., Fiuzat, M., Heidenreich, A., . . . O’Conner, C. (2020). The hospital readmissions reduction program nationwide perspectives and recommendations. JACC: Heart Failure, 8, 1-11.