Surviving on thin operating margins means health systems must maximize every financial earning opportunity. To identify threats to the revenue stream, organizations need access to precise, accurate costing information. An activity-based costing (ABC) system leverages patient resource utilization data to reveal exactly how much it costs to deliver care. Unlike traditional costing systems that provide average cost estimates for services rendered, ABC includes five benefits that help systems understand the cost for every aspect of the care delivery process:
1. Comprehensive costing data.
2. Ease of use.
3. Precision and accuracy.
4. Near real-time analytics.
5. A proactive cost strategy.
 Download
Download
Effective financial management ensures health systems have the resources to carry out every aspect of care delivery—from billing a patient’s insurance provider to performing a CT scan. Without solid financial standing, health systems risk cost-cutting pressures that prevent them from providing the best care to their communities. Furthermore, new financial hurdles, including the pandemic and its aftermath, emerging competitors, and a shifting healthcare market, make sustainable financial health increasingly critical.
Despite evolving financial challenges, many organizations still rely on outdated costing strategies, such as the relative value unit (RVU) and cost-to-charge ratio (RCC) methodologies. Such older approaches will not suffice in today’s fiercely competitive healthcare climate, as they don’t provide detailed cost information—the critical insight to steer financial decision making in tumultuous times.
To maximize already-thin operating margins and recover lost revenue from the spring 2020 suspension of elective procedures, health systems should use an activity-based costing (ABC) system, such as the Health Catalyst CORUS® Suite. ABC provides a comprehensive analysis of every cost driver in the care delivery process, allowing health systems to see the real cost of providing care, not just estimated or allocated costs.
Even before the pandemic, health systems typically survived on small operating margins. Now even smaller due to COVID-19, shrinking operating margins face additional threats, such as the following:
Outdated costing systems (e.g., RVUs and RCCs) assign an average cost estimate to different parts of the care continuum. An ABC system leverages accurate patient resource utilization data to understand—at an individual patient and clinician level—how much it costs to deliver care.
The ABC methodology provides five major benefits for health systems:
Historically, health system leaders (e.g., CEOs and CFOs) were responsible for financial performance, even though clinicians had the biggest impact on cost (e.g., clinicians determining a patient’s length of stay). Because older costing systems lacked the infrastructure to connect financial data to clinical data, hospital administrators couldn’t understand and effectively manage their providers’ clinical costs. Activity-based costing combines a health system’s financial and clinical data so organizations can see clinical costs to accurately identify clinical practice variation.
With clinician-specific cost profiles, providers can see their actual cost consumption and how their performance compares to their peers (Figure 1). This transparent costing information can incentivize providers to improve performance and decrease costs.
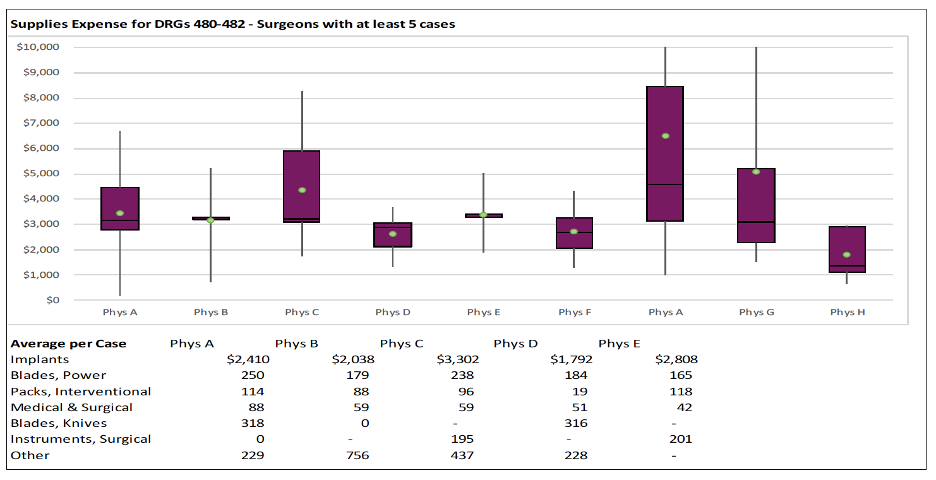
Figure 1: An ABC expense chart of performance by surgeon.
ABC is easier to maintain and implement compared to other costing methodologies because it was built with the EHR in mind. Traditional costing systems were developed before the EHR and thus lack the infrastructure to access valuable operational data recorded in the EHR. This outdated approach leaves financial decision makers with a fragmented view of cost information and reliant on averages and allocations.
As an updated cost management approach, ABC considers the EHR a critical source of operational information. ABC seamlessly integrates with a health system’s EHR, retrieving any relevant cost drivers and including it in the health system’s overall cost data. With this comprehensive, granular level of cost information, financial leaders can pinpoint cost-savings opportunities and cost-effective best practices to implement throughout the organization.
RVUs and RCCs provide an average cost account for every patient encounter. This approach is insufficient because each patient has a different journey through the health system. For example, a patient who enters the health system through the ED will have a different cost compared to a patient who enters through a primary care appointment, even if both patients have the same medical condition. Activity-based costing in healthcare allows systems to access patient resource utilization information for accurate insight into every cost driver of a patient’s unique journey. Clinician variation is real, and ABC is the only way to accurately understand cost and performance.
Activity-based costing in healthcare allows financial leaders to access actionable cost and service line profitability analytics within two to three days of a health system’s financial close, instead of weeks after the closing period. This near-real time information helps financial analysts immediately identify and address cost variation. For example, significant variation for the same procedure might reveal an opportunity to standardize pathways that support best practices or provide additional clinical training, both in pursuit of better care and lower costs.
Organizations can leverage ABC to transform their cost strategy and generate more revenue. Using ABC to understand actual cost, financial leaders can create a proactive pricing strategy and negotiate the best rates for premium services versus commodity services. For example, health systems can command premium pricing for premium services—specific procedures (e.g., specialized surgery) that other health systems can’t perform with the same level of quality—and optimize profitability for that procedure. Additionally, health systems can adjust or discount pricing for commodity services (e.g., imaging) that are more commonplace and have higher competition in the market. ABC allows health systems to accurately price services based on each service’s actual cost.
With continued challenges diminishing healthcare revenue streams, organizations must prioritize an ABC approach to cost accounting. ABC provides five benefits (listed above) that allow health systems to precisely track all cost activity across the care continuum. This level of detailed costing information allows leaders to identify variation in practice, reduce overlapping resources, and find opportunities to improve efficiency—all of which is essential for ongoing financial survival and wellness.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.