Early diagnosis and prompt treatment are crucial for improving recovery chances in pediatric sepsis. Texas Children's Hospital implemented an early alert system and workflow enhancements using big data and prescriptive analytics. The hospital’s investment in new processes, decision support, and analytics has substantially improved pediatric sepsis outcomes.
Pediatric sepsis remains a key concern for hospitals due to the serious nature of the disease. More than 75,000 children are hospitalized with sepsis annually, with between 8 and 21 percent of those diagnosed succumbing to the disease. Early diagnosis and timely care are a top priority, as this significantly improves a patient’s chance of recovery.
Texas Children’s Hospital, a top-ranked, internationally recognized children’s hospital, sought to improve its pediatric sepsis care, but faced some unique challenges in improving the effectiveness of its management of the disease, as sepsis is more difficult to diagnose in children than in adults. To obtain information necessary to drive sepsis improvements, the hospital improved data collection throughout the organization. With the help of big data and prescriptive analytics, it developed an early alert system and workflow changes. Texas Children’s investment in new processes, decision support, and analytics has substantially improved pediatric sepsis outcomes.
More than 75,000 children are hospitalized with sepsis annually.1 Sepsis is extremely dangerous, with a mortality rate of between 8 and 21 percent. Each year, around 7,000 children with sepsis die.2 Early detection improves mortality rates significantly, making the effective management of sepsis—from initial warning signs to treatment—a top priority for hospitals.
Texas Children’s, located in Houston, Texas, is a not-for-profit organization whose mission is to create a healthier future for children and women globally by leading in patient care, education, and research. Texas Children’s is consistently ranked among the top children’s hospitals in the nation. The hospital is continually seeking ways to improve sepsis outcomes for its patients, particularly when it comes to new methods for improving early detection of symptoms.
Since sepsis is more difficult to diagnose in children than in adults, Texas Children’s faced some unique challenges in improving the effectiveness of its management of pediatric sepsis. There are fewer studies focused on children, and less is known about a pragmatic definition for identifying sepsis prospectively and using that definition to drive care improvement.
The organization believed it had 1,034 children evaluated for sepsis, with 856 of those concerning enough to be managed as potential sepsis. Secondary to the challenging nature of analytically identifying the complex diagnosis of sepsis, the true clinical and financial impacts of pediatric sepsis on Texas Children’s were unclear. The hospital lacked applications that could identify cases of potential sepsis, given the lack of precise tests in the science of pediatric sepsis to determine whether sepsis might be present. Initially, most of Texas Children’s data on the subject was collected manually and limited to patients from the emergency department, though data collection was later automated.
The processes for diagnosis and managing patients with sepsis were not adequately standardized, and the organization suspected a significant amount of waste in workflow time and resources in caring for these children. Moreover, the patient experience was not optimized, given the gaps with consistent messaging to parents and provider teams. Texas Children’s knew that early detection of sepsis could save a child’s life, and prioritized pediatric sepsis care for improvement.
Texas Children’s implemented multiple strategies to reduce pediatric sepsis mortality, engaging providers and nursing staff across various specialties, units, and campuses to improve their understanding, recognition, and management of sepsis. This was aided through improved use of data in the EMR and the Health Catalyst® Analytics Platform and a robust suite of analytics applications to drive decision making.
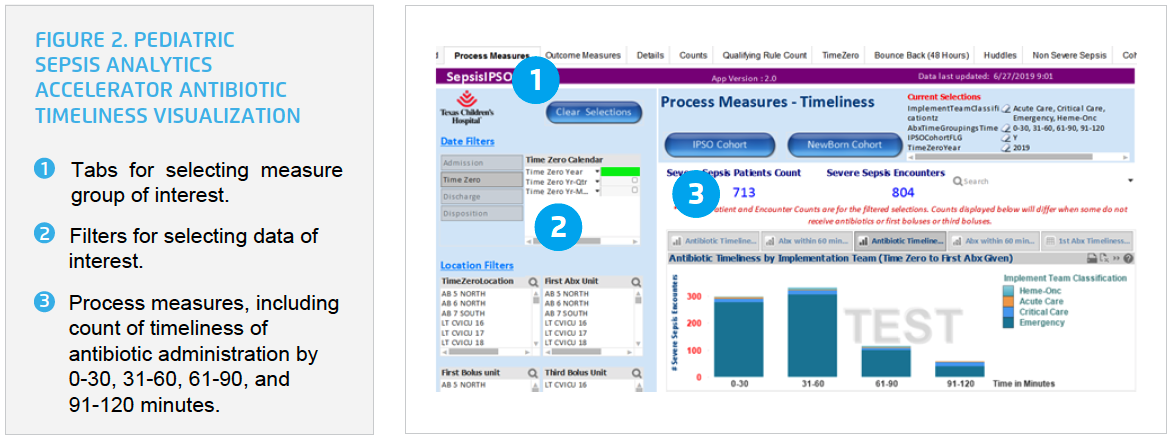
Using the data platform, Texas Children’s developed a Pediatric Sepsis Analytics Accelerator. Texas Children’s uses the analytics accelerator to monitor and improve its sepsis performance. The organization monitors key process measures, such as the timeliness of fluid boluses, antibiotic orders, and antibiotic administration, and uses the analytics accelerator to monitor the effectiveness of its decision support tools. Texas Children’s is able to use the analytics accelerator to actively evaluate the number of children with sepsis, the number of encounters with sepsis, and sepsis mortality, including sepsis mortality in three days from time zero and sepsis mortality in 30 days from time zero (see Figure 1).

Texas Children’s area-based implementation teams leverage real-time and aggregate data on a daily, weekly, monthly, and quarterly basis during the various phases of process improvement. Texas Children’s use of data spans the spectrum of complexity, including the use of simple reports from the EMR, to advanced analytics and unit level population-specific profiles. Texas Children’s has transformed relevant data into actionable data to validate or refute hunches, drive interventions, and to validate if a process change produced the desired results, and ultimately drive improvements. Advanced analytics enabled Texas Children’s to effectively identify potential sepsis, define time zero, and develop prescriptive analytics and decision support.
Texas Children’s data demonstrated what it had suspected—the number of sepsis cases was greater than previously understood —more than 6,000 cases of sepsis (severe sepsis and nonsevere sepsis) annually. Using data from more than 190,000 emergency center encounters, the hospital developed and implemented a pediatric sepsis algorithm to improve the timely diagnosis of sepsis. The algorithm includes data such as heart rate, blood pressure, skin appearance, temperature, and respiratory rate, in addition to other risk factors like diagnosis and/or high-risk medical treatments like chemotherapy, to calculate a risk score and generate a sepsis alert.
Texas Children’s was able to use its data platform to perform a comprehensive analysis of each variable considered for the alert and analyzed the performance of the alert. Doing so required comprehensive evaluation of a sizeable amount of data—while it is one alert, the alert includes multiple parameters, and multiple age groups, resulting in the inclusion of more than 65 different variables. Using analytics, Texas Children’s was able to evaluate each parameter, refining the alert parameters to create the most accurate, predictive alert possible that correctly identifies sepsis, and from there assigns patients with a “sepsis score” that accurately reflects potential risk.
The electronic screening tool automatically calculates the sepsis score each time the child’s chart is opened, or a pertinent new data element is filed. The score is “pushed” to clinicians in the form of an alert, rather than relying on clinicians to manually enter the data to manually calculate a score.
In addition to analytics, Texas Children’s also sought to improve staff knowledge through education. Based on new data, the hospital educated faculty and staff providers to recognize early subtle signs and symptoms of sepsis. The organization enhanced workflows to facilitate escalation of concern about sepsis, using “huddles” and error prevention communication techniques from the safety literature to ensure staff had the latest information on the patient’s current condition. When the sepsis alert fires, the care team huddles to discuss the alert and determine if additional interventions or monitoring are required for the patient.
The huddle includes the charge nurse, the nurse providing care to the patient, patient care assistants, physicians, and the patient’s family—all are engaged in the conversation to ensure the patient is getting the right care at the right time. A structured huddle document, including scripting, helps to ensure new information is documented and accessible at a later date, fostering continued education.
As part of its new workflow process, nursing staff at Texas Children’s is empowered to present the patient to the provider, and the team determines the most appropriate treatment plan together. The organization implemented evidence-based order sets, standardizing approaches to diagnosing, and managing sepsis across 14 disease processes for which children are at risk for sepsis.
Texas Children’s engaged nurses, pharmacists, and physicians in improving the antibiotic workflow, improving the timeliness of antibiotic ordering, delivery, and administration. The organization developed innovative methods to ensure early identification of sepsis, and timely administration of antibiotics, customized to the unique needs of each care setting:
Texas Children’s leveraged the analytics accelerator to evaluate the impact of its interventions on outcomes, supporting rapid cycle improvement, and gaining insight into actionable improvement opportunities.
Texas Children’s can slice and dice its data to answer a multitude of questions. For example, rather than simply evaluating the percent of patients who received antibiotics within 60 minutes, the organization can group and evaluate timeliness by multiple categories. It can view the percent of patients who received antibiotics within 30 minutes, 31-60 minutes, 61-90 minutes, etc. (see Figure 2). The organization can identify specific subgroups, and identify the changes required to improve performance for each subgroup.
Texas Children’s has benefited from improved team structures that oversee the quality improvement and analytics work related to sepsis. Additionally, patients have benefited from improved processes through huddles for agreement on triggering sepsis management, more timely antibiotic delivery, and standardized approaches to managing not only severe sepsis and septic shock, but also potential sepsis. This has resulted in improved outcomes, including a:
"Healthcare professionals at Texas Children’s have benefited from the delivery of improved population data, predictive analytics through interoperable trigger tools, and empowerment to trigger huddles through standardized processes. This has allowed providers to work smarter, not harder. As a result of its ongoing improvement efforts, Texas Children’s was named a sepsis hero by the Sepsis Alliance, recognition of the efforts its teams have invested in driving down sepsis mortality. "We talk about mortality as a statistic, but it’s really about children’s lives. We’ve made a difference in the lives of so many children, that otherwise would have suffered deaths or severe, lasting injury.”
– Charles Macias, MD, MPH, Executive Director, National EMS for Children Innovation and Improvement Center Chief Clinical Systems Integration Officer Texas Children’s Hospital
Texas Children’s is continuing to drive improvement in antibiotic timeliness and formal huddles and plans to expand this improvement work to the NICU and targeted outpatient areas. It plans to evaluate the impact of its pediatric sepsis improvement efforts on financial performance. Additionally, the hospital intends to apply learnings from its sepsis improvement efforts, including the use of data, analytics, and quality improvement methods across the organization, applying this strategy to other patient populations when applicable.