Committed to improving its clinical and financial outcomes, MultiCare focused on improving outcomes for elective colorectal surgery due to high readmission rates and costs. By implementing standardized best practices from the ERAS Society and using data analytics for monitoring, the organization enhanced clinical outcomes and reduced costs for this patient population.
Nationally, readmission within 90 days after colorectal surgery occurs in about one in four patients, at a cost of approximately $9,000 per readmission. Committed to improving its clinical and financial outcomes, MultiCare, an integrated healthcare delivery system in the Pacific Northwest, decided to focus an improvement effort on elective colorectal surgery when it recognized that patient population had a high opportunity for improvement in both clinical outcomes and cost.
Effectively using its existing quality improvement methodology and Collaborative structure, MultiCare leveraged the work of the Enhanced Recovery After Surgery (ERAS) Society and identified and implemented standardized best practice care routines and interventions that would benefit this population. By using the information in the enterprise data warehouse and analytics applications to monitor clinical outcomes and compliance, and leveraging technology in the EHR to provide decision support and order sets at the point of care, MultiCare was able to significantly improve the clinical outcomes for these patients.
Nationally, readmission within 90 days after colorectal surgery occurs for 23.3 percent of patients with a median cost of $9,000 per readmission. On an annual basis, this adds up to roughly $300 million in unwanted readmission costs.1 Surgical site infections (SSIs) are a major contributing factor to readmissions after colorectal surgery. Because SSIs, in general, are a significant issue for hospitals across the United States, the Centers for Medicare and Medicaid Services (CMS) requires hospitals to track SSIs in Hospital Compare on the CMS website for specific procedures—colorectal surgery is one of them.
To effectively reduce readmissions, clinical and systems-based strategies are needed to prevent SSIs and other complications. MultiCare, an integrated healthcare delivery system in the Pacific Northwest, had in place a robust improvement methodology based on a structure of Clinical Collaboratives—teams focused on improving patient outcomes, cost, and patient experience. Within this structure, the Surgery Collaborative was charged with implementing clinical and systems-based prevention strategies to reduce readmissions, length of stay, and SSIs for patients undergoing surgery. The Surgery Collaborative decided to focus on colorectal surgery as its first improvement effort within this Collaborative structure because it was a patient population that presented a valuable opportunity for improvement of clinical outcomes and cost.
Since this was the first clinical improvement project for the Surgical Collaborative under the Collaborative structure, the team was not experienced in this improvement methodology and had not yet established proven implementation strategies. They had data that revealed clinical variation in colorectal surgery, but the Surgery Collaborative did not have agreement among involved surgeons on what constituted the best practices that should be followed to improve outcomes for this patient population.
Colorectal surgery affects a complex group of patients in multiple locations of care, and as such, any proposed practice changes would likely have an impact on multiple discipline’s processes and care routines. Pharmacists and surgeons both expressed concern with moving to standardized practices for this complex population, which suggested that the Surgery Collaborative might encounter resistance in gaining adoption of standard order sets and care routines unless they could adequately address that complexity.
Any change in practice or workflow was unlikely to be successful unless the team had organizational support, including obtaining the resources needed to develop order sets, provide education, and make changes in the EHR. Without the organization’s support, getting multidisciplinary participation and input into the process would not be possible. The team also had no way to easily track the performance of interventions as they related to patient outcomes at the organizational and provider levels. Without this information, they would not be able to show the impact of any potential improvement efforts.
Having analyzed the situation and identified potential challenges, the Surgery Collaborative was ready to move to the next step.
Narrowing the target population. Colon surgeries are often performed emergently, and many patients who have colon surgery do not do so by choice. Surgery is often necessary due to a tumor, trauma, or a blockage. Patients undergoing emergent colon surgery often have comorbidities and complications such as an active infection. However, in other cases, colon surgery is pre-scheduled as an elective surgery.
The Surgery Collaborative decided to focus a workgroup on elective colon surgery only, and avoid the emergent trauma cases so that it had a more predictable and controllable population. Even with that narrowing of the population, the team was still dealing with patients that are more complex and more fragile than many other diagnoses or patient populations.
Forming the team. After selecting elective colorectal surgery as their area of focus, the Surgery Collaborative obtained administrative buy-in and support to launch an elective colorectal surgery improvement workgroup. The administrative buy-in ensured the team would have the resources required to build order sets and provide education as the initiative progressed. To aid in getting buy-in and engagement from all of the disciplines whose care routines would be impacted, the workgroup’s members included multiple disciplines, including:
Since this was the first formal improvement effort of the Surgery Collaborative, the team needed considerable time to work out their processes, develop trust within the team, and work to find ways to implement changes effectively. Initially, the elective colorectal surgery workgroup decided to focus on:
To accomplish these tasks in a way that was cost effective, the team met weekly during the development phase, monthly during the deployment phase, and quarterly during the maintenance phase.
Identifying best practices through research and analytics. Research into best practices for surgery led the workgroup repeatedly to the ERAS Society, an international non-profit professional organization dedicated to the development of protocols based on a multimodal, multidisciplinary approach to the care of surgical patients.2 Guided by the recommendations from the internationally recognized ERAS protocol, the elective colorectal surgery workgroup had a strong, well-documented set of best practices to start from while developing their planned interventions.
With the addition of data and information about MultiCare’s practices and patients, made possible through the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications, the conversation moved quickly from the theoretical to the practical. Having a strong foundation of trusted information, the workgroup was able to quickly build consensus and identify the interventions, and practice changes they believed would be most impactful.
The ability to reduce clinical variation is dependent on establishing consistent care routines based on best practice that can be shown to produce better patient outcomes.
Interventions begin in the outpatient setting. To improve elective colorectal surgery outcomes, there are several key activities that need to occur in the outpatient setting before surgery takes place. Providers must engage patients with pre-op education, pre-op testing, and answer any questions patients may have about what occurs during and after surgery. Additionally, providers or their staff should instruct patients on special cleaning routines that need to be done the night before surgery.
As part of the preparation for surgery, patients are instructed on the importance of diet and nutritional supplements. Nutrition is a key factor for recovery for colorectal surgery patients. At most, the lead time between identifying a need to have colorectal surgery and the actual procedure is four weeks. For best results, there is a need to optimize the patient’s nutritional status as quickly as possible.
Specific outcomes targeted in the inpatient setting. In the hospital, the specific clinical outcomes the workgroup targeted to improve were: pain, LOS, readmissions, and infections.
Pain reduction was selected as an area of focus and a key driver of improvement due to its close relationship with recovery time and patient satisfaction. The team developed a pain protocol using the ERAS recommendations with one modification: MultiCare modified the ERAS protocol slightly by using oral Tylenol instead of intravenous (IV) Tylenol post op, finding that avoiding IV pain medication, and the use of patient controlled analgesia (PCA) pumps, led to faster recovery, which in turn led to earlier discharge and an overall improvement in the patient experience.
Other interventions were particularly effective in shortening LOS, reducing complications, and improving clinical outcomes. These measures included early ambulation post-op, pre-op and post-op glycemic control, bowel prep prior to surgery, and limited use and quick discontinuation of tubes, especially urinary catheters. Indwelling urinary catheters were encouraged to be used only for left-sided colon surgeries, and to be discontinued after 24 hours. Staying true to the recommendations in the ERAS protocol, particular attention was paid to nutritional enhancement, including pre-op use of nutritional shakes and shorter periods of time without food and fluids prior to surgery, as well as an earlier initiation of a post-op diet that was low in fat, fiber, and fluids.
Reducing the risk of infection across the care continuum. The workgroup also selected reduction of SSIs as an area of focus for improvement because of the negative consequences infection has on patient outcomes, increasing LOS and likelihood of readmission, and bringing an associated increase in cost and decrease in patient satisfaction.
The workgroup’s changes were remarkably effective in reducing SSIs related to elective colorectal surgery. The team operated on the premise that infection is not caused by just one thing; therefore, it cannot be prevented by just one thing—a group of interventions was necessary. The workgroup identified a bundle of interventions for reducing infection, including:
These and other interventions were focused around the time of the actual surgery. However, an infection can happen after surgery as well. For this reason, the workgroup also focused on developing post-op interventions to help prevent infection from occurring in the hospital prior to discharge, at a skilled nursing facility (SNF), or while the patient is at home.
Ensuring continuation of optimal care across the care continuum. Approximately 20 percent of all surgical patients go to a SNF after post-surgery discharge. MultiCare decided to employ wound care specialists to work with staff at the SNFs to ensure patients received proper wound care, and that any problems or signs of infection were quickly recognized and addressed.
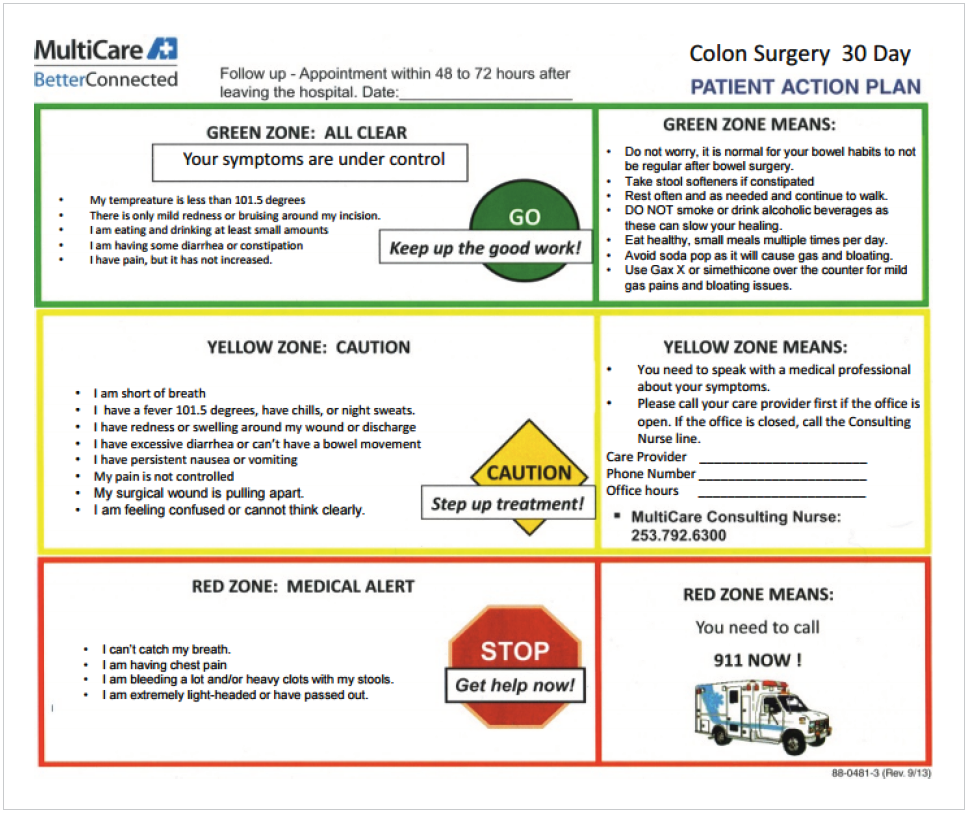
For those patients who were discharged to their homes, discharge instructions with red, yellow, and green zones were developed specifically for colorectal surgery to help patients and their families take appropriate action or reach out for assistance during care at home (see Figure 1). These patient-centered interventions have improved the patient experience and have reduced the number of infections and overall readmissions.
Using guidelines and checklists. The comprehensive description of the care process MultiCare adopted for patients undergoing elective colon surgery was built into the Elective Colon Surgery Care Guideline (see Figure 2), a written document used to outline the recommendations and rationale for caring for patients having elective colorectal surgery. All approved care guidelines, including this one, are publicly available on the MultiCare Connected Care website. These guidelines are updated by the responsible workgroup every two years.
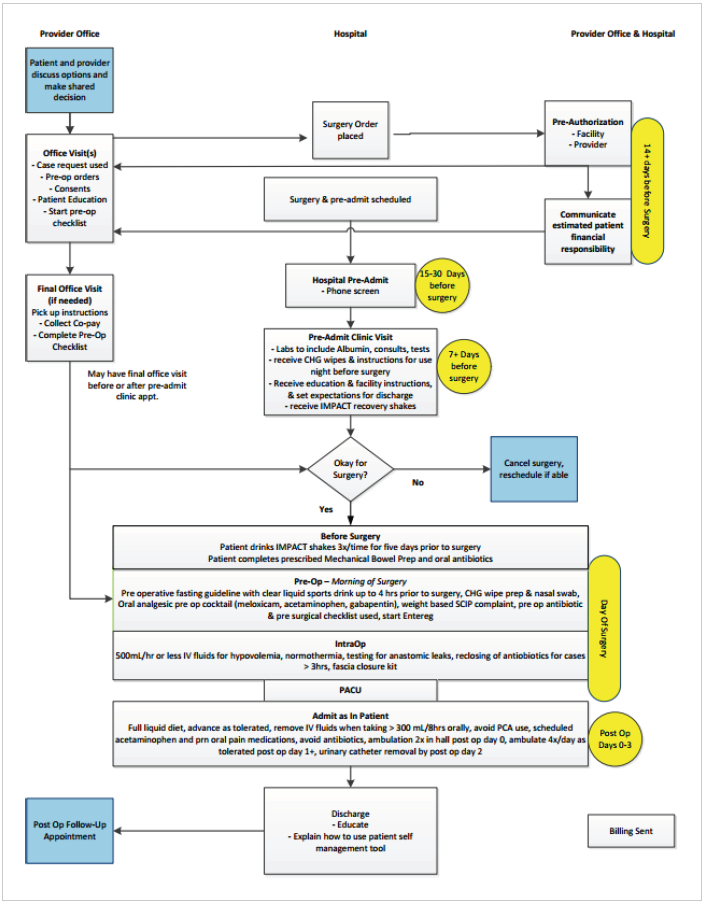
To further facilitate the adoption of best practices across MultiCare, the practice changes and care routines that the Surgery Collaborative workgroup implemented were also built into an elective colon surgery care map and surgical checklist, all supported by standard order sets. These support materials reinforced patient education and provided a standard, accessible, and easy-to-understand instruction set for all disciplines on how to care for elective colon surgery patients.
During development, each of these materials went through multiple revisions within the workgroup. The content was checked by each discipline in the workgroup to ensure accuracy before deployment. To avoid later rejection and revisions, the workgroup made a concerted effort to ensure they had the support and cooperation of all invested parties before the documents were approved and finalized.
Leveraging analytics to monitor compliance and measure impact. The interventions that required orders were built into a standard order set. This made it easy to communicate to the provider the recommended actions to be taken, and easy for all caregivers to carry out the interventions. Doing so also established a record of the interventions in the EHR in discrete data fields, so information could be tracked, measured, trended, and analyzed using analytics applications.
The analytics applications provide reports and detailed information to providers. The platform also allows clinicians to drill down to identify patient groups that can benefit from a surgical intervention, identify patterns and impact of interventions on outcomes, and monitor cost variation among procedures. Clinicians use the information to follow complication rates, outcomes, and monitor order set compliance. Members of the workgroup believe that without the information provided by these applications they would have been unable to affect change so rapidly, or effectively maintain the changes and sustain their outcomes.
The data has shown that interventions within the order sets are being used consistently, and are positively impacting patient outcomes. Armed with data and information on the impact of interventions on outcomes, the workgroup supported the implementation and adoption of the order sets with peer-to-peer conversations and outreach to practitioners. To further encourage adoption of the order sets, MultiCare selected order set utilization as one of its quality metrics for CMS. This alignment of incentives provided extra motivation for practitioners to use the order sets.
Due to the adoption of comprehensive best practices across the care continuum, MultiCare’s elective colorectal surgery workgroup delivered impressive results on all their focused outcome measures:
Order set adoption across MultiCare has contributed to these impressive results. Ninety-six percent of patients receive at least one of the colon surgery order sets; 89 percent of patients receive both order sets.
In conjunction with other interventions, adopting a “Strong for Surgery” approach aimed at improving patient nutrition and engaging them to work toward optimizing their own outcomes has led to improved post-surgery health. Most patients are discharged two days after elective colorectal surgery, and many are driving their own car again in as little as five days. This has greatly boosted patient confidence in the procedure and has contributed to a rise in patient satisfaction.
“These are difficult surgeries to understand and go through – or to have a loved one go through. So, having a standardized pathway we can point patients and their families toward takes away a lot of that anxiety and uncertainty, which in turn contributes positively to patient satisfaction and health.”
– Dr. Joshua Levin, MD, FACS, FASCRS, MultiCare Colon and Rectal Surgery
To date, improvements have mostly focused on pre-op and post-op interventions. MultiCare continues to look for ways to further improve LOS, readmissions, and patient experience. The next area of focus will be on cost improvement in the OR. The Surgery Collaborative is working on a protocol that will result in improvements in equipment availability and the speed and accuracy of pre-operation preparations. These improvements will also lead to workflow changes that should make more effective use of OR staff by minimizing unnecessary trips to gather equipment for a procedure.
The Surgery Collaborative is building on the experience of other MultiCare Collaboratives and putting processes in place to provide metric review and allow for prompt response to any deterioration of outcomes, all in an effort to ensure that improvements are sustained.