Data-Driven Clinical Documentation Improvement Program Increases Revenue and Improves Accuracy of Risk Adjusted Quality Metrics

- 12.1 percent improvement in CV surgical cardiology CC/MCC capture rate.
- 6.3 percent increase in medical cardiology CC/MCC capture rate.
- Increased accuracy in publically reported risk adjusted quality metrics
- Revenue capture improvement across the system – resulting in millions of dollars of additional reimbursements.
Allina Health, an integrated delivery system throughout Minnesota and western Wisconsin, has long understood the value of clinical documentation improvement (CDI), and its growing importance in recent years. With the implementation of ICD-10, the specificity needed for accurate coding has increased, and reimbursement shifts have occurred as well, creating sizeable payment disparity for some clinical conditions. Leaders at Allina wanted to understand where their CDI program would have the greatest return on investment. However, data from the EHR was not sufficient to inform their strategy. CDI specialists still lacked the ability to perform a comprehensive assessment of the accuracy of clinical documentation, and were unable to confidently target improvement efforts in areas that would generate the greatest return on investment. To take a more data-driven approach, team members leveraged the Health Catalyst Analytics Platform, including their Late-Binding™ Data Warehouse and broad suite of analytics applications to develop a CDI analytics application. With the application, the team identified opportunities and thoroughly vetted them, before collaborating with physicians and service line leaders to educate providers on documentation improvements.
WHY IMPROVING CLINICAL DOCUMENTATION MATTERS MORE THAN EVER
Accurate clinical documentation has always been important in healthcare, but it’s become even more critical as providers face increasing regulatory, financial, and operational pressures to improve their documentation. For clinical documentation to be meaningful, it must be accurate, timely, appropriately reflect the scope of services provided to the patient, and provide an appropriate clinical picture of the patient.1 Understanding the patient’s overall state is essential since many of the quality and safety measures that impact hospital payments are risk stratified.2 Therefore, if an organization is not accurately capturing complications or comorbidities (CC) and major complications or comorbidities (MCC) of patients, the mortality index (the ratio of actual deaths to expected deaths) used in publicly reported data and for comparison to other hospitals will not be correct. When the CC/MCC capture rate is lower than what it should be, it doesn’t properly indicate patient conditions and skews the mortality rate, making it appear higher than what it actually is.
Incorrect CC/MCC capture rates are also problematic because clinical documentation, and the resulting coding used to bill for services, directly impacts reimbursement, and that impact can be quite significant. Further, the specificity needed for accurate coding has increased with the implementation of ICD-10. That change, coupled with reimbursement shifts, has created substantial payment disparities for some clinical conditions. Consider the following as an example: for a patient with heart failure and shock without CC/MCC, a hospital receives a payment of $3,971.20. If that same patient has a CC, the payment increases to $5,769.46. For heart failure and shock with MCC, the payment increases to $8,866.20. The numbers tell the story. Failure to improve clinical documentation puts providers at risk for losing the revenue that is appropriate for the level of care they have delivered.
Leaders at Allina Health, which has more than 109,000 inpatient admissions annually, and more than 1.45 million hospital outpatient admissions, understood the need to take action at their 13 hospitals and 61 clinics. While they had already been working to enhance the quality of their clinical documentation, they now wanted to take a more focused, data-driven approach, and direct their efforts where they could produce the most meaningful results.
LACK OF DATA IS DETRIMENTAL TO CDI EFFORTS
CDI specialists at Allina concentrated on improving the quality and accuracy of documentation, to ensure that it conveyed an accurate picture of the patient and contained the information that the care team needed. While that work was valuable, it wasn’t informed by data. The team members lacked the ability to perform a comprehensive assessment of the accuracy of clinical documentation, including CC/MCC. They needed data-driven insights to target their CDI efforts in areas with the greatest opportunity for improvement.
Transforming the Clinical Documentation Improvement Program
Leaders at Allina noticeably improved the consistency of their clinical documentation with the implementation of an EHR. For the first time, CDI specialists could partner with an analytics team to understand the impact of documentation on coding and reimbursement. While the data from the EHR was a step forward and helped improved the consistency of documentation, it was ultimately not sufficient to drive improvement. Leaders at Allina decided to utilize the Health Catalyst Analytics Platform to develop a CDI analytics application to maximize the effectiveness of their CDI program.
They had a four-pronged strategy for optimizing the new technology:
- Conducting a thorough analysis to identify key targets.
- Partnering with physician leaders and service line directors.
- Educating providers through one-on-one engagement.
- Leveraging decision support tools to enhance the program’s success.
Conducting a Thorough Analysis to Identify Key Targets
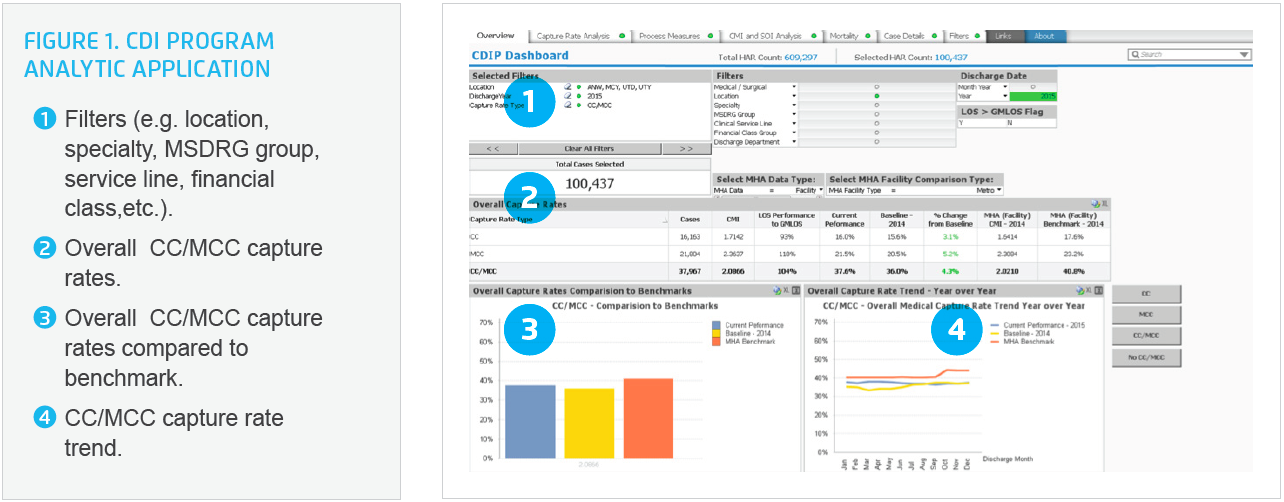
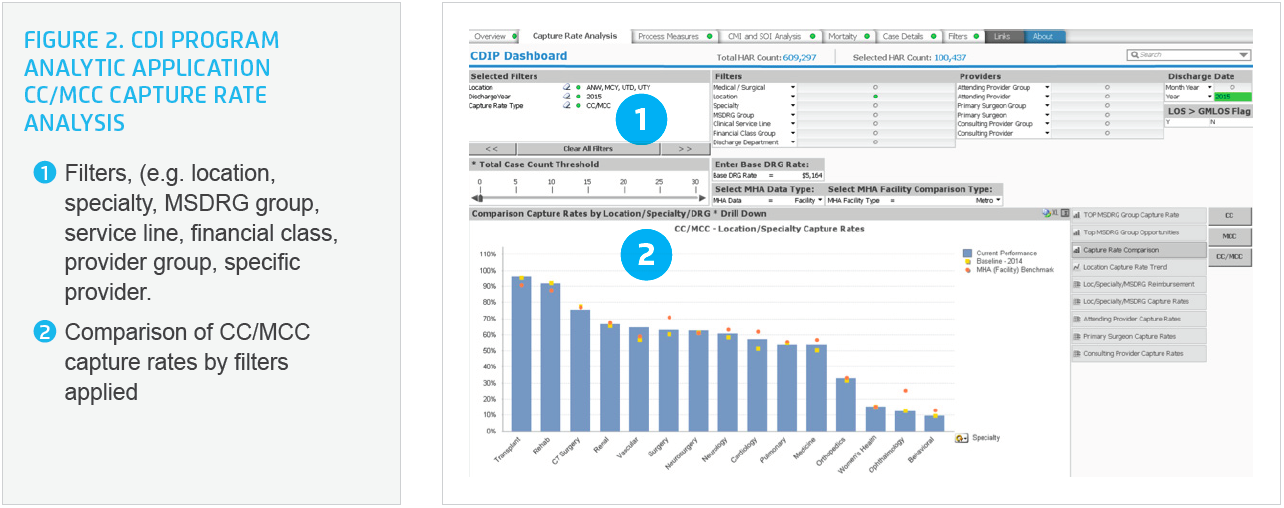
The CDI analytics application enables easy visualization of CC/MCC capture rates compared against benchmark data from the Minnesota Hospital Association (MHA), including a case mix index and severity of illness analysis, mortality rate, and case details (see Figure 1). Rather than focusing only on Medicare accounts, which is common for clinical documentation improvement efforts, the Allina CDI program employs data and analytics to identify specific specialties or providers that have the greatest potential for improving the specificity of their documentation, contributing to a more accurate CC/MCC capture rate (see Figure 2). Team members at Allina can quickly visualize the CC/MCC capture rate between their facilities, CC/MCC capture rate by location and specialty, CC/MCC capture rate by provider and provider groups, and CC/MCC capture rate in comparison to MHA benchmark data.
After identifying potential opportunities in the CDI analytics application, the specialists begin a detailed review of the data to determine if the clinical documentation could be improved, or if it already contains the appropriate specificity and accuracy. Their intention is to be purposeful, and complete their due diligence, prior to engaging with physicians, advanced registered nurse practitioners, or physician assistants. At times, the CC/MCC capture rate may be lower than benchmark, but the detailed review of documentation reveals that it presents an accurate, comprehensive clinical picture of the patient. Other times, the detailed review reveals that the documentation can be improved. Once the analysis is complete, the CDI specialists can confirm whether there is actual opportunity for improvement and start taking action.
Partnering with Physician Leaders and Service Line Directors
The team partners with the medical director for the CDI program and service line leaders, working together to approach the relevant providers. Physician leaders, who have a deep understanding of the data, help to determine how CDI specialists should best share performance data with providers. The medical director for the CDI program and physician leaders collaborate with their colleagues to explain how their clinical documentation might be improved, and illustrate why the specificity and accuracy of clinical documentation is so critical. The CDI specialists also partner with service line leaders who schedule meetings with providers, and provide leadership by setting clear expectations about the importance of the review process and accurate clinical documentation.
Educating Providers Through One-on-One Engagement
Allina’s CDI specialists use targeted one-on-one education sessions, and concurrent chart reviews, to engage with providers on improving the accuracy of clinical documentation and CC/MCC capture rate. In the past, they had relied on online learning applications to review documentation principles with providers. However, they found that individualized coaching and customized support is more effective because sharing specific examples from the provider’s own documentation is more impactful than generic education curricula. CDI specialists hold personalized education sessions with providers, and explain that they will monitor their documentation by performing concurrent chart reviews. The CDI specialists complete the concurrent chart reviews on a daily basis when providers are on shift. Throughout the process, the CDI specialists use the analytics application to identify if the providers’ CC/MCC capture rates have improved. They review provider-specific data again two months and four months after the initial education sessions occur.
Leveraging Decision Support Tools to Enhance the Program’s Success
Team members at Allina decided to integrate decision support tools into the EHR to drive even more improvements to the specificity and accuracy of their clinical documentation. They embedded smart tools and phrases in hospitalists’ notes. Hospitalists use the smart tools and phrases to increase the accuracy of their clinical documentation. Additionally, if providers document an unspecified diagnosis on the problem list, they receive an automated prompt that requests more specificity, eliminating the need for additional follow up later and increasing accuracy.
RESULTS
CDI specialists at Allina used analytics, education, coaching, and decision support tools to help improve the accuracy of clinical documentation and CC/MCC capture rates, which has resulted in appropriate reimbursement for the services provided. Thus far, over a 12-month period they have realized:
- 12.1 percent improvement in surgical cardiology CC/MCC capture rate.
- 6.3 percent increase in medical cardiology CC/MCC capture rate.
- Increased accuracy in publically reported risk adjusted quality metrics
- Revenue capture improvement across the system – resulting in millions of dollars of additional reimbursements
“It’s important for CDI programs to set realistic goals and expectations. Initially, we were focused on meeting benchmark performance, but that shifted once we were able to visualize and better understand our data. Within surgical specialties, many CC/MCC are for surgical complications and that’s not what we want to deliver. Our current goal is to perform under benchmark for surgical specialties because safe care is what our patients deserve.”
– Erin Holthusen, RN, CCDS, CDI Manager
WHAT’S NEXT
Clinical documentation improvement will grow in importance as the healthcare landscape continues to shift. Team members at Allina want to build on their program’s success and further leverage the CDI analytics application. They plan to add data on LOS and geometric mean length of stay (GMLOS) to the application, which will enable them to visualize LOS outliers, determine if there is an opportunity to improve CC/MCC capture rate, and ensure that the clinical documentation reflects the clinical challenges contributing to a prolonged LOS.
REFERENCES
- Neville, D. & Bonno, D. (2012). The why and how of a CDI program. Quadra Med.
- McNally, M. (2015). The importance of detailed documentation in ICD-10. Bulletin of the American College of Surgeons.
ABOUT HEALTH CATALYST
Health Catalyst is a mission-driven data warehousing and analytics company that helps healthcare organizations of all sizes perform the clinical, financial, and operational reporting and analysis needed for population health and accountable care. Our proven enterprise data warehouse (EDW) and analytics platform helps improve quality, add efficiency and lower costs in support of more than 50 million patients for organizations ranging from the largest US health system to forward-thinking physician practices.
For more information, visit healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.