Six Steps Towards Meaningful, Ongoing Healthcare Performance Improvement
Health systems primarily concentrate performance improvement initiatives around critical areas, including clinical outcomes, patient experiences, and organizational costs. While this high-value improvement approach has the potential for significant impact, its long-term success relies on strategic execution.
Performance improvement efforts fall short of their desired results when organizations approach improvement as a series of one-off projects. To achieve an effective and sustainable performance improvement, organizations must develop and perform their initiatives within an ongoing performance infrastructure and program.
An Infrastructure for Ongoing Performance Improvement Initiatives
The ongoing performance improvement infrastructure comprises the following three systems-based elements:
- An analytics system to measure improvement. A performance improvement analytics system (e.g., the Health Catalyst Data Operating System (DOS™)) integrates the organization’s data sources (e.g., clinical, claims, financial, operational, etc.) and facilitates quick, accessible data sharing.
- An adoption system to create permanent cross-functional workgroup teams focused on identifying, deploying, and monitoring the effectiveness of quality improvements. Interdisciplinary teams analyze the data and discover patterns that lead to insights and progress through different levels of healthcare analytics, per the Healthcare Analytics Adoption Model (Figure 1).
- A best practice system to deploy a data-driven approach to implementing evidence-based best practices.
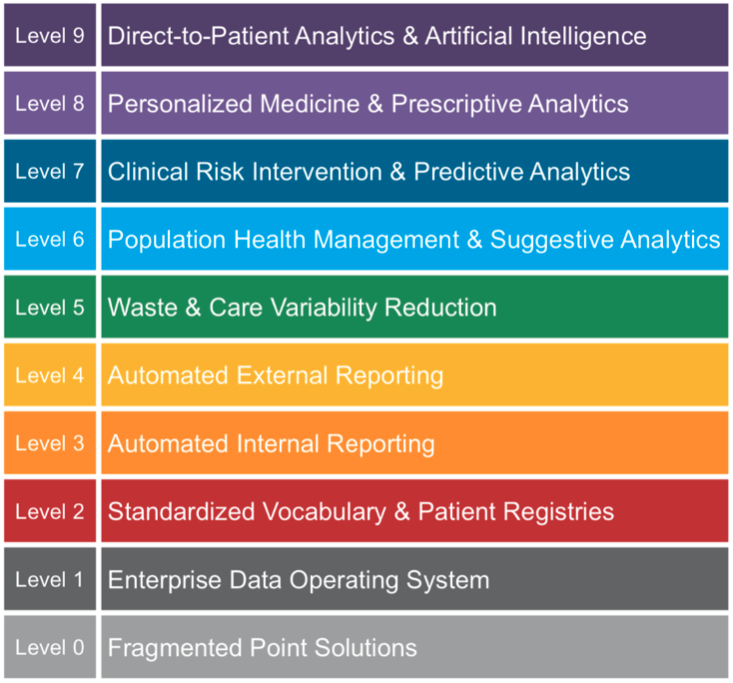
Figure 1: The Healthcare Analytics Adoption Model.
Six Steps to Implementing a Sustainable and Impactful Performance Improvement Program
With the improvement infrastructure in place, healthcare organizations can follow six steps for a sustainable, impactful performance improvement program:
Step 1: Integrate Performance Improvement into Strategic Objectives
Healthcare is a complex, adaptive system comprised of interactions and relationships between different components. Health systems must integrate performance improvement within the organization’s strategic objectives (e.g., forming an ACO or focusing on population health management). Integrating performance improvement also improves efficiency and focuses resources on programs most likely to yield meaningful overall benefit.
Step 2: Use Analytics to Unlock Data and Identify Areas of Opportunity
An analytics application can help an organization identify opportunities for improvement efforts by uncovering variation. Variation points to a potential for standardizing processes because the existence of variation inherently means that some care practices are more efficient and produce higher-quality outcomes than others. There also is a greater likelihood that some practices are not achieving optimum outcomes. Hospitals and health systems will have a significant opportunity for care improvement if they can identify their highest-performing practices and begin to make those practices and evidence-based practices the standards for all caregivers.
Variation in cost can be a good surrogate for quality of care because the higher cost may result from the delivery of inefficient or unnecessary services. As the prescribers of care, clinicians are among the most significant influencers in managing variable cost, representing the direct cost. By focusing on variable cost (i.e., looking at the volume of procedures and cost per procedure, in particular), they can identify avoidable costs and begin working with clinicians, using evidence-based practices, to address them.
Step 3: Prioritize Programs Using a Combination of Analytics and an Adoption System
Successfully improving clinical outcomes and streamlining operations requires a strong organizational commitment and changes in culture, organizational structure, staff education, and workflow processes. Consequently, any organization that embarks on a performance improvement journey should first assess its readiness for change. Examples of criteria that an organizational readiness assessment evaluates include clinical leadership readiness, data availability, shared vision, and administrative support (e.g., data manager, outcomes analyst availability).
A readiness assessment helps the organization determine how ready the teams are to accept change, to estimate what, if any, impact there is on staffing and the potential implications for frontline caregivers. Understanding the strategic objectives and integrating results from a readiness assessment and analytics help the organization prioritize which care families (clinical services) can be starting points.
Step 4: Define the Performance Improvement Program’s Permanent Teams
The organization will require permanent performance improvement teams to review and analyze data, define evidence-based and best practices, and monitor ongoing results. Improvement teams should include the following components:
- A guidance team should have accountability for clinical quality across the continuum of care in a specific domain (such as women and children). The primary role of such a team is to select goals, prioritize work, allocate resources, and remove barriers. The guidance team then delegates accountability to clinical improvement teams to improve care.
- Clinical improvement teams typically report to a physician and nurse and consist of frontline staff who understand the processes targeted for improvement. These teams define workgroup outputs and lead process improvement implementation. Whenever possible, clinical improvement teams should represent a broad range of departments, clinics, hospitals, and regions to help disseminate knowledge across the organization. These teams generally create workgroups to perform detailed work.
- Workgroups generally report to a physician and nurse subject matter expert and include best practices, analytics, and technical experts. These teams frequently meet to analyze processes and data and look for trends and improvements. Their role is to develop aim statements, identify interventions, draft knowledge assets (e.g., order sets, patient safety protocols, etc.), define the analytic system, and provide ongoing feedback of the status of the care process improvement initiatives.
Step 5: Use a Best-Practice System to Define Program Outcomes and Interventions
The focus of performance improvement initiatives for many organizations tends to be on low-performance outliers—that is, identifying instances where costs are much higher and outcomes substantially poorer than averages among caregivers. However, a more effective approach is to identify those practices that consistently lead to the best outcomes and promote them, with evidence-based guidelines, to improve outcomes across the board—in other words, best practices.
Step 6: Estimate the ROI
As the guidance team sets priorities for performance improvement, the team may also estimate the potential ROI for each initiative based on available information. The team can start by identifying organizational costs and assessing benefits using industry benchmarks for similar projects, vendor case studies, and internal estimates. Most organizations will need to educate their clinicians, operations, and finance departments on the value of sharing data and working together on interdisciplinary teams rather than keeping everything in silos.
Next, the team should identify direct benefits and savings (either from enhanced efficiency and productivity) or from clinical improvement and waste reduction. Then, the team can identify indirect benefits, such as a reduction in future infections or an improvement in patient satisfaction.
The team also should consider revenue opportunities, such as higher market share and patient volume, an increase in contract compliance, or a reduction of bad debt.
Building the Framework for Healthcare Performance Improvement Initiatives
Creating a foundation for sustainable improvement and prioritizing initiatives does not have to be overwhelming. By following these steps and establishing a framework for performance improvement based on analytics, the right teams, and evidence-based practices, an organization can obtain the right tools to achieve and sustain performance improvement gains into the future.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.

