As a performance-based incentive program, DSRIP (the Delivery System Reform Incentive Payment) is designed to help participating states reform Medicaid. To date, 13 states have implemented DSRIP and received a Section 1115 waiver from CMS to transform their Medicaid programs and align them with value-based reimbursement. These states have agreed to budget neutrality, transparency, statewide quality metrics, and frequent reporting of outcomes.
While each state’s program structure and objectives are unique, under DSRIP, participating states share three key goals:
1. Reducing the total medical spend.
2. Improving patient outcomes.
3. Establishing a direct link between provider performance and payment.
 Download
Download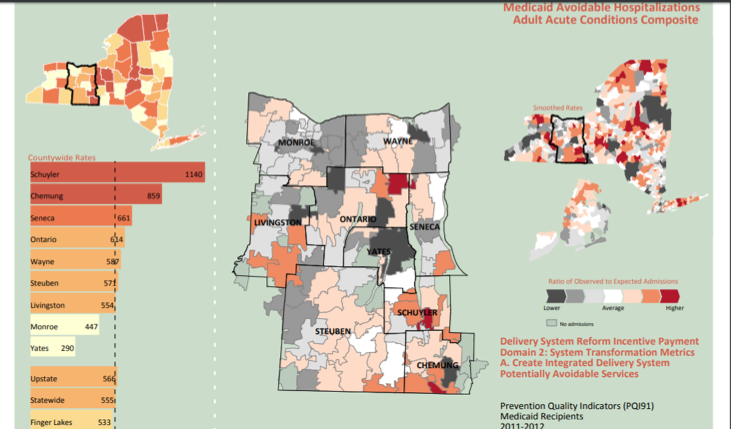
As part of the evolving Medicaid programs, Delivery System Reform Incentive Payment (DSRIP) programs have been implemented in thirteen states with the goal of transforming Medicaid in those states. DSRIP programs are not grants but, rather, performance-based incentive programs. They emphasize three concurrent goals for each state:
In 2010 California was the first state to implement the DSRIP program. Since then, more states—Alabama, Arizona, Kansas, Massachusetts, New Hampshire, New Jersey, New Mexico, New York, Oregon, Rhode Island, Texas, and Washington—have implemented DSRIP. Each of these states obtained a Section 1115 waiver from the Centers for Medicare and Medicaid Services (CMS). The Section 115 waiver, which is typically in effect for five years, gives states the authority to transform their Medicaid programs and align them with value-based reimbursement. Participating states must agree to budget neutrality, transparency, statewide quality metrics, and frequent reporting of outcomes. Each state’s program is unique in its structure and goal.
In general, the DSRIP programs focus on four main areas:
Below are the DSRIP states and a few notes on structure:
The DSRIP programs that started before 2014 focused on payment enhancement and preservation for safety net providers. The newer (post 2014) DSRIP programs show a greater emphasis on Medicaid payment and delivery system reforms, as well as increased emphasis on mental health programs.
The DSRIP policymakers recognized upfront the need to start with process and move to population improvements over time. This allows for short-term and long-term goals; many program goals were milestones in the journey.
The three state programs below differ in content but share a focus on improving health for the state’s population:
To support the above areas, providers will need to collect data and report results. All participating states must report standardized measures. Health systems provide general reports to the state semi-annually.
For example, the state of New York requires six types of reports:
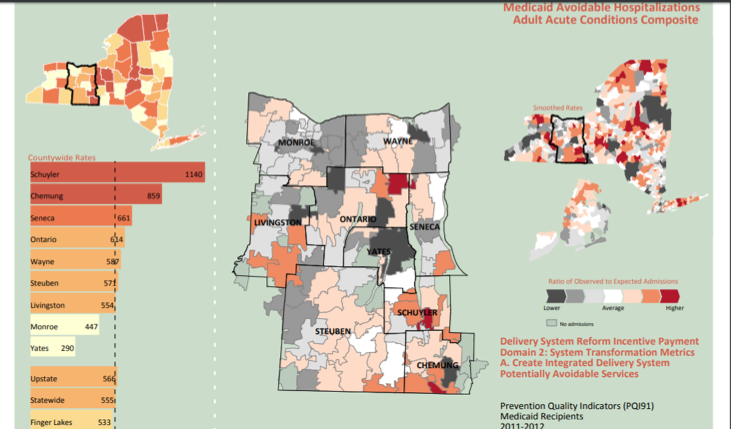
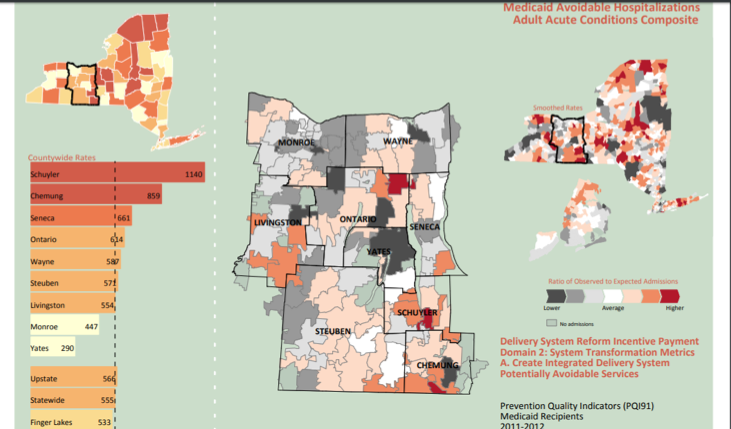
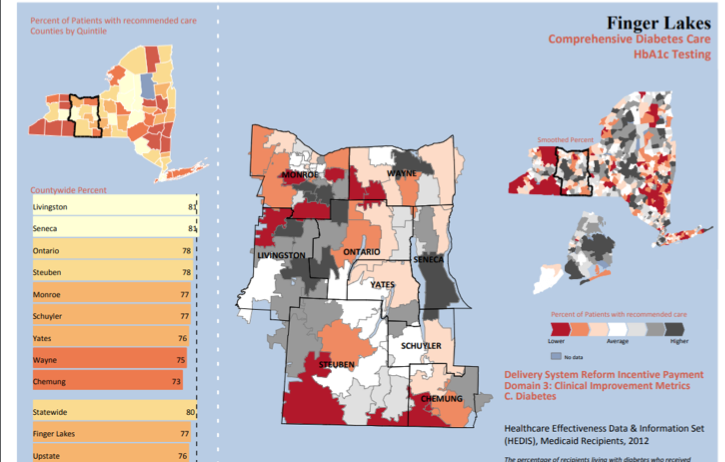
The following results from 2011 and 2012 (Figures 1 and 2), publicly available on the New York State Department of Health website, show metrics for hospitalizations and diabetes care:
According to a March 2018 Medicaid and CHIP Payment and Access Commission (MACPAC) issue brief, key policy changes for the more recent waivers increase the emphasis on reform:
States and health systems have had some concerns with DSRIP, as they need to align DSRIP with other Medicaid and value-based programs. Metrics and implementation plans cannot conflict with other initiatives. DSRIP participants, however, are meeting the program’s challenges. Programs in New York state, for example, are meeting high standards:
The New York DSRIP program started with the bold goal “to reduce avoidable hospital use by 25 percent through transforming the New York healthcare system into a financially viable, high performing system.” The New York program began in April 2014 and will continue through March 2020. The state required providers and community-based organizations to form Performing Provider Systems (PPS); New York currently has 25 PPSs. By the end of the waiver period, 80 percent of payments to providers must use value-based methodologies.
A 2016 article from the Healthcare Finance Management Association describes the experiences of Finger Lakes Performing Provider System (FLPPS), a nonprofit with more than 3,000 providers from 600 organizations. FLPPS members united to provide care to 400,000 Medicaid and uninsured individuals, with several key goals:
DSRIP payments to providers are tied to achieving process metrics; in 2015 around 150 organizations received $23 million in incentive payments. To date FLPPS has achieved 100 percent of the possible award dollars. The organization is working on the next phase of delivery reform to mature the performance goals for each member of the delivery system.
Providers have met the milestones and targets but have struggled to isolate the impact of the DSRIP projects against other policy changes. Three states (California, Texas, and Massachusetts) have completed final evaluations for the first time period. To date little evidence exists that DSRIP waivers have significantly improved quality and health outcomes or reduced spending on healthcare services. Several states have shown lower ED visits but are unable to tie this outcome directly to DSRIP.
Despite lack of evidence, DSRIP also has had obvious some overall positive results:
DSRIP could be an important program in the pursuit of delivery system reform. Many models may need continued monitoring and measurement. But which models will be successful, and which ones can be replicated to improve our health care system? CMS has initiated this waiver process but has not issued any specific guidance about future requirements. Recent waiver approvals, however, include more accountability and broader list of provider participants. As renewal dates approach, measurement of population and provider results will be important. Comparing the effort to maintain and participate in the program with final outcomes will help participants replicate and scale the population-based movement at the state level.
Participating DSRIP states are best positioned to meet DSRIP requirements when they have seven elements in place:
States that participate in DSRIP and meets its goals gain momentum toward value-base care, as well as rewards for high clinical performance. Without such incentives, states risk remaining in an older fee-for-service system and won’t be prepared as healthcare continually shifts towards a value-based system. By putting in place the seven must-haves for DSRIP above, states are positioned the transform their Medicaid programs and thrive in a value-based environment.
Would you like to learn more about this topic? Here are some articles we suggest: