Publicly reported measures of healthcare quality include the Hospital Safety Score Grades, which award a letter grade representing performance for 30 evidence-based patient safety measures. In the fall of 2014, Piedmont's Hospital Safety Score Grades included four "C's" and a "D," highlighting the need for improved quality measures. To enhance efficiency and outcomes, Piedmont utilized its analytics platform to automate surveillance activities and better monitor quality improvement efforts, ultimately redesigning its approach to ensure resources were aligned with the value chain for sustained improvements.
Publicly reported measures of healthcare quality includes the Hospital Safety Score Grades which award a letter grade representing performance for 30 evidence-based measures of patient safety. An “A” represents the best Hospital Safety Score, followed in order by “B,” “C,” “D,” and “F.” In the fall of 2014, Piedmont’s Hospital Safety Score Grade for its five hospitals included four “C’s” and a “D.” This demonstrated a need to change its approach to quality improvement and ensure proper resources were allocated and aligned with the value chain, enabling it to efficiently conduct surveillance activities, perform analysis, and facilitate sustained outcomes improvement.
To increase capacity for performing more value-added work, Piedmont leveraged its analytics platform to automate surveillance activities and monitor the effectiveness of quality improvement efforts. These tools helped Piedmont redesign its quality improvement efforts.
Quality improvement (QI), the systematic and continuous actions that lead to improving services and health status, is critical to effective healthcare delivery, and reducing unintended variability in care.1,2 Successful QI programs include four key principles: QI work as systems and processes, priority placed on the patient, an emphasis on being part of the team, and a focus on using data for improvement.2
Piedmont Healthcare, a private, not-for-profit organization serving nearly two million patients across Georgia, is transforming healthcare, creating a destination for the best clinicians, and a one-of-a-kind experience that always puts patients first. Piedmont is known as a leading health system in cancer care, treatment of heart disease and organ transplantation, with seven hospitals, 19 urgent care centers, 94 physician practice locations, and 1,615 Piedmont Clinic members.
Piedmont recognized that providing world-class patient care ultimately requires an ongoing commitment to improving patient satisfaction, clinical outcomes, administrative processes and community involvement, and invested resources in its quality improvement department to help foster ongoing improvement.
Despite these efforts, Piedmont was not achieving the desired performance level. In the fall of 2014, Piedmont’s Hospital Safety Score Grade for its five hospitals, a letter grade representing performance for 30 evidence-based measures of patient safety where “A” represents the best Hospital Safety Score, followed in order by “B,” “C,” “D,” and “F,” included four “C’s” and a “D.”
Piedmont identified several barriers impeding its ability to have a successful QI function that reduced variation and achieved sustained outcomes improvement, including:
Additionally, Piedmont’s structure was not conducive to sharing across facilities, further limiting QI efforts.
In reflecting on its QI structure, Piedmont identified that it lacked a quality strategy. The structure of this department had grown organically over time, and each individual hospital was attempting to develop expertise in every domain, resulting in ineffective redundancy. Piedmont needed to change its approach to QI and ensure appropriate allocation of resources aligned with the value chain, enabling it to efficiently conduct surveillance activities, perform analysis, and facilitate sustained outcomes improvement for the patients in its care.
To improve efficiency, creating capacity for more meaningful, value added work, Piedmont redesigned the structure and work of its QI teams, establishing the lofty goal of eliminating all patient harm by 2024. Prior to redesigning the quality function, each facility had independent structures and resources that were focused on hospital specific work. Piedmont changed this, establishing a central quality department supporting the local hospitals.
Rather than having each hospital attempt to invest resources to solve quality problems independently, Piedmont now coordinates the work among hospitals, and prioritizes investment in QI efforts, allocating assets to address those activities that are likely to cause patient harm, aligning work with the value chain. The quality department has been restructured with fresh workflows, identified new roles, and revised job descriptions, aligning skills and resources with four major categories of work:
To increase capacity for performing more value-added work, Piedmont leveraged the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications, to automate surveillance activities, and use the analytics platform as the source of data and analytics for monitoring the effectiveness of quality improvement efforts. Piedmont uses the Central Line Associated Bloodstream Infection (CLABSI) Prevention Advanced Application (Figure 1), enabling the team to efficiently find, review, and document CLABSI cases to support National Healthcare Safety Network (NHSN) reporting, and facilitate monitoring of process measures that have an impact on CLABSI rates.
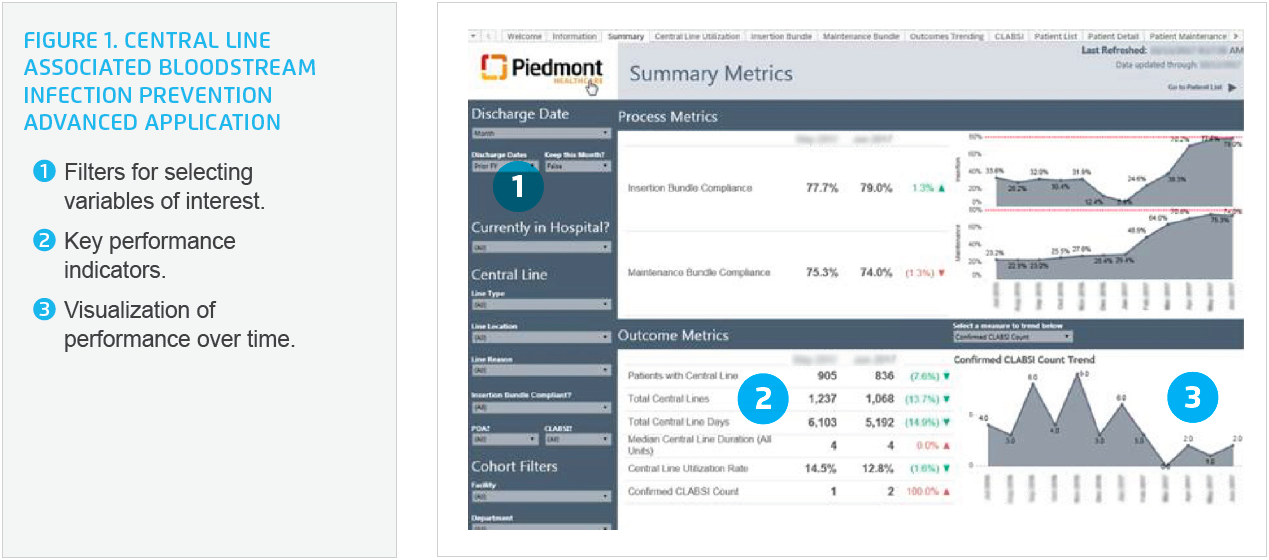
Similarly, the Catheter Associated Urinary Tract Infection (CAUTI) Prevention Advanced Application supports improved NHSN reporting and ongoing QI. Professionals and leaders in this area are able to quickly monitor insertion and maintenance bundle compliance, and observe the impact of the process measures on the CAUTI rate for the organization and individual hospital units. A lab surveillance dashboard has automated a sizeable portion of lab result review, enabling centralized monitoring of surveillance, and improved control of HAIs.
By reducing the resources required for surveillance and analysis, Piedmont can increase the staff available to support quality improvement work, introducing process engineers who partner with clinicians to accelerate improvement.
Piedmont uses a structured approach to QI. When a problem is identified, and prioritized as having the potential for harm, Piedmont allocates resources, including process engineers and clinicians, to improve the processes of care. The QI team develops a project charter, including definition of the scope, timeline, team and subject matter experts needed, and the business case.
After developing a project charter, the team identifies the current state, maps the existing process, compares that method to evidence-based practices, performs chart review, observes the workflow at a unit level, and uses data and analytics to better understand the current state, informing the development of an improved future state.
The team then moves on to engaging subject matter experts and stakeholders in developing, and documenting, the ideal future state. The future state documentation includes (as appropriate):
Once the future state is defined and fully-documented in a central location, referred to as the “Promise Package,” the team pilots the proposed changes. This step allows the team to work on the proof of concept, obtain stakeholder, clinician, and hospital leader feedback, and provides for completion of validation testing, and confirmation of process measures. Once the pilot demonstrates effectiveness, the team obtains approval to move forward from the appropriate governing body.
The system chief executive officer, chief medical officer, chief nursing officer, and the executives at the hospital location where the change is occurring review and approve the proposed future state, assign resources to support the implementation plan, and identify local resources who will assume responsibility for monitoring and reporting out on compliance to the standard work.
Implementing changes is led by the local chief medical officer and director of quality improvement, and is supported by a process improvement lead. The implementation plan includes delivery of the “Promise Package,” active coaching, and at-the-elbow support on all shifts for a minimum of two weeks. During this two-week period, resources are available at a unit level, helping staff locate the policies, procedures, and standard work outlined in the “Promise Package,” helping leaders utilize the analytics applications, surfacing and resolving barriers, issues, and questions from the frontline staff.
For each improvement project, Piedmont establishes a 60-day plan for the post-implementation period. The QI team supports local operations using, applying, and improving the “Promise Package.” During this time, the team partners with local leadership, conducting rounds at the unit level to solicit barriers and issues. Following 60-days, and resolution of barriers and issues, responsibility is handed off to local leadership, who ensure ongoing monitoring and continuous improvement. Responsible leaders report out on both process and outcome measures—even in the absence of any infections—and are accountable for ensuring compliance to the standard work.
Redesigning the hospital quality function around the value chain, a rigorous process for quality improvement, standard work, analytics, accountability, and ongoing performance feedback has helped Piedmont achieve sustained outcomes improvement, including a:
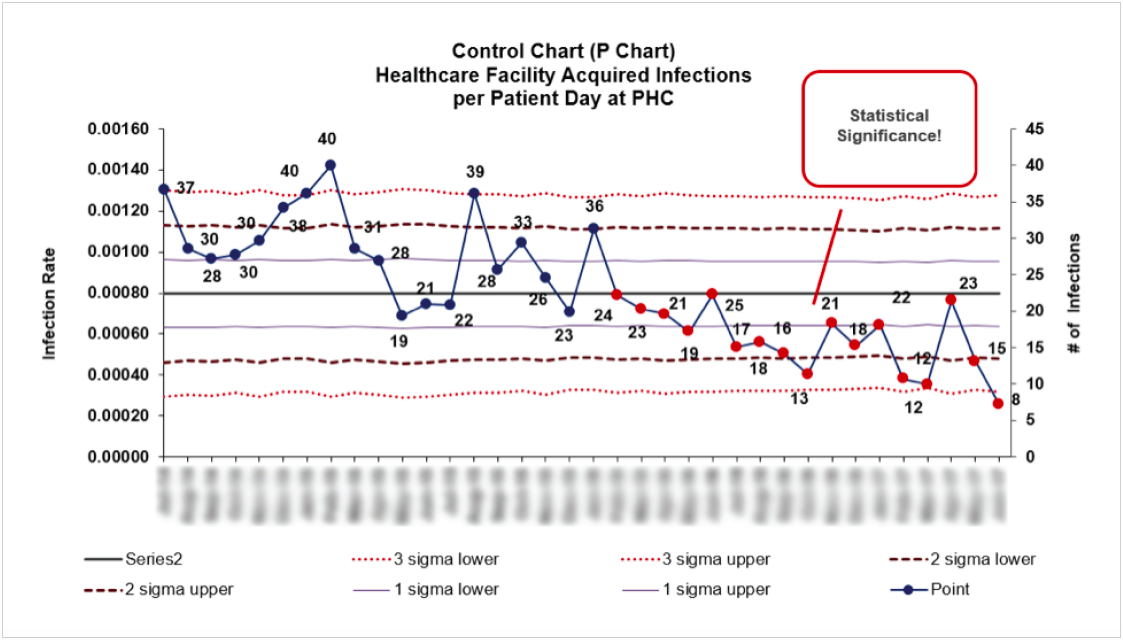
The redesign of the quality department is also improving efficiency. Piedmont has achieved a 50 percent reduction in the time required for peer review, and has doubled the number of active QI projects, while achieving a 50 percent reduction in the time required to implement improvement projects.
“We’ve dramatically changed our approach to quality. We are no longer sitting in a room discussing a problem, but actively working on the elimination of patient harm.”
– Leigh Hamby, MD, MHA, Chief Medical Officer, Piedmont Healthcare
Piedmont is focusing on continual improvement, developing real-time support tools for nursing to support workflow, decision making, to provide feedback regarding compliance, and on reducing the documentation burden for clinicians. The organization is also continuing to identify opportunities to leverage analytics and automated systems to free up labor resources, and is working at improving workflow to drive down labor costs for accreditation.