Thibodaux Regional Medical Center prioritizes continuous improvement in patient care. Guided by a methodology recognized by The Joint Commission, the organization employs a three-systems care transformation model that includes best-practice care protocols, near real-time analytics, and rapid implementation of analytics applications to enhance patient outcomes.
Thibodaux Regional Medical Center has always excelled in delivering quality care to its patients, but a fundamental tenet of its culture is continuous improvement.
Driving that continuous improvement is a methodology The Joint Commission called “best practice in how to use data and get physicians engaged.” This improvement methodology centers around a three-systems care transformation model that includes best-practice care protocols, near real-time analytics, and rapid time-to-value analytics application development and implementation.
The Joint Commission (TJC) accredits and certifies nearly 21,000 healthcare organizations and programs in the United States.1 As an independent, not-for-profit organization, TJC serves as a symbol of quality that reflects a healthcare system’s commitment to meeting CMS and TJC performance standards including standards for implementing a quality improvement methodology.
In order to be granted accreditation, a hospital must create and execute an annual performance improvement plan that prioritizes the healthcare needs of the health system’s community. The organization must set measurable goals as part of the plan and show metrics for improvement toward meeting those goals.
Thibodaux Regional Medical Center is a TJC-accredited hospital that delivers healthcare for the Thibodaux, Louisiana community located about an hour southeast of New Orleans. Thibodaux Regional is committed to creating a premium-value enterprise in its community by achieving patient-centered excellence through working smarter.
Thibodaux Regional’s pathway to achieving this excellence includes four components:
Effecting change in a community hospital is a different process than in a large academic organization. Physicians, nurses, and other caregivers all care about what happens to their patients in any size institution, but in a community hospital, the ability to mandate change doesn’t exist. While community hospitals do have the ability to institute change faster, they must create excitement and show data to change minds about how to best care for patients.
Clinical improvement requires engaged physicians, complete transparency, agile analytics, and early success to motivate the team to spread the new practices. Thibodaux Regional needed a systemized and organized approach to consistently create that dynamic for its quality improvement teams, so it instituted a care transformation organizational structure (see figure 1).

A steering team of three physician leaders, the chief executive officer, the program coordinator, the vice president of quality and compliance, the chief nursing officer, and the chief information officer provides overall governance and prioritization of initiatives.
Other elements of the structure include a content and analytics team, an MD advisory council, and a guidance team that, together, provide support to the clinical implementation teams. It is the clinical implementation teams (also called clinical improvement teams) that drive quality and process improvement efforts.
With the support of the steering committee, the clinical implementation teams identify and organize the right people to inspire a high level of physician engagement and clinical collaboration. This in turn drives clinical improvement and engenders a sense of excitement about changing clinical practice.
Each clinical improvement team is given the right tools and the right environment to succeed. These include executive and physician leadership, a wide base of clinical expertise, established (and clear) goals and aims, and analytic support and feedback. To make them more effective, teams receive support from someone very knowledgeable in hospital operations and process improvement, and who can facilitate meetings and checkoff action items.
It’s also essential that the team leader build a relationship with all members of team, especially at the beginning. The leader ensures the team’s continual progress toward goals and makes sure all members have input and feel valued.
Clinical improvement teams all go through the forming-storming-norming-performing model of group development, but they need nurturing and guidance to do so. At the beginning, Thibodaux Regional set these ground rules and followed them.
Thibodaux Regional bypasses the tension that can exist between clinicians and administration because it has an engaged, adaptive leadership team, and it established an improvement and data-literate culture. This enables ongoing dialogue between these two groups. The leadership team participates in setting up the clinical improvement teams, as well as the high-level strategy and goals. But the real key is when the leadership team turns over the “how” to the clinicians and implementation teams after setting expectations.
The other key component is effective, near real-time analytics that provide information about results and the effect of interventions on clinical outcomes.
With its organizational structure in place and clinical implementation teams identified and ready, Thibodaux Regional ensures positive change in its clinical outcomes through a care transformation model. This model is based on three systems of care transformation (see figure 2).
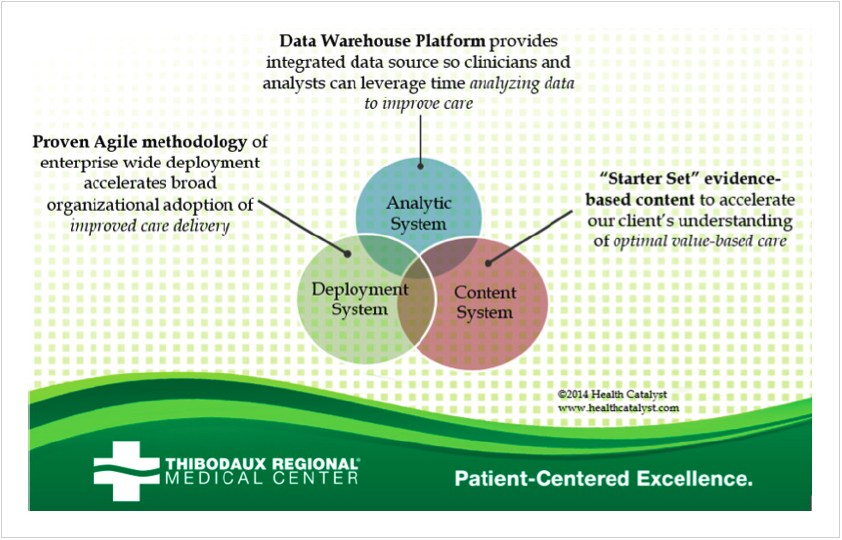
Optimized care delivery requires excellence in all three systems:
The clinical implementation teams execute this care transformation model effectively through training and support.
During its recent TJC survey, Thibodaux Regional shared its quality improvement methodology and improvement team results. The upshot of all this hard work? Thibodaux Regional received unprecedented approval from the surveyors. At the executive briefing, which is part of the survey, TJC commented:
“This is the most sophisticated and comprehensive system I have ever seen… [Thibodaux Regional’s methodology] is a best practice in how to use data and get physicians engaged.”
“Care Transformation has broadened the knowledge base of docs and staff and changed their paradigm. It has proven to them that taking steps to improve care with protocols, bundles, and pathways can save people’s lives in this community. This has convinced them that the process is worth the effort. This is a win throughout the organization.”
– Greg Stock, CEO
With a realistic and effective improvement model led by its CEO and implemented by capable teams, Thibodaux Regional is applying care transformation to sepsis, acute myocardial infarction, and colon oncology.