Community Health Network (CHNw) observed higher than national rates of maternal substance use disorder, with a higher number of pregnant women having positive drug screens for opioids, cocaine, amphetamines, barbiturates, and benzodiazepines. It developed a care coordination and substance use program to help reduce the incidence of substance use disorders among pregnant women. Using its data platform and analytics applications, CHNw was able to evaluate the impact of various process measures on patient outcomes.
Neonatal abstinence syndrome (NAS) is a group of problems that occur in a newborn when withdrawing from exposure to opiates. In the U.S., a baby is born with symptoms of NAS every 15 minutes. Between 2004 and 2014, inflation-adjusted hospital costs for NAS increased by $472M.1
Ranked among the nation’s most integrated healthcare systems, Indianapolis-based CHNw is Central Indiana’s leader in providing convenient access to exceptional healthcare services. Nearly 8,000 births occur at CHNw hospitals each year. Twenty percent of babies born in Indiana test positive for opiates.
Several state governments have responded to the increase in opioid use during pregnancy by prosecuting and incarcerating pregnant women with substance use disorders. That approach has no proven benefits and may decrease the willingness of women to engage in substance use disorder treatment programs.2 CHNw opted to take matters into its own hands and find a way to improve outcomes for babies and mothers exposed to opiates
CHNw observed rates of maternal substance use disorder in its patients that were higher than the national average. Many pregnant women screened at CHNw for drugs tested positive for opioids, cocaine, amphetamines, barbiturates, and benzodiazepines. At the Community Hospital East location, a total of 42 percent of babies were exposed to illicit substances, and the organization was losing an average of $12K for each NAS diagnosis, as the cost of care was substantially less than the reimbursement received.
Worse yet, the number of babies diagnosed with NAS was increasing, mirroring the growth of the opioid epidemic. Despite this concerning trend, there were limited treatment options for women with substance use disorders. Rather than continuing to react to this challenge by treating an ever-increasing number of babies with NAS, CHNw needed to get upstream of the problem, intervening to reduce the incidence of substance use disorders among pregnant women.
In response to the growing concerns related to NAS, CHNw opted to develop, implement, and evolve a program for pregnant women struggling with substance use disorders. The organization started offering medication-assisted treatment (MAT), which involves the use of medications in combination with counseling and behavioral therapy to treat substance use disorders. An obstetrics and gynecology (OB/GYN) physician and nurse practitioner obtained licenses to prescribe buprenorphine for the treatment of opioid use disorder. Both are trained to address the unique needs of patients struggling with substance use disorders.
Over time, CHNw further developed the support available to women, offering patients the opportunity to participate in its CHOICE (Change, Hope, Overcome, Inspire, Compassion, Education) program—a program for pregnant women struggling with substance use disorders. The OB/GYN and nurse practitioner lead the CHOICE program, which has the flexibility to leverage various expert resources available either on-site or via telehealth that may help improve outcomes for patients. The goal is to help each patient get into a treatment program that works for her and to support her on the path to recovery.
Community Hospital East became a center of excellence in the care of mothers and babies that have been affected by substance use disorder. The labor and delivery (L&D) unit at Community East offers a team of registered nurses (RNs) trained in trauma-informed care, and specifically trained to provide care to these patients, who work with the CHOICE care team to provide exceptional care. From detoxification to delivery, patients are treated with dignity and respect.
To identify women who could benefit from the CHOICE program, CHNw performs universal maternal testing at the first prenatal visit, and again at presentation for delivery. Clinicians screen patients verbally, requesting permission for a toxicology test. Some patients have entered the CHOICE program after presenting to the emergency department for hydration and management of hyperemesis after unsuccessfully attempting to detox at home; others are referred to the program by people in their social network.
CHNw takes a non-punitive approach for toxicology testing and does not automatically report pregnant women with a positive drug screen to child protective services. Rather, the organization focuses on immediately providing these women the support required to help them to stop using substances.
Patients with a positive result are immediately offered:
Patients who could benefit from buprenorphine treatment meet with one of the buprenorphine subscribers. CHNw proactively removes barriers to program enrollment and participation, meaning its patients do not receive a referral and then wait weeks for an appointment. CHNw patients are not left to navigate the complex health system or coverage issues on their own. Maternity and postpartum patients in acute crisis are seen immediately, and the interdisciplinary team—including behavioral health coordinators, RNs, and social workers—provides care that supports the patient’s goals.
Some patients may want to quit using the substances they have been abusing and want to be able to parent their child; others may have different goals, such as using fewer substances. Patients receiving buprenorphine are scheduled to attend weekly counseling sessions. Patients may also be offered inpatient detox on the labor and delivery unit.
CHNw provides wrap-around services, supporting each patient in achieving her specific goals. The organization helps patients with challenging day-to-day issues, such as a lack of housing or issues with safety, while also offering emotional and medical support to ensure they meet long-term treatment goals. The team offers patients flexible treatment options, fortification, and forgiveness. Patients are not “fired” from the program for arriving late, missing appointments, or other issues related to adherence. The CHOICE program recognizes that confounding factors impact patient behavior, and provide the patient the support needed to be able to effectively participate in the program.
For example, it is not uncommon for the patients to lack transportation, making it difficult to arrive at a scheduled appointment on time. One patient was interested in completing inpatient treatment but was concerned about leaving her beloved dog with her boyfriend. Social workers assisted the patient in locating emergency foster care placement for the dog so the patient could complete inpatient detox.
The interdisciplinary team coordinates patient care, providing an effective hand-off to the L&D inpatient unit for delivery, and informing the special care nursery staff of the patient’s delivery plan and expected delivery date, ensuring the special care nursery is prepared to provide care to a baby who is likely to experience NAS. CHNw performs umbilical cord drug screens for babies born to mothers with a history of substance use and/or a positive tox screen upon admission. This screening is also conducted if the patient refused an ambulatory drug screening.
Babies identified as being exposed to opioids are monitored for signs of withdrawal for five days. Those who experience NAS receive pharmacological treatment to manage symptoms and prevent complications. Affected babies also receive non-pharmacologic care, including a low-stimulating environment, breastfeeding on demand, rooming in with their mother, and “cuddlers” who help snuggle the babies, decreasing uncomfortable stimulation, lessening crying time, and helping the babies to sleep peacefully.
After delivery, CHOICE program participants are connected with another provider to continue their long-term MAT.
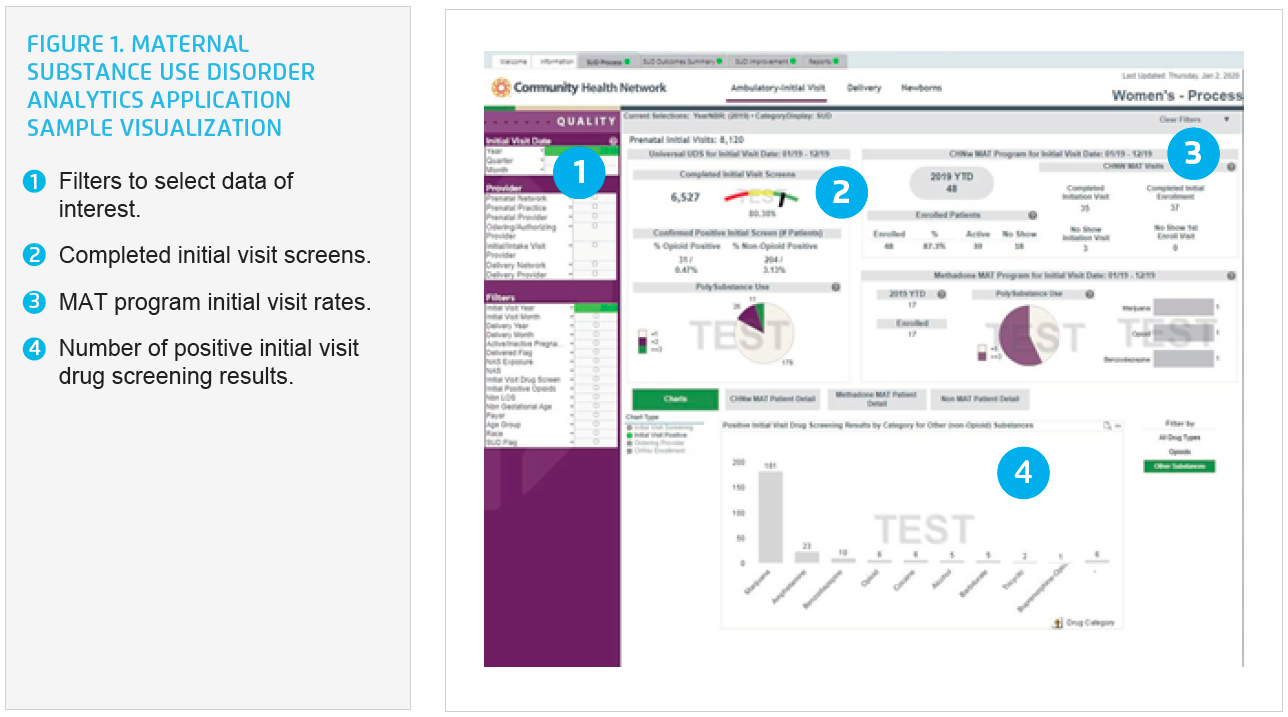
CHNw leverages the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications, including a maternal substance use disorder analytics application, to understand the needs of its patient population, and to evaluate the impact of various process measures on patient outcomes.
Using the analytics application, CHNw can easily visualize the number of patients receiving buprenorphine, along with the number of patients taking methadone, and evaluate the outcomes for each group (see Figure 1). The organization can easily compare differences between groups, including maternal and neonatal LOS, and variable cost. This allows providers to easily visualize the number of patients who tested positive for opiates during the prenatal period who were subsequently negative for opioids at the time of delivery, so the effectiveness of all interventions can be properly evaluated. CHNw is able to answer specific questions about its patient population, and can quickly identify changes in the patient population, enabling it to adjust its program offerings to better meet patient needs.
CHNw’s CHOICE program meets the needs of women with maternal substance use disorder, and has positively impacted patient outcomes and financial performance. Results include:
“It is an incredible gift to have access to real-time data. We’re able to use the analytics platform to immediately demonstrate the clinical benefit of the universal drug screen, and our medication-assisted treatment program for both mom and baby.”
– Brooke Schaefer, MSN, FNP-C, RN, Director Perinatal Substance Use Disorder Program, Nurse Practitioner
CHNw plans to continue to grow the CHOICE program to meet patient needs, also opting to continue to advance analytics within the organization to help facilitate outcomes improvement. The organization is also working to ensure the well-being of the CHOICE team care providers and is working to prevent burnout.