Thibodaux Regional Medical Center sought to reduce care variation and standardize labor and delivery care. Utilizing Health Catalyst solutions, the care transformation team analyzed data to identify improvement opportunities. Enhanced provider education, redesigned workflows, and standardized protocols resulted in cost savings and improved patient outcomes.
One in three women delivers via cesarean in the U.S., and more than 90 percent of them have repeat operations in subsequent deliveries. Despite numerous evidence-based guidelines and established best practices for labor and delivery, clinical care varies widely for many practices. Labor and delivery care varied at Thibodaux Regional Medical Center, causing the organization to look for ways to standardize care. While there was a general awareness that care could be improved, specific, detailed information that provided insight into the opportunities to support prioritization and decision-making was lacking.
To better understand variations in care, and opportunities to reduce its cost, the labor and delivery care transformation team at Thibodaux Regional used the Health Catalyst® Labor and Delivery Advanced Application as well as the Financial Management Explorer application, which integrates data from billing and costing, and creates snapshots of current financial metrics.
Informing and educating providers with provider-specific data in conjunction with redesigned workflow, standardized supplies, and new, standardized protocols enabled the labor and delivery care transformation team at Thibodaux Regional to experience cost savings and improved outcomes.
Induction of labor, using medications or other methods to instigate labor, has contributed to an increase in cesarean rates. The American Congress of Obstetricians and Gynecologists recommends that induction not occur at all prior to 39 weeks, and then, should only occur when the cervix is “ready” for labor.
Inductions, particularly when the cervix is not ready, carry risk, including increased risk of infection, uterine rupture, fetal death, and an elevated risk of cesarean birth.1
The national cesarean rate began to rise in 1996, ultimately peaking in 2009 with a seven-fold increase.2 Today, one in three women deliver via cesarean.3 Decreasing the incidence of first-time cesareans, and increasing the number of women who are successful in completing a normal, vaginal delivery, has a long-term impact on cesarean rates—more than 90 percent of women in the U.S. who undergo a cesarean delivery have repeat operations in subsequent deliveries, and one-third of all cesareans in the U.S. are a repeat cesarean.4
Thibodaux Regional Medical Center, the recipient of the 2016 Women’s Choice Award – America’s Best Hospital for Obstetrics, is driven by its commitment to excellence. Among its top priorities is ensuring that it provides the highest quality patient care, including looking for ways to create improvements in labor and delivery.
Thibodaux Regional’s care transformation teams are focused on the triple aim—improving the quality of care, reducing the cost of care, and enhancing the patient experience. Within the labor and delivery care transformation team, there was a general awareness that variations in care were present and that there was a potential opportunity to improve upon the triple aim.
Despite the notion of variations, specific, detailed information was lacking to support teams in delivering on the triple aim. It would take leaders and analysts between days and months to perform the burdensome chart review required to provide data regarding performance. As such, the data would immediately be outdated and was difficult to use for meaningful improvement. Because it was so difficult to obtain performance data, long-term data was not available, further limiting the understanding of performance over time and restraining effective prioritization of improvement activities.
Thibodaux Regional needed better data that could support its labor and delivery care transformation team in its efforts to achieve the triple aim through improving the quality of care, reducing related costs, and enhancing the patient experience.
Thibodaux Regional relies upon the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications, for data and analytics to support its care transformation efforts. To better understand variations in care, and opportunities to reduce the cost of care, the labor and delivery care transformation team used the Financial Management Explorer application, which integrates data from billing and costing, and creates snapshots of current financial metrics (see Figure 1), as well as the Labor and Delivery Advanced Application.
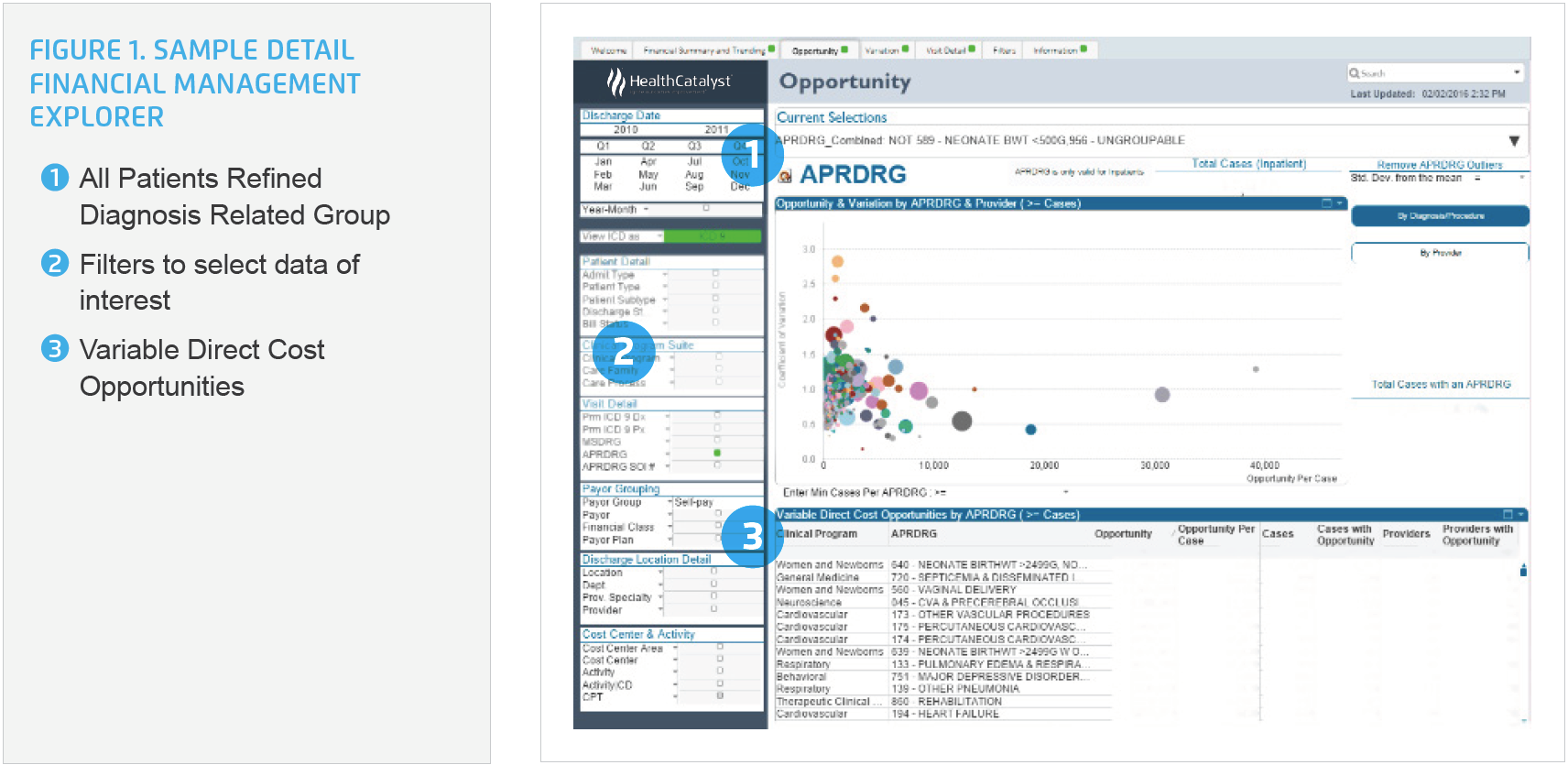
Using the Financial Management Explorer application, the team identified that the two highest cost areas with the largest variability were vaginal deliveries, driven by total labor minutes and drug usage, and cesarean deliveries, with costs driven by total operating room (OR) time. As such, these two areas were prioritized for improvement.
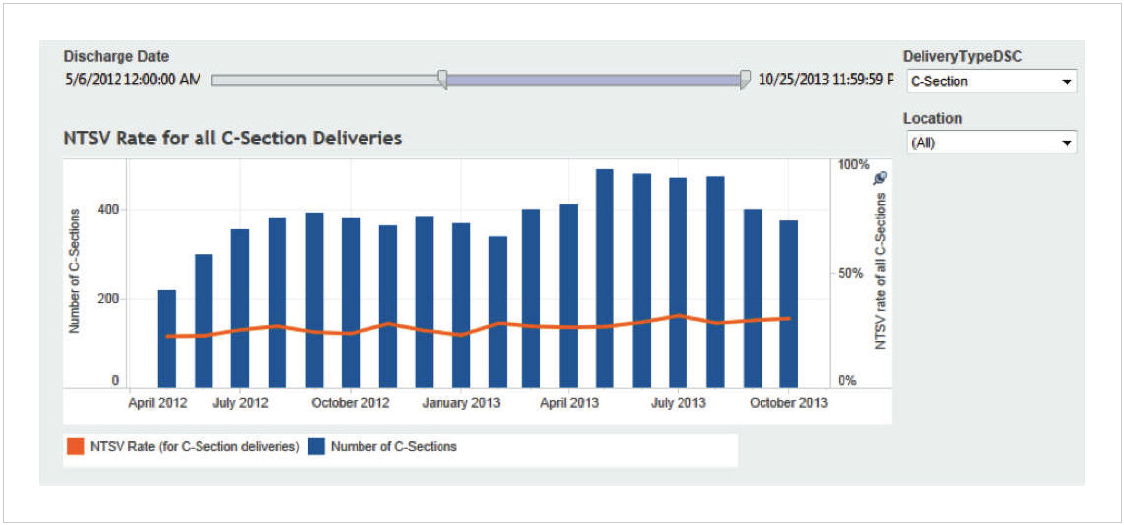
The Labor and Delivery Advanced Application provided the care transformation team detailed insight, including an overview of all deliveries in the health system, the data required to meet The Joint Commission PC-01 (elective deliveries), and PC-02 (Cesarean deliveries for NSTV), and key interventions for the antepartum period, such favorable induction compliance (cervical readiness) and LOS hours, including door to delivery (see Figure 2).
Prepared, for the first time, with comprehensive data, the labor and delivery care transformation team prioritized opportunities for improvement, selecting to invest resources to decrease the average variable cost for uncomplicated vaginal and cesarean deliveries. The team established cost quality goals, redesigned the induction and cesarean section workflow to make it consistent, standardized supplies, and shared provider-specific performance data to engage physicians in reducing cost while maintaining patient satisfaction and high-quality care.
To engage providers, the team included them in the improvement process efforts and shared provider-specific performance data with them. For many, this represented the first time they received their specific performance data.
The sharing of reliable, valid, provider specific data was key in garnering support for change. Previously, providers lacked data, making them largely unaware of opportunities for improvement, and without knowledge of how their performance, particularly for items like supply usage and cost, compared to their peers. The analytics application made it convenient for the team to easily compare and evaluate the use of medications and supplies, and clearly identify the impact on both cost and patient outcomes. The team engaged providers and registered nurses (RNs) in discontinuing the use of costly medications and supplies that did not result in a better clinical outcome for the patient.
Members of the team observed the nursing workflow, monitoring both newer and experienced RNs. In doing so, they identified several opportunities to streamline activities, standardize processes and eliminate waste. The team used available literature and best practices to develop a comprehensive favorable induction protocol, redesigning workflow and documentation requirements to ensure consistency and efficiency.
When scheduling inductions, physician offices now have one point of contact. In addition to communicating the indication for induction and relevant patient history, physicians ensure they also convey the Bishop score, a method used to determine the readiness of the cervix for labor, to the nursing staff. This is an important piece of information as women whose cervix are ready, labor for a shorter time and are less likely to have a cesarean section.
Upon patient arrival, the nursing staff also assess the Bishop score. Leaders use the analytics application each day to review the required documentation, consistency between the two Bishop scores, and the patient outcomes. The data from the analytics application is used to provide feedback to the nursing staff and physicians, and to help ensure continued adherence to the standard induction protocol.
The workflow for cesarean deliveries within the OR has also been standardized. A checklist of the sequential activities that are to be performed after the patient’s spinal is complete, and prior to the incision, is displayed in the OR, serving as a reminder for the most efficient, effective sequence for essential activities.
To support physicians in communicating to their patients the importance of waiting until at least 40 weeks for induction, 41 weeks in many cases, the team developed patient education materials, including posters hung in the exam rooms. Over the course of the pregnancy, physicians engage the patient in a discussion about the importance of delaying induction until the pregnancy has progressed, the baby is fully developed, and the mother’s body is prepared for delivery.
Thibodaux Regional’s labor and delivery improvements impact cost and outcomes, and the transformation team is delivering on the triple aim, achieving impressive results.
“If you save someone from that first cesarean, it is important as it sets the stage for future success in vaginal deliveries.”
– Richelle Dufour, RN, BSN, Clinical Director, Women’s Center of Thibodaux Regional
The labor and delivery care transformation team is continuing to pursue opportunities for improvement and is working on standardizing the care provided to patients during the recovery period. The team expects further reductions in the nulliparous cesarean rate and anticipates that they will further reduce costs.