Healthcare organizations must prioritize effective revenue cycle management to maintain financial health. Timely identification of claims issues is crucial for revenue recovery. This large health system improved its revenue cycle processes by adopting a healthcare analytics solution, significantly reducing rework.
With cash flows declining, margins tightening and bad debt increasing, it’s more important than ever for healthcare organizations to maintain their bottom line. Efficient, effective revenue cycle management that ensures timely and accurate payment is one key to an organization’s financial health.
To catch and address issues that prevent claims from being paid, revenue cycle teams need the ability to easily access data throughout the cycle. Because claims are processed every day, these teams need to constantly monitor trends and variances and quickly identify and address the root cause of performance issues. Prompt identification is critical. The further a processing error moves through the cycle, the harder it is to recover the lost revenue associated with that error. In addition to potential lost revenue, the inability to identify errors up front can result in substantial rework and lost productivity for revenue cycle teams.
One large, internationally renowned health system was facing significant challenges in its revenue cycle management processes. For several years, the organization had tried to improve these processes—including upgrading its revenue cycle management system—with little success. This paper explores how by simply adopting a healthcare analytics solution the health system was able to at last improve revenue cycle management and reduce rework.
The health system had made a significant investment in a revenue cycle management technology solution, but only 15 percent of the revenue cycle team was actually using it. The team didn’t trust the system because it had too many data integrity and data modeling calculation issues.
One data integrity problem was that the system wasn’t calculating denial rates properly. Instead, to get accurate denial rates the team had to work extensively with the business intelligence (BI) department. BI would pull data from the clinical system and then write complex reports. The number of reports that the revenue cycle management team requested from the BI team was staggering—and there was no centralized effort to keep track of which reports were being created or by whom at any given time.
Furthermore, the data for these fragmented reports was being pulled from a flat file created on a weekly basis. Sometimes the level of granularity needed to discover the root cause of an issue didn’t exist in the flat file data. This necessitated follow-up report requests to the BI team, which resulted in ever-increasing report queues.
This manual reporting process contributed to a significant problem with data timeliness—and timely data is critical to managing accounts receivables and denial rates. Unfortunately, the data the revenue cycle team received from the flat files lagged by as much as a week to ten days. In addition, due to the enormous BI reporting queue, the turnaround times for custom reports could be as many as 30 days. By then, the revenue cycle team’s window to revisit claims with insurance providers had sometimes closed.
Finally, data integrity issues were requiring the revenue cycle team to perform a significant amount of manual rework. Because they didn’t trust the data, the team felt the need to manually perform calculations to verify that the data was accurate.
To have a more coordinated, efficient revenue cycle management effort that maximized revenue generation, the revenue cycle team needed to:
The health system turned to Health Catalyst’s Late-Binding Enterprise Data Warehouse™ (EDW) platform for a solution. The organization had already deployed the EDW to drive clinical and operational performance improvement initiatives. This EDW aggregates data from the electronic health record (EHR), financial systems and more to create an enterprise-wide, consistent view of all of the health system’s data—a single source of truth to inform business decisions.
To use this solution to address the healthcare revenue cycle, the health system deployed the Health Catalyst Revenue Cycle Explorer financial application on top of the EDW platform. The application is a full-service solution where all key revenue cycle management metrics reside in one place as a single source of truth, eliminating the need for manual report creation, distribution and file extraction. Revenue Cycle Explorer helps the healthcare organization identify macros issues—versus reviewing claims in a piece-meal fashion— resulting in cleaner claims submissions and reduction in costly rework.
Using the application, the revenue cycle team can drill into financial metrics and perform analyses at the granular level. This drill-down ability enables them to find answers on their own and eliminates the majority of the reporting requests to BI previously needed to investigate a performance issue. The key revenue cycle metric calculations are built directly into the application—and since the data in the application links directly to the source systems, timeliness and data integrity have also been addressed.
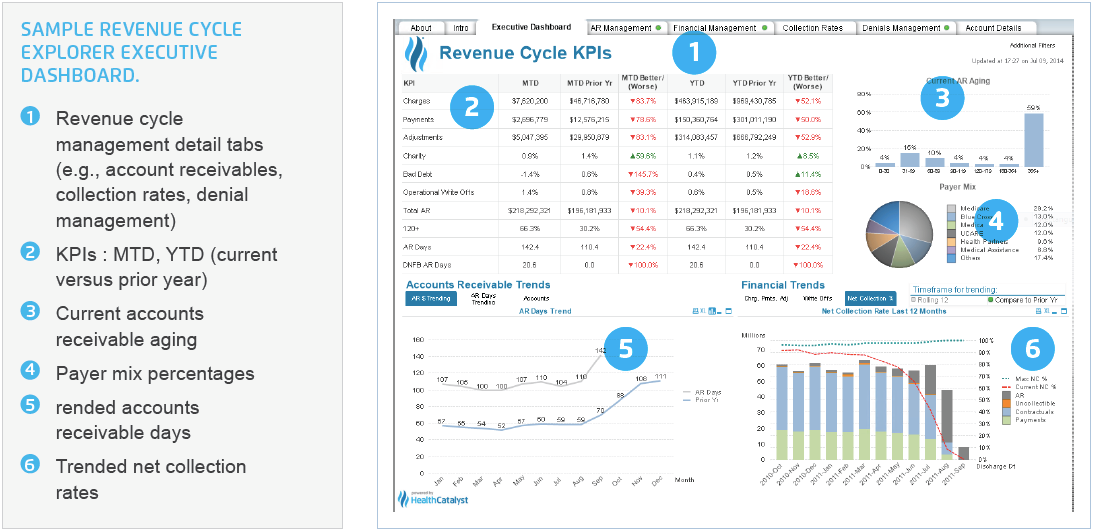
The Revenue Cycle Explorer executive dashboard (Figure 1) provides a high-level view of key performance indicators (KPIs), with trending data to quickly enable comparisons of any variances to prior periods. This dashboard enables the user to quickly internalize the overall health of the revenue cycle.
The application enables the team to identify operational problems that can lead to denials. Figure 2 shows an example of the denials management dashboard that arranges denials into actionable categories. The revenue cycle team can quickly research by variance, denial code, location, payer, provider and CPT code (for professional billing) to identify root causes before they turn into larger problems. The team can drill down within claims all the way to a specific patient or particular charges for that patient.

Since the data in Revenue Cycle Explorer is updated in near real-time, the revenue cycle team can access the application at any time to get the most up-to-date information, enabling them to more effectively manage their revenue cycle. The team is able to identify and resolve issues more quickly, enabling earlier revenue generation for the healthcare organization.
The healthcare system was able to eliminate its previous revenue cycle IT solution provider for their professional component billing. Additionally, they were able to reduce manual data extracts, manual one-off reports, and manual report distribution, freeing up the BI team to focus on strategic reporting needs. The BI reporting queue has been reduced by 30 percent. As a result, the organization has realized an estimated $400K in operational savings.
One hundred percent of the revenue cycle team now trusts the accuracy of the data because it has been validated within the EDW. This trust in the data has eliminated the need for one-off BI reporting requests. In addition, the team no longer feels the need to manually perform their own calculations to ensure the data is accurate, avoiding rework. Revenue Cycle Explorer automatically calculates what was being manually calculated before—and since the data in the calculations comes directly from the EDW, accurate data modeling is ensured. Rather than spend hours on calculations and manual reporting, the team is able to dedicate their time to using the application to arrive quickly at the root cause of revenue cycle performance issues and to resolving them more quickly.
“This application gives me instant insight into our revenue performance. I don’t have to pull together a number of reports to see how successful we are being at collecting timely payment. All the pertinent aspects of the revenue cycle are here in front of me on the dashboard.”
– Revenue Cycle Manager
The organization has established benchmarks for key healthcare revenue cycle measures such as claims denials, underpayment and accounts receivable aging. With these validated baselines in place, the team is ready to measure the improvement in the health system’s revenue cycle management going forward.
Would you like to use or share these concepts? Download this quality improvement presentation highlighting the key main points.
Click Here to Download the Slides
https://www.slideshare.net/slideshow/embed_code/key/cxou9WNeZ5yOAy


