Mission Health sought to address overcrowding in its emergency department, where 4,000 patients were leaving its ED each year without being seen. By implementing an improvement process using an analytics platform, the hospital focused on staffing, registration, triage, and early provider access, leading to significant enhancements in ED performance and patient care.
Overcrowding in the emergency department (ED) has been associated with increased inpatient mortality, increased length of stay (LOS), and increased costs for admitted patients. ED wait times and left without being seen (LWBS) rates—patients who present to the ED but leave before receiving a medical evaluation—are indicators of overcrowding.
Mission Health needed to address overcrowding in its ED. The community hospital system confirmed overcrowding when it determined that approximately 4,000 patients were leaving its ED each year without being seen.
Mission implemented an improvement process to address ED overcrowding. The hospital leveraged its analytics platform to develop an ED analytics application that provided actionable, timely ED performance data to focus improvement efforts on four areas: staffing patterns, registration, triage assessment by the registered nurse (RN), and early access to a qualified medical provider.
Emergency department triage is increasingly instrumental in ensuring high-quality, timely care. As ED volumes have increased, so have wait times. ED wait times and LWBS rates are indicators of ED overcrowding. Overcrowding is associated with increased inpatient mortality, increased LOS, and increased costs for admitted patients.1, 2 Additionally, the time from patient arrival to the first contact by a qualified provider plays an important role in ED wait times.3
Mission Health’s Emergency Services includes western North Carolina’s designated Level II Trauma Center at Mission Hospital, select telehealth specialties at regional hospitals with medical direction provided by Mission Hospital-based specialists, ground transportation by Regional Transport Services (RTS), and air transport provided by Mountain Area Medical Airlift (MAMA)—both transportation services can provide transport for neonatal patients.
Mission strives to provide world-class care to people and their families when they need it most with the aim to get every person to the desired outcome, first without harm, also without waste, and always with an exceptional experience for each person, family, and team member. The hospital system targeted improving ED care as part of its efforts to better its services overall.
Mission identified that the rate of patients leaving the ED without being seen by a qualified provider was higher than it should be, suggesting issues with overcrowding and wait times. Approximately 4,000 patients were walking out of the ED each year. This patient safety issue was negatively impacting the patient experience. In addition to a high LWBS rate, Mission knew the wait time to see a qualified medical provider after triage was also too long, suggesting larger problems with ED throughput.
Mission ED leadership knew it needed a change, which would require participation from the entire team. The hospital system also knew it needed data to inform timely, meaningful, and scalable adjustments to the delivery of emergency care.
Prior to engaging in process improvement, Mission used the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications for data and analytics to obtain actionable, timely data. Using the analytics platform, Mission developed an ED analytics application (see Figure 1) that provided visibility into ED performance. This included data for patient volume, percent of patients admitted, LWBS rate, door to provider, door to bed, bed to provider, LOS for both admitted and discharged patients, and the longest wait time in the waiting room.
In addition to ED performance data, Mission added real-time data from imaging and laboratory, as well as inpatient bed capacity, to the analytics application. This supported a systems approach to care and provided insight into the status of departments that impact ED throughput.
Using the analytics application, Mission analyzed arrival and throughput data from the previous four years, established baselines and trends, and analyzed the data for opportunities for improvement.
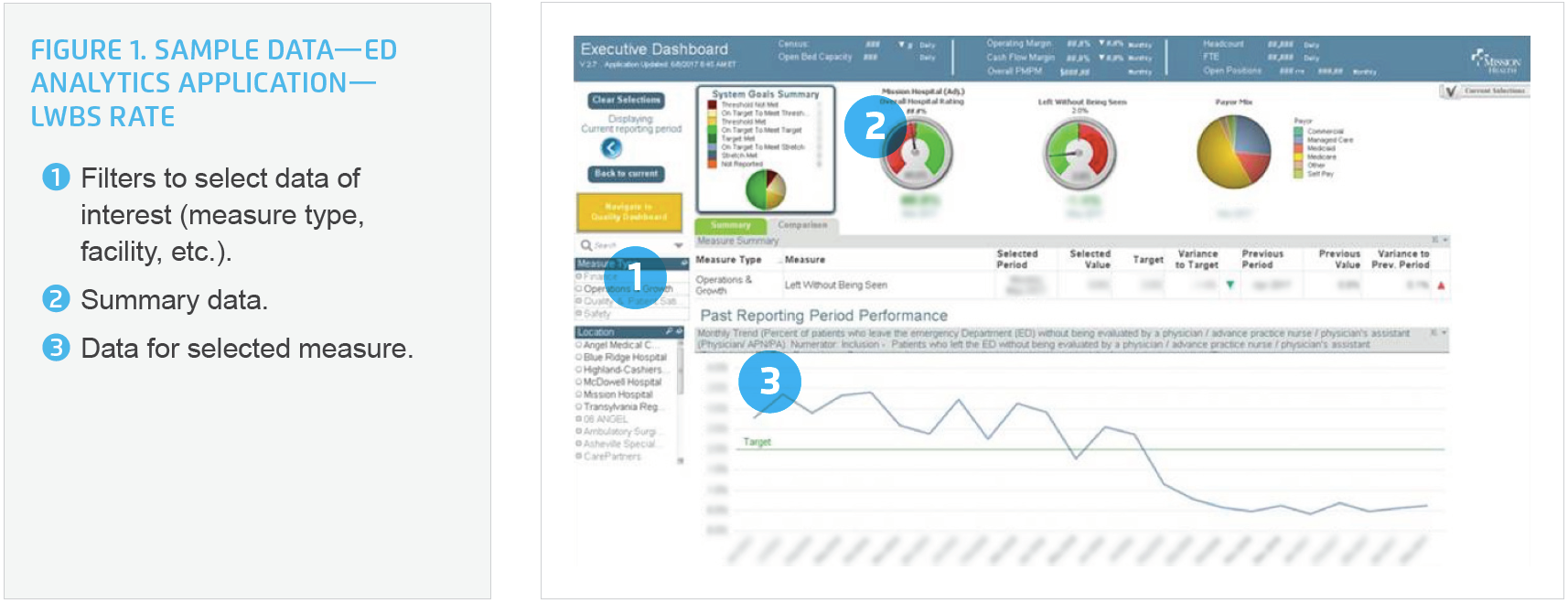
Mission also used data from the analytics application to identify inefficiencies in the ED triage process: the hospital system reviewed performance for door to triage, time to triage complete, and time from triage to bed. It analyzed physical layout and impact on the ED workflow to determine waste in patient and staff movement.
Mission focused its improvement efforts on four areas: staffing patterns, registration, triage assessment by the RN, and early access to a qualified medical provider.
To revise staffing patterns, Mission used the analytics application to review changes in patient arrivals over time (using four years of historical data). The baseline review showed that volume varied substantially throughout the year, particularly during specific seasons and holidays. Mission subsequently adjusted their staffing to better align with patient volumes.
To improve the registration process, Mission instituted quick registration. Registration is a critical component of care, and registration staff must confirm correct patient identification upon patient arrival. Rather than asking a lengthy list of questions that contribute to delays in care, Mission limited triage questions to the minimum required to register the patient and initiate care. To complete the registration process, ED staff now asks remaining questions at the patient bedside during ED stay.
To improve triage workflow, Mission used an evidence-based triage assessment—the Emergency Severity Index (ESI)® triage acuity scale—to determine patient acuity and priority of care at triage. Mission determined that the list of initial questions by the triage nurse were too lengthy. It scaled down the list of questions to ensure a rapid triage process and placement in appropriate care, limiting questions to those needed to determine the severity of illness. Following triage, patients either moved to an ED room or if not critically ill, may have had to wait for care.
Mission identified the opportunity to improve throughput for patients who were not critically ill, as not all patients who visit the ED need life-saving treatment. The hospital system determined they could make better use of its resources, and speed throughput, for this group of patients. To improve care for noncritically ill patients who are not critically ill, Mission developed an Early Team Evaluation (ETE) protocol to determine which patients may be treated and wait safely in a chair in results pending, rather than a hospital bed. The ETE protocol helps to standardize the decision process for patient placement, bed utilization, and appropriate allocation of resources. While people who are critically ill (e.g., those experiencing chest pain or diabetic emergencies) need to be placed in a bed as soon as possible, other patients are appropriate for the ETE protocol. These patients (e.g., those who may have a sprain, rash, or minor respiratory infection) are ambulatory and can safely remain in a results pending waiting area until diagnostic studies are completed, freeing up the hospital bed for more acutely ill patients.
To address the delay in patient arrival to assessment by a qualified provider, Mission developed and implemented a new role—Triage Advanced Practitioner (TAP). This position is an advanced RN practitioner or physician assistant who works in the triage area alongside the triage nurse to help reduce ED wait times. During peak hours, both the triage nurse and the TAP assess patients in parallel. To eliminate wait times and deliver more timely care, the TAP orders diagnostic tests (e.g., imaging, labs, or EKGs) for patients waiting for placement in the ED, eliminating wait times and improving the timeliness of care.
Even with the best possible processes, Mission’s ED still experiences unpredictable surges in patient arrival. To make sure it can meet the needs of patients even when experiencing these fluctuating patient volumes, the hospital system now holds interdisciplinary team-based care huddles at 2:00 p.m. each day. The team uses real-time data to determine adjustments in beds and staffing, and identifies potential bottlenecks and needed changes to prepare for the busy evening shift. Leaders from the ED and inpatient units responsible for throughput also meet at the start of each day; they use the analytics application to identify possible barriers to efficient throughput and develop plans to mediate those barriers.
Using a data-driven, systems approach, Mission dramatically improved ED performance in a little more than a year the hospital system achieved the following:
“The use of the analytics and real-time data are key to our success. Without the real-time data, process improvement is like driving without your headlights—you don’t know if you are making positive or negative gains. We would not have been able to improve without the data.”
– Rick Lee, MSN, RN, CEN, NE-BC, Executive Director, Emergency Services
Mission plans to continue this interdisciplinary approach to improve ED workflow and outcomes. Future activities include expansion of the team-based care huddles to three times daily and expansion of the TAP hours to better align with the peak utilization hours (as identified by the analytics application).