Health equity means everyone should have the chance to live a healthy life, which requires removing barriers to health. The U.S. faces significant health disparities, especially among minority groups. Allina Health sought actionable data to identify and address these inequities. The organization analyzed race, ethnicity, and language data and consulted with patients and community members to create effective interventions. Allina Health is raising awareness about health inequities and taking steps to ensure all patients receive the care they need.
Health equity means that everyone has an equal opportunity to live the healthiest life possible – this requires removing obstacles to health. The U.S. ranks last on nearly all measures of equity, as indicated by its large, disparities in health outcomes. Illness, disability, and death in the United States are more prevalent and more severe for minority groups. Health inequities persist in Minnesota as well, which motivated Allina Health to take targeted actions to reduce inequities.
Allina Health needed actionable data to identify disparities and to reduce these inequities. This came in the form of REAL (race, ethnicity, and language) data, which Allina Health analysts used to visualize how health outcomes vary by demographic characteristics including race, ethnicity, and language. To understand the root causes of specific disparities as well as to identify solutions within their sphere of influence as a healthcare delivery system, Allina Health consulted the literature and also consulted patients, employees and community members. Then Allina Health created appropriate interventions based on this information.
As a result, Allina Health created an awareness of the health inequities among its patient populations, as well as effective approaches to breach the barriers that were preventing these patients from getting the care they needed. While much work remains in this long journey to achieve health equity, Allina Health has taken some significant steps forward.
According to the Robert Wood Johnson Foundation, “Health equity means that everyone has a fair and just opportunity to be healthier. This requires removing obstacles to health, such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”1
The U.S. ranks last on nearly all measures of equity because of its large income-related differences in health outcomes.2 The most common causes of illness, disability, and death in the U.S.—heart disease, cancer, diabetes, and stroke—are more common and more severe for minority groups.
Health inequities persist in Minnesota as well, despite the efforts of many organizations and programs to improve health.3
Allina Health, a not-for-profit healthcare system with 12 hospitals and 67 clinic sites and ambulatory care centers, is dedicated to the prevention and treatment of illness, and helping people live healthier lives in communities throughout Minnesota and western Wisconsin.
For more than 15 years, Minnesota has tracked disparities in populations of color, American Indians, children, adolescents, immigrants and refugees, and lesbian, gay, bisexual, transgender, and queer (LGBTQ).
In 2011, the state of Minnesota began requiring healthcare providers to collect race, ethnicity, and language (REAL) data. These data revealed inequity. Available literature provided insight into several variables that contribute to these inequities:
Allina Health began stratifying some of its clinical quality outcomes metrics in 2013, revealing opportunities to close the gap amongst some of its racial/ethnic minority patient populations. This stratified data demonstrated that serious health inequities persisted, motivating Allina Health to take targeted actions to reduce inequities.
To be successful in reducing inequities, Allina Health needed to understand the outcomes its patients were experiencing. For this, it needed data. Using the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and a broad suite of analytics applications, Allina Health studied REAL data, and data regarding country of origin, to begin understanding inequities.
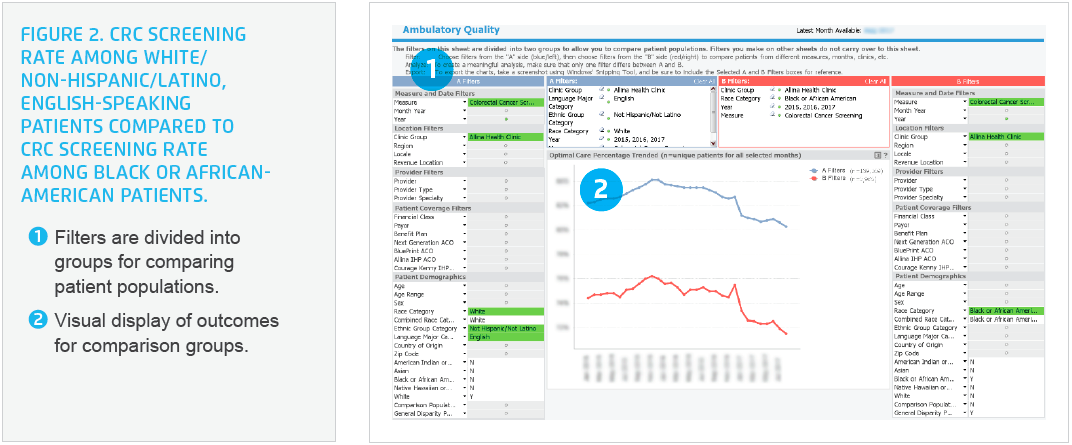
After standardizing data collection, categories of data, and methods used to conduct the analyses, data analysts at Allina Health provided visualizations of health outcomes by race, ethnicity, and language, and displayed the outcomes compared to the white, non-Hispanic/Latino, English-speaking population (see Figure 1).
Analytics revealed that Allina Health had opportunities to reduce health inequities, including improving colorectal cancer screening (CRC) rates. Allina Health developed a multi-level work plan to increase CRC screening rates among speakers of Somali, Hmong, Spanish, Arabic, and Russian languages; as well as Hispanic/Latino, American Indian, African-American, and Native Hawaiian and other Pacific Islander populations. The goal was to achieve a screening rate comparable to the white, non-Hispanic/Latino, English-speaking patients, incrementally closing the gap.
Allina Health recognized that despite having REAL data, its understanding of patients’ needs and perceptions regarding CRC screening was likely incomplete. The REAL data, and data in the EHR, does not include important data regarding other factors that influence health, such as patient values and beliefs about healthcare and specific healthcare interventions, housing stability, financial resource strain, culture, gender identity, food insecurity, social connectedness, and other social determinants of health.

To develop a complete picture and understand root causes contributing to lower CRC screening rates, Allina Health researched available evidence about how to increase screening rates in minority populations, which increased its understanding of barriers, and activities to remedy those barriers.
Allina Health used focus groups with its certified medical interpreters, to gain additional understanding of various patient populations. Allina Health learned about values, beliefs, and barriers that might impede patients from completing the recommended CRC screening:
With improved understanding of the needs of the various patient populations, Allina Health developed and implemented a work plan to improve CRC screening rates, which includes the following interventions:
Allina Health’s data-driven approach to reducing health inequities demonstrated effectiveness through customized interventions. The system increased its understanding of health equity, improved its awareness of where inequities existed, and confirmed an effective approach for reducing them resulting in:
“We’ve learned that there is a difference between equality—where everyone is treated the same—and equity; providing our patients the level of support they need to be successful. By providing additional support to address the barriers, we are able to reduce health inequities.”
– Jana Beckering, RN, Project Manager, Allina Hospitals and Clinics
The integration of demographic filters into all of Allina Health dashboards has enabled the organization to identify opportunities to address health inequities in many areas, including:
The organization will continue to build capacity for the organization to understand the root causes of the inequities and to take action. Allina Health is sharing the learnings from this important work and creating additional organizational capacity to reduce health inequities throughout the organization, integrating health equity data into all its quality improvement efforts.


