Allina Health has three Integrated Health Partnership contracts aimed at financially incentivizing providers for Medicaid patients. With a focus on reducing costs and enhancing patient outcomes, the organization utilizes its analytics platform and PMPM Analyzer to identify cost drivers and develop interventions for improved care and reduced expenses.
Growth in the government payer mix and an increased cost burden to the commercial population, decreases in the private payer population, and programs like the Medicare Shared Services Program, have caused joint ventures, partnerships, and co-branding efforts, better known as at-risk contracts, between payers and providers to increase.
Allina Health has three Integrated Health Partnership (IHP) contracts, an accountable care model that incentivizes healthcare providers to take on more financial accountability for the cost of care for Medicaid patients, which cover approximately 90,000 members. To achieve success in its IHP contracts, and avoid losses, Allina Health needed to reduce healthcare costs while improving patient outcomes and experience.
To identify and analyze opportunities, Allina Health combines several data sources, including claims-based information from the Department of Human Services. Using its analytics platform, Allina Health is able to integrate internal and external data sources to deliver insight into cost drivers and clinical outcomes across the care continuum. The organization also uses a PMPM Analyzer application to complete a comprehensive evaluation of the drivers of per member per month (PMPM) payment performance.
Allina Health has developed the infrastructure required to perform additional opportunity analyses in the future and effectively utilize claims data. Using data and analytics for opportunity analysis has given Allina Health insight into its IHP patient population, supporting the creation of interventions to decrease the total cost of care and improve outcomes.
Driven by the growth in government payer mix and the increased cost burden that the commercial population must pay, decreases in the private payer population, and programs like the Medicare Shared Services Program, joint ventures, partnerships, and cobranding efforts between payers and providers are increasing.1,2 In 2008, Minnesota passed healthcare legislation designed to improve the affordability of healthcare, expand coverage, and improve the health of Minnesotans. This resulted in the development of IHP, an accountable care model that incentivizes healthcare providers to take on more financial accountability for the cost of care for Medicaid patients.2
Healthcare delivery systems which participate in the IHP enter into an arrangement with the Minnesota Department of Human Services and are held accountable for the costs and quality of care their Medicaid patients receive—providers who demonstrate an overall savings (compared to target) receive a portion of the savings, while those who cost more over time may be required to pay back a portion of the losses.2
Allina Health, an integrated delivery system in Minnesota, has three IHP contracts, which cover approximately 90,000 members, half of which live within a three-county metro area. Forty-two percent of the Medicaid members are racial, ethnic, and or language minorities, and 41 percent are less than 18 years old.
Allina Health understands that value-based programs are instrumental in transforming its business. To prosper in its IHP contracts, and avoid losses, the organization needed to reduce healthcare costs while improving patient outcomes and experience.
Prior to developing a plan for reducing costs and improving quality, Allina Health conducted a comprehensive analysis of potential opportunities, ensuring the understanding of its patient population and supporting the development of a strategy and operational plan. While Allina Health previously conducted analyses of IHP patient population opportunities, the analyses were narrow, developed to address a specific problem of interest, performed by an individual analyst, and focused on one IHP program, rather than all covered lives.
To ensure a successful transition to at-risk contracts, Allina Health instituted the proper internal structure to support this shift and brought in the necessary analytics tools that would allow the organization to understand how it was progressing in lowering the total cost of care.
To support effective, data-driven development of a strategy and operational plan, Allina Health implemented a new structure to provide governance, oversight, and continuous improvement of the IHP contracts and patient populations. Allina Health’s infrastructure includes a:
Reducing the total cost of care is impossible without understanding where the opportunity to improve costs and outcomes resides. Allina Health’s IHP programs are supported by robust data, analytics, and subject matter experts enabling effective opportunity analysis.
Allina Health and Health Catalyst professional services combines several data sources necessary to complete the opportunity analysis, including claims-based information from the Department of Human Services. The Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and broad suite of analytics applications, provides the ability to integrate organizational data with external data sources to provide insight into cost drivers and clinical outcomes across the care continuum.
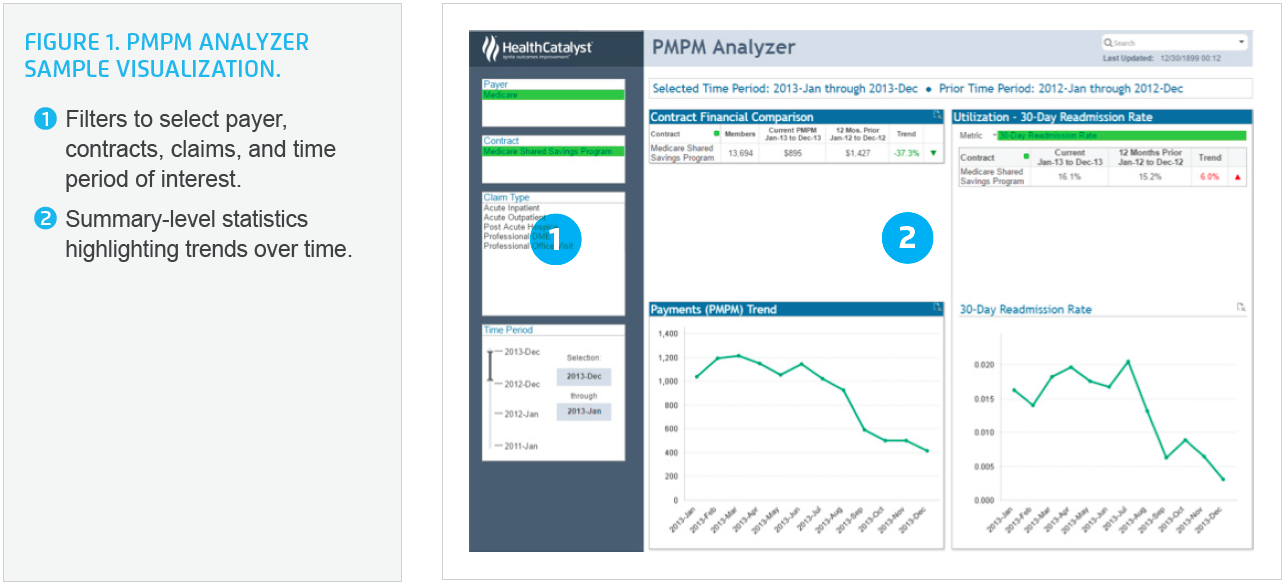
An IHP Cohort Explorer, a case finding tool Health Catalyst professional services built over IHP claims data and reports, and a PMPM Analyzer application are utilized to complete a comprehensive evaluation of the drivers of PMPM payment performance. The claims-based analytic application gives an in- and out-of-network view of payment trends, providing the ability to understand how Allina Health’s ACO procedures, providers, members, and specialty areas are contributing to PMPM payment performance (see Figure 1).
Using PMPM Analyzer, Allina Health can quickly identify top contributors to PMPM performance such as PMPM per 1,000 utilization rates, and network leakage. Areas of high spend, utilization, and variation can be examined, along with factors driving trends. Using the analytics application, teams can explore drivers based on member, provider, and/or claim-based attributes and conduct a detailed analysis of PMPM performance to identify opportunities for improvement.
Using the analytics applications, Allina Health began exploring improvement opportunity within the IHP patient population, starting with an analysis of systemwide claims data to identify the highest cost areas. It then conducted seven additional sub-analyses to drill down into each of the opportunity areas.
When conducting the opportunity analysis, Allina Health focused on clinical areas with high cost and variation, starting with either clinical service lines, or services that cut across multiple departments, such as labs, medications, readmissions, or network leakage, examining risk-adjusted variation by facility and/or provider. Allina Health can drill down to homogenous patient populations by segmenting the patients based on severity, diagnoses, procedures, or a variety of other patient, encounter, or payer attributes.
Allina Health engaged content experts and clinical operational leads to share opportunities and refine the analyses. Once the opportunities are identified, and the analysis is refined to the point of being meaningful, it falls to the Operations Committee to execute the interventions that will improve or maintain outcomes for the targeted patient population while positively impacting the identified cost drivers.
Allina Health’s IHP program uses a robust process for developing interventions, including standardized tools for tracking interventions and related cost drivers. Logic and financial models are used to support program planning and development. An evaluation plan serves as a standard part of measurement planning, and a performance management tool is used for monitoring interventions.
In addition to the opportunity analysis, Allina Health conducts intervention-specific analyses and analysts are actively engaged in the measurement plan. Prior to implementing new interventions, Allina Health identifies what it needs to know, what the questions are, and how the questions could be answered. Analysts are engaged to determine how the data can best be captured and the source.
Operations leaders, data analysts, and key stakeholders work together to develop a driver diagram, creating a visual display to illustrate the relationship between the overall goal of the project, the primary drivers or opportunity areas contributing to the goal, and the specific tactics and interventions required to achieve the goal (see Figure 2).

Allina Health uses data from the EHR and analytics applications to provide monthly reports on leading measures and analytics for quarterly reports focused on lagging measures. These quarterly reports include an executive summary, performance reports, trended data, care coordination data, and driver diagrams, providing visualization of program interventions and the impact on patient outcomes and cost drivers.
Using data and analytics for opportunity analysis has provided Allina Health new insight into its IHP patient population, supporting the development of interventions to decrease the total cost of care and improve outcomes. Allina Health has achieved the following:
“Rather than focusing on a specific intervention, or a narrow clinical question, we started with the claims and electronic health record data to tell us our population health opportunities.”
– Melissa Hutchison, MPH, Manager, Program Strategy, Value and Analytics
Allina Health and its IHP programs continue to build out interventions and measurement plans. The infrastructure (Strategy, Operations, & Analytics Committees) has since been expanded to focus on all Allina Health value based contracts (including Medicaid, Medicare, and commercial).




