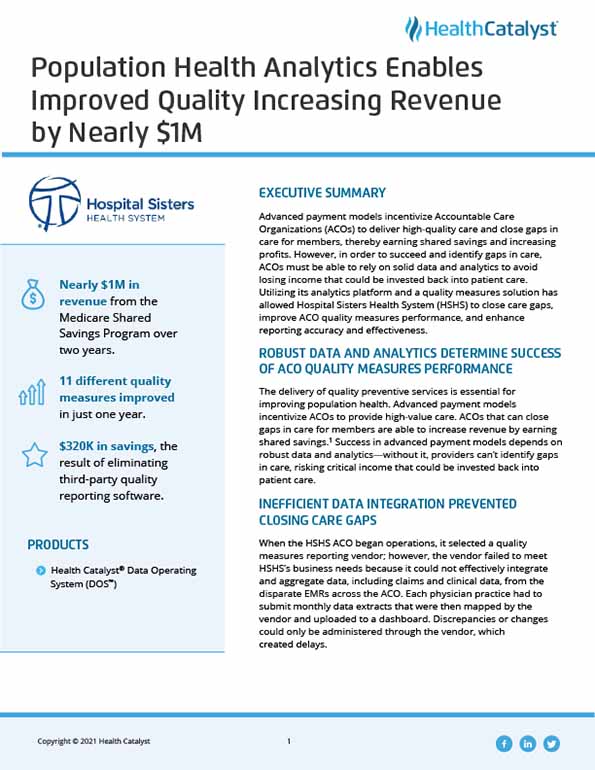
Advanced payment models incentivize Accountable Care Organizations (ACOs) to deliver high-quality care and close gaps in care for members, thereby earning shared savings and increasing profits. However, in order to succeed and identify gaps in care, ACOs must be able to rely on solid data and analytics to avoid losing income that could be invested back into patient care. Utilizing its analytics platform and a quality measures solution has allowed Hospital Sisters Health System (HSHS) to close care gaps, improve ACO quality measures performance, and enhance reporting accuracy and effectiveness.
The delivery of quality preventive services is essential for improving population health. Advanced payment models incentivize ACOs to provide high-value care. ACOs that can close gaps in care for members are able to increase revenue by earning shared savings.1 Success in advanced payment models depends on robust data and analytics—without it, providers can’t identify gaps in care, risking critical income that could be invested back into patient care.
When the HSHS ACO began operations, it selected a quality measures reporting vendor; however, the vendor failed to meet HSHS’s business needs because it could not effectively integrate and aggregate data, including claims and clinical data, from the disparate EMRs across the ACO. Each physician practice had to submit monthly data extracts that were then mapped by the vendor and uploaded to a dashboard. Discrepancies or changes could only be administered through the vendor, which created delays.
Inefficient, inconsistent, and inaccurate reporting made it virtually impossible to generate real-time, actionable insights that could be used to close care gaps and improve performance. HSHS needed an ACO quality measures solution that supported its practices in delivering best-practice preventive, primary, and specialty care while ensuring real-time reporting, effective care-gap closure, and quality improvement.
HSHS leveraged the Health Catalyst® Data Operating System (DOS™) platform and a robust suite of analytics applications, including a quality measures solution, to establish a single source of truth across its disparate systems. The quality measures solution allows HSHS to track and visualize care gaps at an individual patient level and generate realtime, actionable quality measures reporting.
HSHS uses the quality measures solution to help practices and providers identify patients’ current and rising needs, schedule outreach to specific patients for follow-up, coordinate care across sites and providers, and quickly determine screening, monitoring, and therapies needed for care-gap closure.
For the first time, practices and providers have access to the detailed data required for effectively closing gaps in care, ensuring patients receive the primary and preventive care they need. Practices use the data in the quality measures solution for pre-visit planning. Practices can also identify the specific measures for which each patient qualifies, allowing providers to quickly and easily determine if the patient has received all necessary care. Providers no longer waste their valuable time digging through the EMR to locate critical patient data. Instead, providers can focus on addressing each patient’s unique care needs, improving the effectiveness of the time they spend with the patient.
In addition to visualizing practice- and patient-specific data, HSHS can analyze and visualize data for the entire ACO and gain valuable insight into performance. It is able to use DOS and the quality measures solution for electronic clinical quality measures reporting. Leadership can quickly and easily monitor performance, allowing them to identify areas where the ACO is on track to achieve the desired quality targets and opportunities for improvement. The ACO uses the quality measures solution to select priorities for improvement and to guide the deployment of resources and development of programs to help the practices improve.
HSHS supports high-performing practices in sharing workflows and best practices while also accelerating learning and care-gap closure across the ACO.
HSHS used DOS and the quality measures solution to close care gaps, improve ACO quality measures performance, and enhance reporting accuracy and effectiveness. Results include:
"We’ve had great success using the Health Catalyst quality measures solution to integrate and analyze disparate data across our network. We now have the data and analytics required to calculate performance accurately. We’ve improved reporting of performance and given the practices the detailed data required for improvement. The practices have closed care gaps for tens of thousands of patients, and increased revenue by nearly $1M."
- Tricia Hannig, RN, BSN, Director of Quality Improvement, Physician Clinical Integration Network, HSHS ACO
HSHS will continue to use a data-driven approach for closing care gaps and reporting quality measures while seeking additional opportunities to improve the information shared with its providers and support them in delivering high-quality care to patients.