Health system mergers can promise significant savings for participating organizations. Research, however, indicates as much as a tenfold gap between expectation and reality, with systems looking for a savings of 15 percent but more likely to realize savings around 1.5 percent.
Driving the merger expectation-reality disparity is a complex process that, without diligent preparation and strategy, makes it difficult for organizations to fully leverage cost synergies. With the right framework, however, health systems can achieve the process management, data sharing, and governance structure to align leadership, clinicians, and all stakeholders around merger goals.
 Download
Download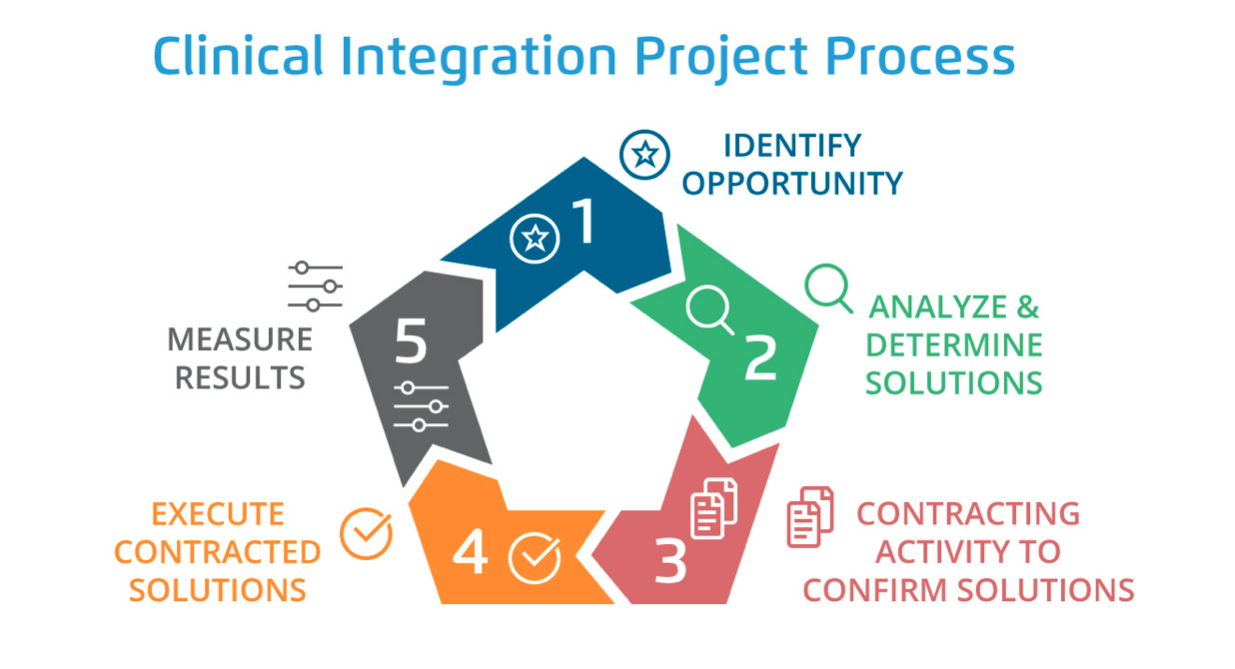
This report is based on a 2019 Healthcare Analytics Summit presentation given by Hani Elias, JD, MPH, Chief Executive Officer, Lumere, and Amy Whitaker, RN, BSN, Vice President, Supply Chain Clinical Integration Accountability, Bon Secours Mercy Health, titled, “Expediting Mergers & Acquisitions: The Role of Data and Clinical Evidence.”
Health system mergers and acquisitions promise appealing benefits, including eliminating inefficiencies and the competitive advantage of scale. However, successfully navigating the merger process for optimal gains is complex, and research shows that organizations often fail to fully leverage cost synergies.
For example, while executives may expect a supply chain cost savings of 15 percent (e.g., $1.7 million) with a merger, the average savings realized is far lower at 1.5 percent (e.g., $176,000)—a tenfold gap between expectation and reality. Part of the challenge is that federal, state, and internal regulations may prevent two legacy systems from accessing each other’s data before the merger, compounded by possible distinct standards, governance structures, IT infrastructure, and cultures between the two systems.
Though healthcare mergers may not yield the big gains once forecasted, organizations can still benefit with a merger strategy that supports sophisticated process management, data sharing, and a governance structure that aligns leadership, clinicians, and all stakeholders. With the right framework and preparation, mergers can achieve goals rapidly by jointly leveraging clinical evidence and analytics to accelerate benefits.
With the right organizational framework, legacy systems can quickly scale and align value analysis and vendor management capabilities to achieve desired supply chain efficiency and scale. Pre-merger, the executive steering committee (comprised of the CFOs and other members of executive leadership) uses high-level data analysis to identify its supply chain goal (e.g., 10 percent savings target for supply chain costs).
A four-pillar framework will help the merger achieve its stated goal:
Review both legacy systems’ partnerships to identify commonalities, redundancies, and opportunities.
Establish effective process for the legacy systems to reach goals together and align communication to ensure both entities are working towards same goal. Identify which organizational level to make process decisions (e.g., the facility, system, or market level).
Establish the culture—such as determining a collaborative/interdisciplinary model versus a more siloed approach. Review the current teams’ skillset and establish accountability for talks post-merger.
Consider post-merger technology challenges (e.g., are both legacy systems on the same enterprise resource planning software?). To ensure clinical integration, data from disparate software and platforms will need to be translated into a common language.
After establishing the four pillars for a successful merger, the next step is applying evidence and analytics to achieve to following milestones:
Legacy systems may have to plan their merger without seeing one another’s specific data. In this case, an analytics partner can create a “black box,” in which blinded information from both systems can be stored and analyzed pre-merger. As soon as the merger takes place, the analytics partner can share findings and recommendations to immediately start realizing savings goals.
By establishing the four pillars for a merger and applying evidence and analytics, organizations prepare a pipeline that allows them to move forward with supply chain clinical integration as soon as the merger is complete, taking action for instant wins.
Organizations can follow four steps to implement supply chain clinical integration:
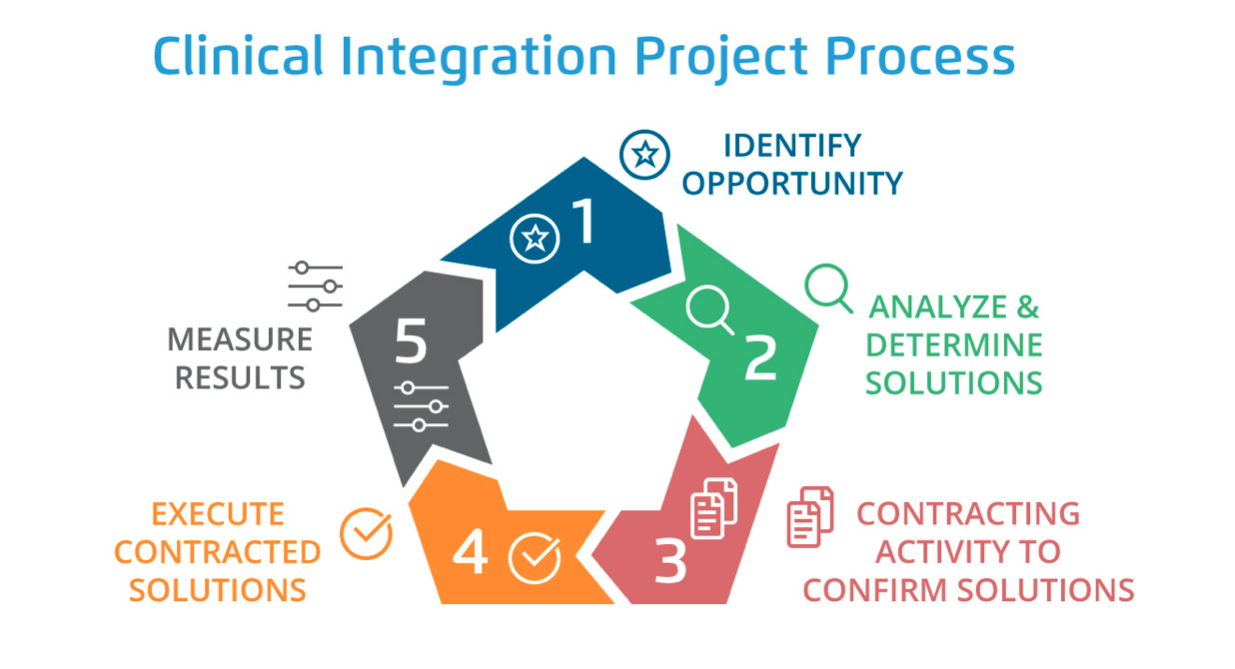
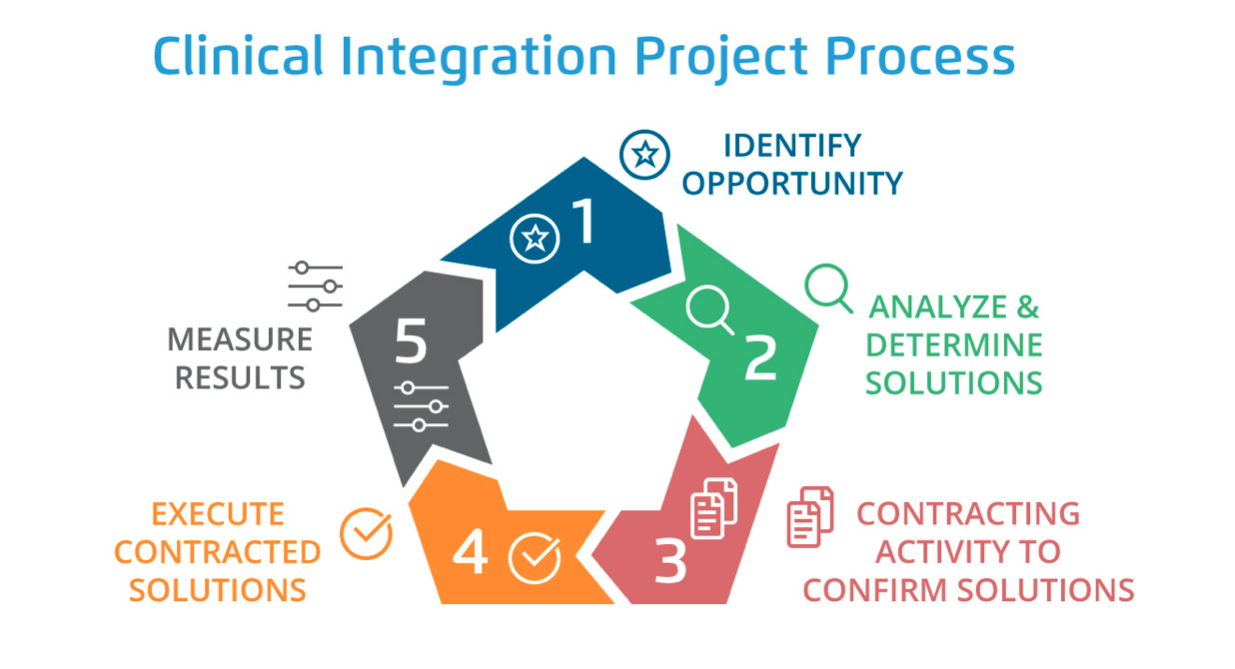
Following the four steps above, the clinical integration process takes place in five phases: identifying opportunity; analyzing and determining solutions; contracting activity to confirm solutions; executing contracted solutions; and measuring results (Figure 1).
A successful clinical integration process has positive impacts both financially/operationally and clinically:
As referenced earlier, mergers seldomly deliver the level of savings they might promise. Their greater benefit may be the opportunity to rethink and improve operations of both organizations while also achieving realistic savings with a robust evidence- and analytics-driven clinical integration process. By building a pre-merger framework and engaging clinicians and empowering them with data to make the best decisions, post-merger organizations can optimally prepare to deliver improved outcomes while saving costs.
Would you like to learn more about this topic? Here are some articles we suggest:
The Top Three 2020 Healthcare Trends and How to Prepare
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.