Drs. Allen Frankel and Michael Leonard have developed a framework for creating high-reliability organizations in healthcare. This report, based on their 2018 webinar, covers the components and factors of this frame work, including:
• Leadership
• Transparency
• Reliability
• Improvement and Measurement
• Continuous Learning
• Negotiation
• Teamwork and Communication
• Accountability
• Psychological Safety
 Download
Download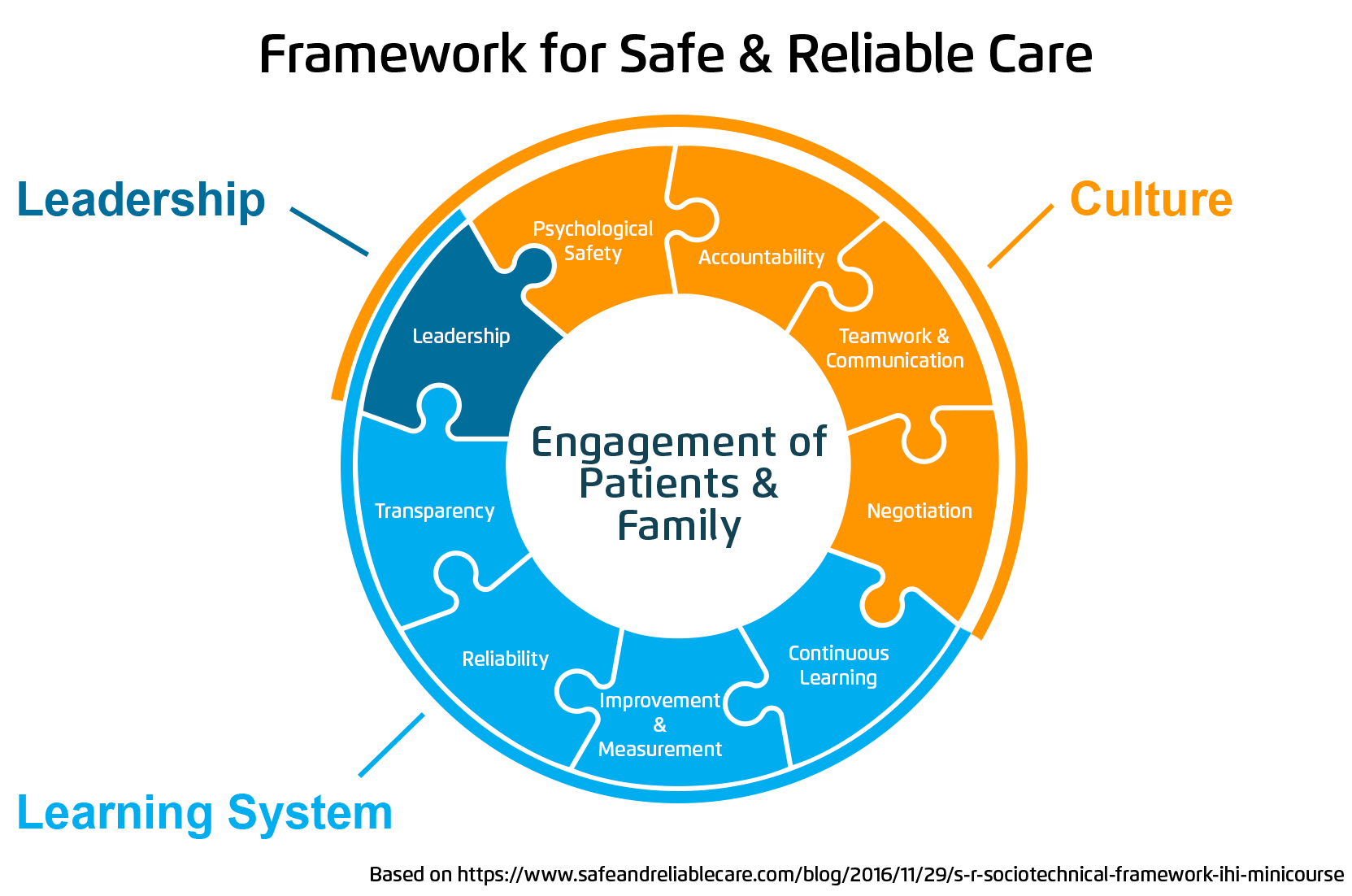
This report is based on a 2018 webinar presentation given by Allan Frankel, MD, Founding Partner, Safe & Reliable Healthcare and Senior Faculty, Institute for Healthcare Improvement; and Michael Leonard, MD, Managing Partner, Safe & Reliable Healthcare and Adjunct Professor of Medicine, Duke University School of Medicine. entitled, “A Systematic Framework for the Delivery of Safety, Highly Reliable Care and Habitual Excellence.”
Despite a growing focus on quality improvement in healthcare, the skills needed to make measurable, sustainable improvements in care are not inherent, even among dedicated, smart healthcare professionals, because those skills were not baked into their DNA from medical school through residency through practice as many other skills were. But as anyone in healthcare knows, quality improvement is an essential piece of organizational evolution and development. Patients and their families are at the center of everything healthcare providers do. They entrust their lives and wellbeing with their providers, and that is a sacred trust.
To address the need for quality improvement skills, Drs. Allen Frankel and Michael Leonard, both experts with more than 23 years of experience across more than 1,300 hospitals, created a practical, systematic framework that can be applied in virtually any care setting, from neurosurgical ICU to office practices to pharmacies to home care organizations. Drs. Frankel and Leonard published a white paper in 2017 entitled “A Framework for Safe, Reliable, and Effective Care” with the Institute for Healthcare Improvement (IHI) that delves deep into this framework.
In addition to developing the framework, Drs. Frankel and Leonard have put together the key components of High Reliability Organizations (HROs), including leadership, a safety-focused culture, and a dedication to continuous learning and improvement, and they offer practical tools and insights that enhance the ability to deliver optimal patient care in an environment focused on learning and quality improvement.
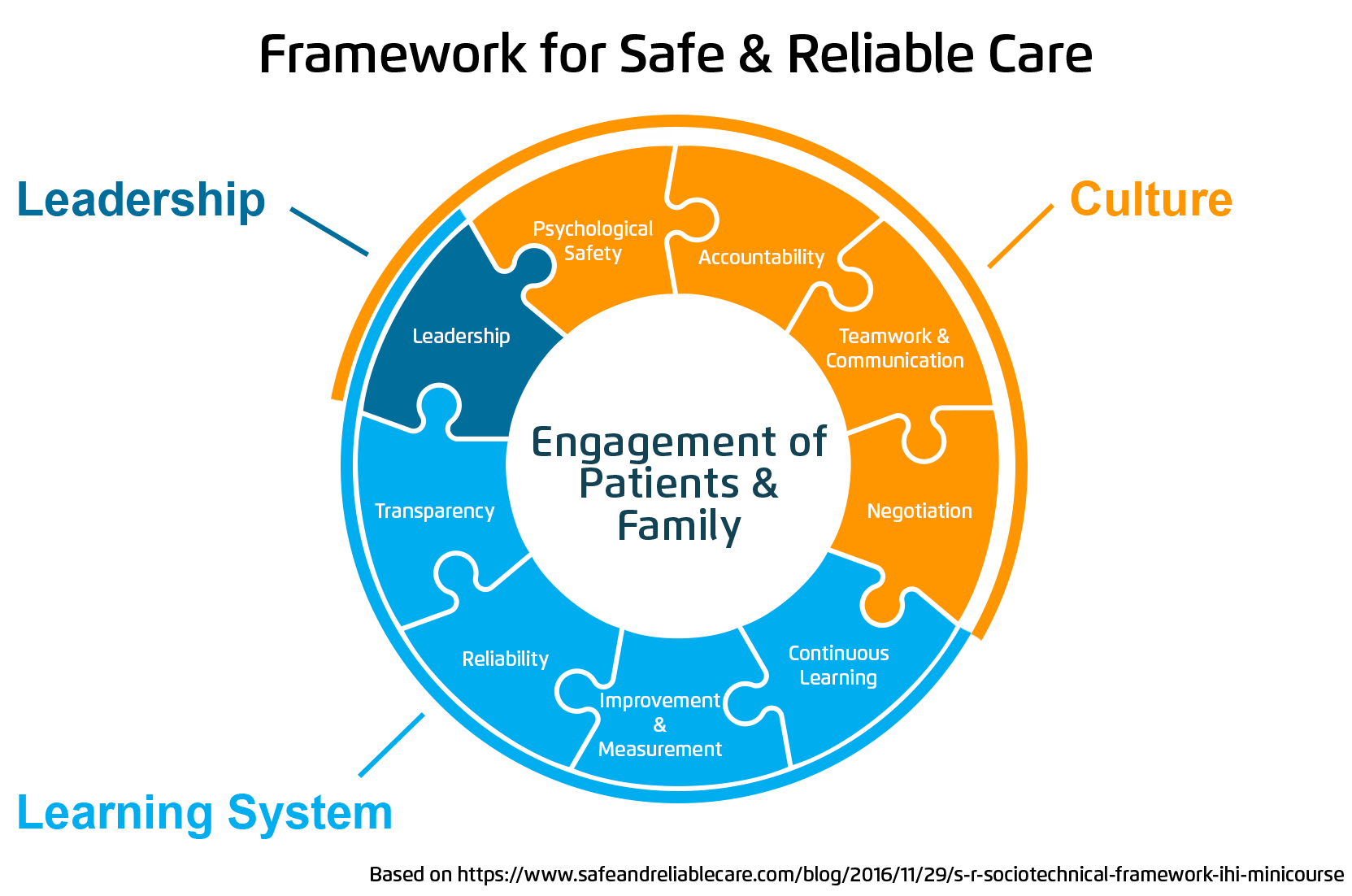
The necessary pieces for developing and sustaining a culture and system that delivers safe, highly reliable care are strong effective leadership, a culture of safety, and an accessible learning system. Figure 1 shows the components of that framework and how each aspect fits into three categories: leadership, culture, and learning system.
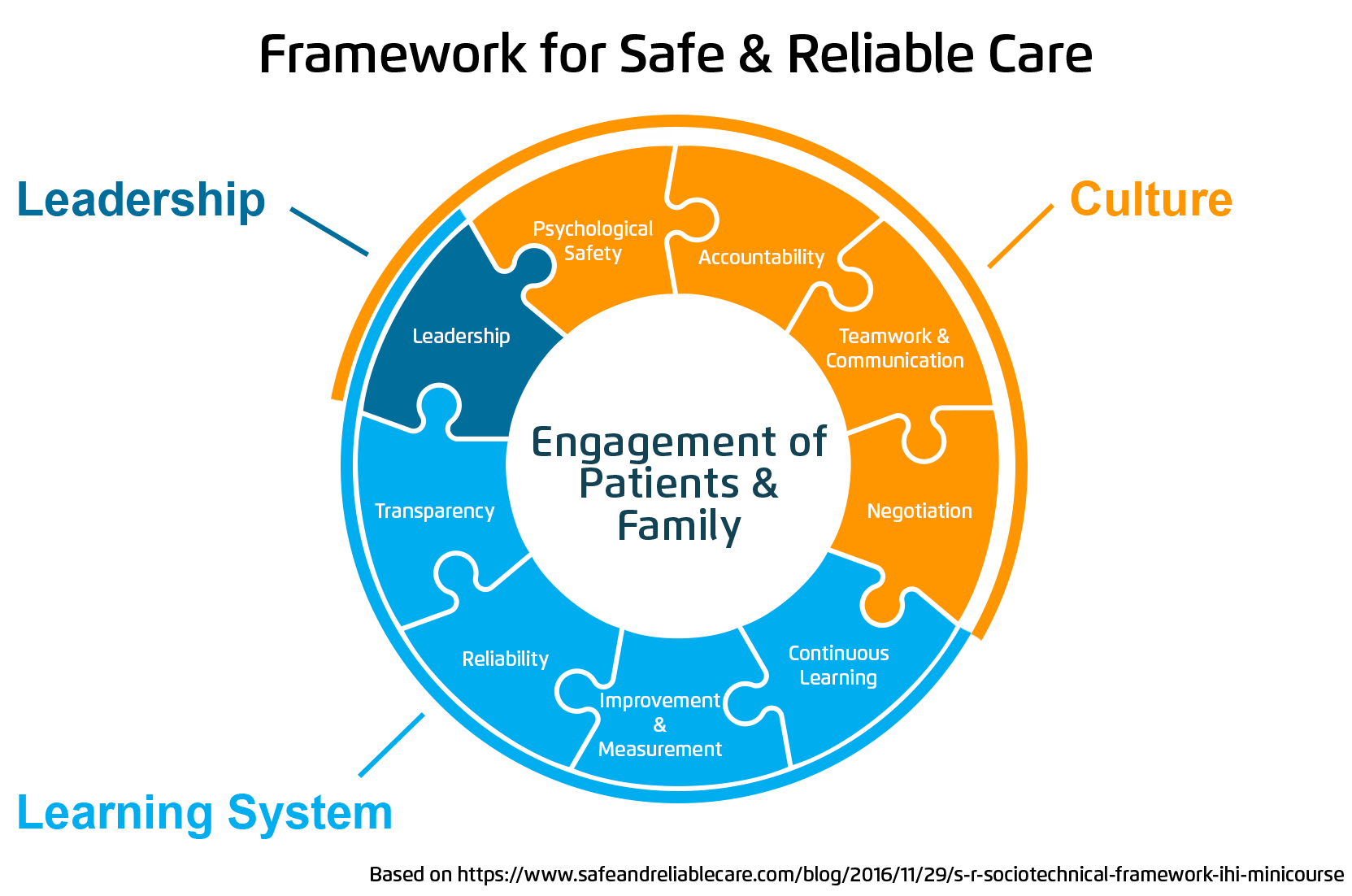
The framework provides a clear roadmap to move forward and do the work of developing an organization focused on patient safety. What Drs. Frankel and Leonard have learned through their decades in patient safety is that all aspects of the framework must exist, or learning won’t be sustainable. Improvement won’t be sustainable. The cultural maturity model helps illustrate the type of culture that is necessary to move forward toward becoming an HRO.
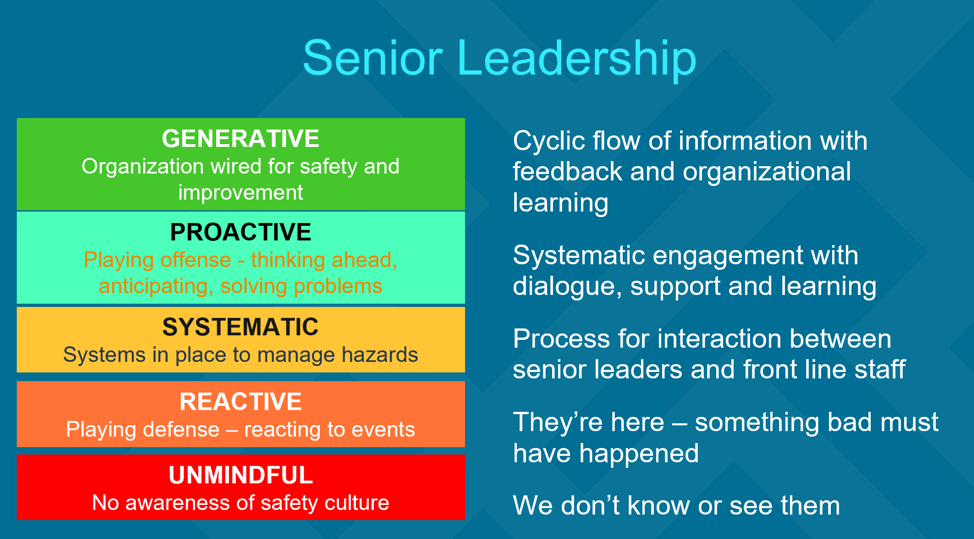
The concept of a cultural maturity model has been around since around 1975 and since its development, it has evolved to help organizations think about how they can from an unmindful culture to one that is generative. Within healthcare, all components of the framework, from leadership to learning, can be rated on a cultural maturity scale, as seen in Figure 2.

Historically, nurses and doctors have been trained and evaluated using the individual expert model. The idea behind that model is that if expert healthcare professionals are put in any healthcare environment, they’ll figure it out. The problem is that doesn’t work. Healthcare today is too complex to do that successfully across the board. The best, most effective solution to quality improvement is to work collaboratively and proactively. As Figure 2 shows, the tipping point for psychological safety is when an organization goes from a systematic model of managing hazards to a proactive one in which staff anticipates and prevents problems before they occur. The pinnacle of cultural maturity is a generative culture in which safety is the culture. It’s how business is done. It’s constantly vigilant and transparent.
Reactive cultures are like playing defense. They react to problems rather than trying to foresee them and get ahead of them before they become catastrophic. When people within an organization are simply reacting, they tend to make mistakes. They’re distracted, they need to multitask, and they forget things. And, much like distracted driving, distracted caregiving can have unintended negative consequences.
Being proactive and generative doesn’t come naturally, and in today’s health systems, it’s not yet the norm. Drs. Frankel and Leonard and their team assessed 30 community hospitals for the state of Massachusetts to help figure out how these organizations could sustain high-quality community care within an ever-changing environment full of systems mergers and political changes. They found that only four out of the 30 hospitals were proactive to generative, and the overwhelming majority were reactive.
They also found that even within the reactive cultures there were pockets of proactive units – departments within the hospitals that were getting it right some of the time. And what they learned about those departments was that they worked collaboratively. They didn’t do it all the time, but it was a start, a foundation.
The ability to come together, think ahead, and play as a team is critical for the ability to deliver safe care. Novices on the team can turn to the experts for valuable information, and thus learn how to deliver excellent care, eventually becoming experts themselves. It creates a huge library of experience for the entire team to draw from that will create predictability. One of the most basic concepts of high reliability is anything that can be made predictable should be made predictable. This helps avoid surprises. And avoiding surprises helps improve cultural maturity.
HROs thrive because their leadership takes charge of the culture, engages staff, promotes a culture of safety, and embeds continuous learning and improvement processes into the everyday lives of everyone within the organization. Effective leadership is the primary component of an HRO.
An organization with a proactive or generative culture must have effective leadership, both at the senior and local level, aligned with the goals of the organization. Strong, effective leaders of HROs are engaged and knowledgeable in several aspects of organizational and system management, such as organizational development, whole system change, and measurement to manage. They must also have a relentless focus on process and know that culture is a process, not a destination.
A culture of safety starts at the very top with senior leadership. An organization is only as strong as its leaders, so having leaders guiding the culture is important. Figure 3 below provides examples of how leaders are engaged in the different levels of cultural maturity. In an unmindful culture, the staff doesn’t know who the leaders are. The leaders are absent, and they aren’t engaging with the doctors and nurses on the ground providing patient care. Moving up the scale from unmindful to generative, the leaders are more and more engaged. Leaders in proactive and generative cultures are present. They’re talking with staff. They listen, support, and learn. And in the best cultures, they make space for a cyclic flow of information that encourages feedback and cross-organizational learning.
Next in the top-down culture of safety is local leadership. In unmindful organizations, local leadership is mostly absent, but in proactive and generative organizations, local leaders model the behaviors that drive a culture of safety and create an atmosphere that provides for psychological safety and accountability. They play offense, think ahead, and wire the whole organization for safety and quality improvement.

There is plenty of data about the effects of leadership on overall culture and staff engagement. One example is a survey of staff at 30 Michigan hospitals. The data collected shows the importance of leaders being present and listening to the frontline staff and how their presence and engagement can have significant positive effects on culture, safety, and burnout.
Drs. Frankel and Leonard published a study in 2017 about cultural data that surveyed and collected data from 17,000 people across 30 hospitals in Michigan. The survey looked at seven specific areas.
At the beginning of the survey, there were two questions. The first was: “Do your leaders participate in walk-arounds in your organization?” Ten thousand of 17,000 people said yes. The second question was: “Did you get feedback on the issues you raised?” And 4,500 said yes, and 5,500 said no.
Figure 5 illustrates the effect of leadership not only asking for feedback, but actually acting on it, closing the loop, so to speak, of ideas and concerns brought up by staff on the frontline of patient care. The graph in Figure 5 represents the seven areas surveyed. The red bar represents scores when leadership did not close the loop. The green bar represents scores when leadership did close the loop. And the blue bar represents the mean.
The takeaway here is that providing feedback after leadership walk-arounds is associated with better patient safety culture, higher employee engagement, and lower burnout. The scores for people who felt listened to and heard are dramatically higher than those who didn’t.
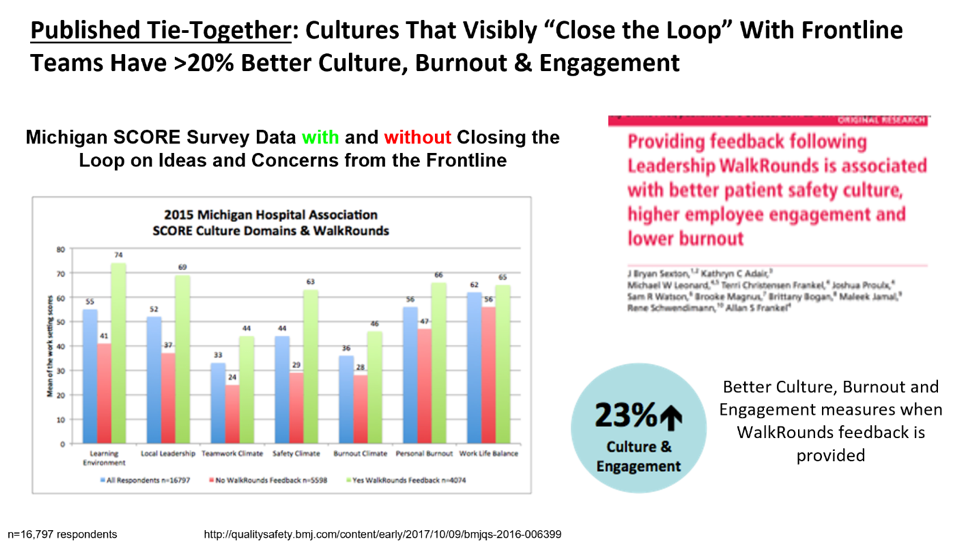
For statistical significance, there must be a five to seven-point difference in scores. In this survey, the difference is more than 30 points in some cases, and in all cases, it’s at least nine points.
Another component of HROs is a culture of safety. Patient safety is an important part of that culture, but it’s more of a result and a goal than a defining part of the culture. A culture of safety must address burnout and encourage different aspects of safety.
Burnout in healthcare can lead to many negative effects, including errors, infections, higher mortality, and decreased patient satisfaction. It can also lead to high turnover, which can have a significant effect on the bottom line.
The opposite of burnout is resilience. And a culture of safety tends to have low burnout rates and encourage resilience. Going back to the cultural maturity model, resilience goes up and burnout goes down as the culture becomes more proactive and generative.
There are several factors that encourage resilience and decrease burnout. Each factor revolves around the employee being heard and supported:
Safe, optimal care requires psychological safety and feeling safe and empowered to speak up. When frontline care providers don’t feel safe and empowered, they may not feel comfortable speaking up if they notice something that isn’t quite right. Wrong site surgeries and retained foreign bodies are two medical errors that are too common in healthcare, and they are entirely preventable. Studies show that when OR staff feels safe and empowered, there are fewer surgical never events like these.
Accountability is another significant aspect in a culture of safety. The framework stresses differentiating between individual issues and systems issues when holding individuals accountable. It’s also important to create a work environment that is perceived to be both just and fair.
A culture of safety requires teamwork and effective communication. Much like psychological safety, successful teamwork is correlated with improved patient safety. Going back to the cultural maturity scale, a generative culture values teamwork and continuous learning. These things are deeply embedded in the culture, and teamwork is taught and modeled across the organization.
There are four tenets of effective teamwork.
The last tenet of effective teamwork, resolving conflict, leads into the next aspect of a culture of safety: negotiation.
Conflict is unavoidable. Whenever there are more than two people involved in an organization, there will be conflict. But conflict does not have to be negative or degenerative. With collaboration and negotiation, conflict can be addressed effectively, thus encouraging a more robust culture of safety.
Negotiation should involve collaborative forms of negotiation. No one negotiates in a vacuum. It should also differentiate position from interests, and it should use appreciative inquiry.
The four concepts that must be addressed to develop and nurture a culture of safety, psychological safety, accountability, teamwork and communication, and negotiation, all work together to create teams that work – for each other and for the patients. All healthcare organizations must also address burnout. If leadership focuses on these things and makes them central parts of the culture, they are well on their way to becoming an HRO.
Another vital component of an HRO is continuous learning. HROs have one thing in common when it comes to learning: a visible and transparent learning system. An effective learning system must be transparent. It must be reliable. It must focus on continuous learning. And it must provide for improvement and measurement in order to learn and grow.
A learning system, when well developed and rolled out, can have measurable positive effects throughout the organization.
For example, Drs. Frankel and Leonard have spent about 25 years running interventions at hospitals and health systems. One of their significant interventions started at Mayo Clinic. After working to integrate the framework into their organization, including a transparent learning system, Mayo now has local leadership, local managers, and power workers who give staff a voice and make them feel cared about. From there, they can successfully layer on the improvement process.
About 18 months into the work with Mayo, one senior surgeon talked to Dr. Frankel about the transformation he saw throughout the organization. He said, “Before we started this program, my biggest concern when I went home in the evening was that I didn’t know what I didn’t know. In other words, nurses weren’t comfortable coming and talking to me about the issues they were running into with the patients on the unit. Now that nurses and staff are comfortable about speaking up about their concerns, I know what I need to know to help the services run smoothly and safely. I go home in the evening with great assurance that we are on track.”
What’s notable and important about this comment is that it’s illustrative of the idea that when people are comfortable speaking to each other, it can be an essential piece of creating operational excellence and delivering safe, reliable care.
Similar results can be seen at other organizations when the three components of the framework are in place: culture, leadership, and a learning system. Leadership is the key component. Without effective, engaged leadership that supports a generative culture, it becomes difficult to have holistic change. Local leadership must work hand in hand with senior leadership to create a culture where psychological safety is manifest, where people feel like they’ll be held accountable fairly, and where the team behaviors, like briefings and debriefings, are robust regardless of care setting.
Ultimately, Drs. Frankel and Leonard have seen true change is possible, that cultural maturity can happen if teams and units and organizations are both self-reflecting and improvement-capable. The culture must be robust enough that self-reflection becomes part of that culture, and they have to have enough improvement capacity that they can look at weaknesses and cracks and act on them in an effective, cultural healthy way that focuses on overall safety.
Getting to that point takes more than people and processes. It also takes tools that can take the components of HROs from theories to action.
In addition to the framework, Drs. Frankel and Leonard have developed practical tools that enhance the ability to deliver optimal patient care in an environment of continuous learning. The most effective tool is a real-time learning board. These learning boards have several benefits.
A well-designed learning board encourages a culture of safety in key ways:
Through their years of experience, Drs. Frankel and Leonard have found that doing this work and creating a culture of safety is critical. It provides a framework to integrate all initiatives and a foundation to successfully carry them out. It also gives a clear focus on culture, and a proactive, generative culture is essential to creating sustainable value and providing world class care. Culture is the social glue. It reflects the attitudes and behaviors of the people delivering care. So, a generative culture enhances patient care – and care for the caregivers, the frontline personnel–which can go a long way to addressing burnout and increasing psychological safety.
Figure 6 shows how the components of HROs all come together into the Framework for Clinical and Operational Excellence.

With this framework in place and patients and their family always at the center of care, it is possible to become an organization that delivers safe, highly reliable care across the board. But to do this successfully and sustain improvement, all pieces of the puzzle must be in place. A culture change starts at the top with strong, engaged, system-wide leadership that encourages a culture of safety and pursues continuous improvement by implementing a transparent, robust learning system. And to get there, organizations must be open to feedback and must have avenues of measuring improvement.
Drs. Frankel and Leonard, along with their team at Safe & Reliable Healthcare, have been working on this process at more than 1,300 hospitals for more than two decades. Much like cultures at HROs, their process has evolved and matured. It’s a process that works. And it’s a process that leads to significant changes that can have real, positive, measurable effects on patient care and patient safety. When organizations follow the framework for the delivery of safe, reliable care, staff benefits. Frontline providers benefit. The organization benefits. Patients benefit. And that is worth the investment every time.
Would you like to learn more about this topic? Here are some articles we suggest:
Would you like to use or share these concepts? Download this presentation highlighting the key main points.