Continuity of Care Documents: Today’s Top Solution for Healthcare Interoperability Demands
ACOs, clinically integrated networks (CINs), and those seeking to increase exposure to value-based payment (VBP) models and take on risk need more data interoperability to achieve desired outcomes. Organizations that continue to rely solely on claims data to drive quality improvement may lack more than 80 percent of available critical patient information.
This article considers health data’s current interoperability limitations and why using only claims and acute clinical data can’t close quality gaps. It poses using ambulatory clinical data in the form of continuity of care documents (CCDs) as today’s best interoperability solution.
Quality Measurement Today Demands a New Data Standard
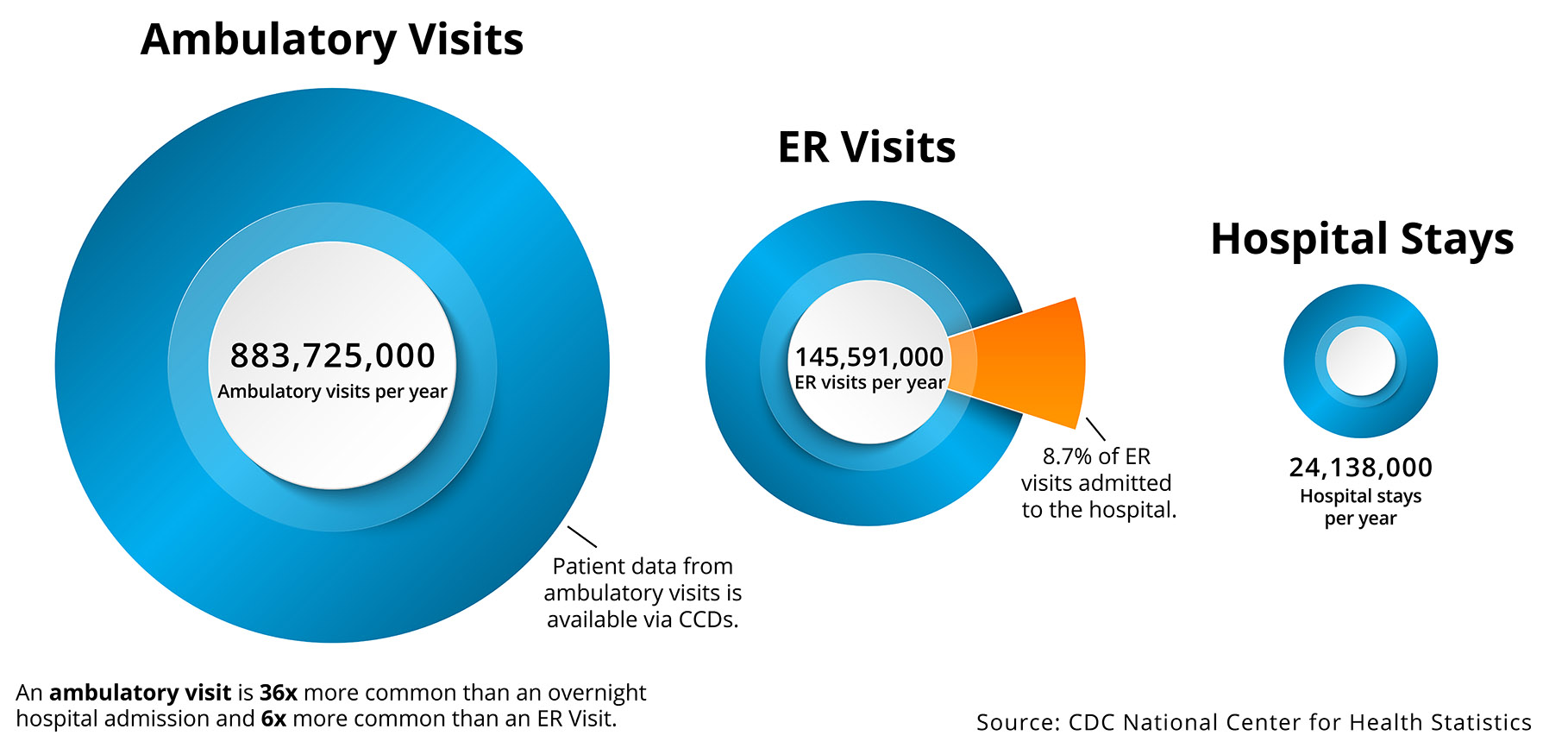
Because healthcare consumers today are much more likely to receive care in an ambulatory setting versus the acute care setting (which claims data represents), organizations must have the interoperability to access ambulatory data.
Data interoperability drives insights behind and takes steps towards significant quality improvements, including the following:
- Project quality performance.
- Perform quality initiatives (e.g., reduce readmissions).
- Accurately stratify patients according to risk.
- Prioritize patients who will benefit the most from prompt care.
- Track clinical performance in near real time (versus retrospective claims data).
With a variety of healthcare delivery settings, it’s important to understand some of the key limitations and differences, including identifying where most of the valuable clinical data resides (Figure 1).
Health systems have used claims data to inform quality measurement and calculate required metrics, but as the industry evolves further towards population health and value-based care (VBC), organizations need more timely, comprehensive, and higher quality data. CCDs, which contain patient-centric clinical data, are not an ideal solution, but as the industry finalizes interoperability standards and removes the hurdles to sharing data, CCDs are today’s most capable and broadly adopted healthcare clinical data source.
Organizations that overlook CCDs and wait for a more comprehensive data solution (i.e., FHIR) will miss out on years of improvement opportunities and fall behind industry benchmarks, as they’ll rely on delayed or incomplete data:
- Claims data is often delayed or incomplete. Claims can provide retrospective analysis of financial and operational performance but is too delayed or incomplete to support near real-time evaluation of implemented interventions. Claims processing can be delayed up to 90 days or more, lack clinically relevant data (e.g., blood pressure, body mass index, and lab result), and provide an incomplete data set for evaluating clinically driven quality measures (QMs), custom measures, and identifying gaps in care.
- Clinical data is the best current solution. CCD data quality can vary based on the contributing source system; however, it can be available near real-time, providing timely operational and clinical insights. And though CCDs alone lack the ability with complete fidelity to effectively monitor key operational and financial metrics in value-based contracts, they can provide leading indicators that performance is trending in the right, or wrong, direction before claims are processed, adding the key capabilities:
- Delivering directional metrics in real-time (e.g., patients seen or not seen by primary care a provider within seven days of hospital discharge).
- Blending into a patient centered longitudinal clinical record.
- Sharing with any Meaningful Use Stage 2 compliant system to support transitions of care.
While Healthcare Waits for FHIR, A Data Solution for Today
The 21st Century Cures Act sets the stage for FHIR, however, it is several years away, and many EMRs do not currently offer an effective way to ETL (extract, transform, and load) data. FHIR is likely the preferred method of the future, but its standards were out for commentary until May 2019 and not expected for release until the fall of 2019. The release date for the latest and fourth version of FHIR also has one- to two-year grace period, meaning it may not happen until 2021 or 2022. While healthcare waits for FHIR, CCDs may be the best available solution to interoperability.
By providing a standard way to document and transmit clinical data, CCDs provide interoperability between multiple acute and ambulatory providers, pairing retrospective analytics (e.g., claims) and robust near real-time clinical analytics. Interoperability is increasingly critical as QMs require certain data that often only resides in ambulatory clinical records:
- Medications.
- Problems/complications (e.g., high blood pressure).
- History of procedures.
- Lab results.
- Social History.
- Vitals.
- Encounters.
- Immunizations.
- Care plan.
Three Guidelines to Help Organizations Best Leverage the Interoperability of Continuity of Care Documents for QMs
The following guidelines help healthcare organizations best leverage CCD interoperability for QMs:
1. Maximize the Value of Clinical Data with an Organizational Data Quality Program
An organizational data quality program drives success for quality measures and alignment to other strategic objectives:
- Perform CCD coding analysis.
- Parse, map, stack and normalize coded values.
- Translate into standard terminology.
- De-duplicate across sources.
- Align coded data to strategic objectives and defined metrics.
- Evaluate level of value the new data content has for strategic objectives and KPIs.
- Continuously seek improvement in data quality and alignment to goals.
2. Measure Clinical Data Quality and Identify Supportive Technology for QMs
The following strategies support an effective approach for QMs:
- Harmonizing quality measure data capture.
- Exploring the use of APIs and shared platforms to aggregate information.
- Evaluating data quality and measurement with pre-submission validation testing tools.
- Determining options for new data capture within workflows to support QMs.
- Identifying common workflows that support QMs.
- Exploring vendor options to report on all QMs appropriate to the client base.
Interoperability Requires a Robust Analytic Platform
Interoperability to capture ambulatory clinical data from CCDs is an essential part of improving outcomes, but healthcare still involves a diverse set of public and private data collection systems (e.g., CCDs, surveys, enrollment, and claims data). Driving better outcomes starts with blending more data together, particularly two data types—near real-time CCDs and retrospective claims.
To meet healthcare’s modern goals, organizations must leverage a fully interoperable analytics platform to acquire near real-time clinical data and harmonize it with a range of data types from a variety of sources. An optimal modern healthcare data approach includes use of a cloud-based analytics platform, such as the Health Catalyst® Data Operating System (DOS™).
The Top Benefits of Interoperable Clinical and Claims Data
Interoperable CCD clinical data and claims data can support an effective continuous quality improvement process in healthcare, as the blended data more effectively measures quality, creates new ways of evaluating impact of interventions (near real-time and retrospective), and evaluates applied interventions with a dashboard that incorporates the best of real-time clinical and claims data. The top benefits of interoperable data can include, but are not limited to, the following:
- More refined population risk stratification and impactability analysis empowers population health programs to identify, engage, and intervene with the right person, at the right time and with key details. This improves focus on populations most in need of support and services via enhanced risk stratification.
- Enhanced care management program effectiveness improves access to clinical information to support care plan development, increases focus on people most in need of support and coaching services, and more effectively assesses barriers to care and identify options to address them.
- Improved ability to assess and get credit for delivering high-quality care and address real, versus data, care gaps reduces the amount of time to close preventive and primary care gaps, increases the team’s focus on real preventive and primary care gaps, and enables real-time assessment of opportunities to ignite new operational measurement and impact assessment of care team interventions.
- Improved access to clinical and claims data as well as other valuable data sources (e.g., social determinants of health, HL7 data such as ADT, laboratory, radiology, pathology and quality reporting document architecture [QRDA]) enhances predictive opportunities (e.g., machine learning and AI). Clinicians can identify risks and opportunities for intervention as soon as possible as well as predict behaviors and events across entire patient populations.
A Better Data Asset Means More Opportunity to Generate Better Outcomes
Organizations that wait for FHIR, and do not find an interim interoperability solution for acquiring cross-community CCDs, risk missing out on opportunities to enhance their overall data asset. The ability to provide different methods (e.g., the Health Catalyst® Interoperability Suite) to acquire cross-community CCDs and clinical data is critical to support care delivery (operationally and clinically), boost confidence around population health, and enable more accurate performance measurement.
Additional Reading
Would you like to learn more about this topic? Here are some articles we suggest:
- Pairing HIE Data with an Analytics Platform: Four Key Improvement Categories
- Linking Clinical and Financial Data: The Key to Real Quality and Cost Outcomes
- 6 Steps for Implementing Successful Performance Improvement Initiatives in Healthcare
PowerPoint Slides
Would you like to use or share these concepts? Download the presentation highlighting the key main points.
Click Here to Download the Slides
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.


