Revenue Cycle Management: Analytic Driven Insights and Efficiencies

- Increased ability to identify financial management improvement opportunities
- Up to 99% improvement in time to access data
- 97% reduction in staff time to identify root causes
To run efficiently and use the money they earn to improve the health of a community, healthcare institutions must manage their revenue cycle well. The Healthcare Financial Management Association defines revenue cycle in healthcare as all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue.1 When such functions are managed poorly, organizations may struggle to keep up in an industry where margins are shrinking and efficiency is key. At worst, they can find themselves in the position of not having the cash on hand to operate.
Crystal Run Healthcare, one of the fastest growing multi-specialty group practices in the country, and a physician-led accountable care organization (ACO) was one of the first ACOs to participate in the Medicare Shared Savings Program (MSSP).2 As an organization, they are committed to ensuring that the dollars they earn serve their patient population and are not wasted on inefficient processes. This expanding ACO—currently composed of 325 providers in more than 20 locations with 25,000 commercial lives at risk and 10,400 attributed beneficiaries—had already adopted a successful strategy using clinical analytics for managing population health. Its leaders determined that it also needed to apply its analytics strategy to improving revenue cycle management.
Specifically, Crystal Run sought to optimally manage the time to payment on account, measured as accounts receivable (A/R) days. The organization also aimed to eliminate operational waste resulting from inefficient and ineffective processes for gathering and using data.
THE CHALLENGE: DATA-DRIVEN REVENUE CYCLE MANAGEMENT IN HEALTHCARE
To achieve its growth and population management goals, Crystal Run needed the ability to provide data to clinical and operational personnel to support informed decision-making. The organization had already implemented a late-binding enterprise data warehouse (EDW) from Health Catalyst. The organization’s leaders’ strong commitment to using analytics to inform critical decisions has nurtured a culture of data-driven improvement throughout the ACO. With the EDW, clinical and operational decision-makers have access to data from a single source of truth integrated from several disparate systems across the enterprise. They use self-service analytics applications running on the EDW platform to support timely and informed decision-making.
While the EDW platform supported Crystal Run’s efforts in population health management and risk-based contracting, the organization had not yet deployed revenue cycle management analytics on the platform. Instead, the organization relied on cobbling together reports from multiple, unrelated data sources to obtain revenue cycle information. Leaders had to request custom reports from the business intelligence (BI) department when investigating the source of variation in key financial metrics, such as A/R days, collection rates, charges, and payments. New custom reports would take five days to develop on average, and even existing reports required four days for the BI team to populate them with updated information. These inefficient processes made it difficult to make quick, well-informed decisions related to revenue cycle management.
In a data-driven environment, Crystal Run needed a solution that would provide quick access to A/R and other key financial metrics. In addition, to address any problems proactively, the organization also needed more in-depth, physician-specific metrics and access to trends on demand.
SOLUTION: ADVANCED, SELF-SERVICE REVENUE CYCLE ANALYTICS
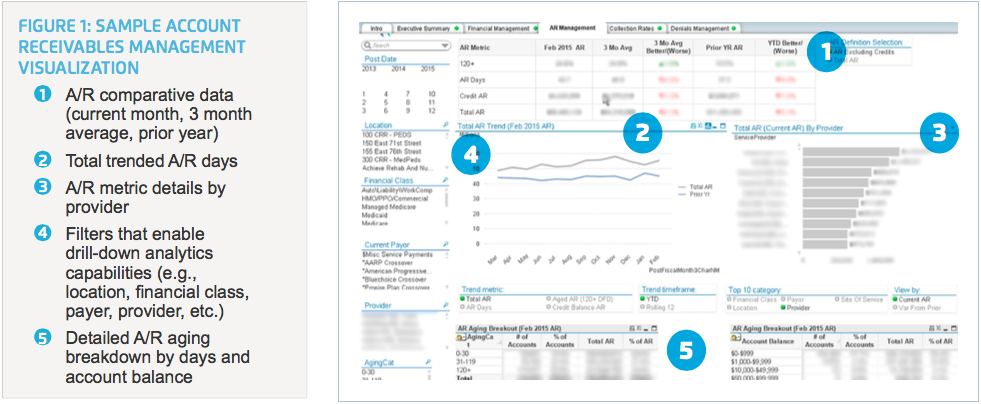
Crystal Run implemented Revenue Cycle Explorer, an advanced analytics application that runs on the EDW platform. This application provides increased data validity, access, and utility for financial information related to charges, payments, days in A/R, financial class, and collections.
The application delivers self-service analytics to finance and operations personnel so they don’t have to rely on BI for reports. Users are able to access the data quickly and have the ability to drill down to view data by provider. This in-depth insight provides a better context for decision-making and helps identify opportunities for improvement. The enhanced analysis available through Revenue Cycle Explorer also includes trending and analytics visualizations so that users can quickly interpret the data.
RESULTS
The implementation of a Revenue Cycle Explorer analytics application represents another step in Crystal Run’s evolution to a data-driven culture. Though still in its early stages, the results of this step are already significant:
Increased ability to identify financial management improvement opportunities
With the new analytics application, Crystal Run is able to quickly identify opportunities for improvement in policies, reporting, and workflow both on the executive level and in the trenches. The analytics inform the executive team at their weekly financial meetings. And the revenue cycle team has immediate access to data and trending analyses—making it easier to identify variances in the data and to investigate root cause before taking action to correct problems.
The ability to identify weak points in its revenue cycle processes has prompted Crystal Run to come up with new solutions for process improvement. One such solution resulted from an identified problem with self-pay collections. The organization designed a new process that introduces electronic tablets into physician offices. Using the tablets, patients can quickly view their co-pay and any open charges. They can then make a payment or set up a budget plan based on their needs. Crystal Run expects this new process to have an immediate impact on A/R days for self-pay accounts and to help the organization achieve its goal of no more than 5 percent of self-pay A/Rs beyond 90 days.
Up to 99% improvement in time to access data
Finance department personnel can now look at charges per month per provider on demand, a process that takes approximately four minutes. Finance used to have to wait four days to get this information in report format from BI. Furthermore, in the past, when reports came back from BI, finance did not have the ability to drill down to look for additional information—which frequently created the need for another report request and another delay. The new analytics application has eliminated that issue. In fact, for the most recent Joint Commission accreditation visit, the data was so readily available, there was no need to ask BI for any reports. The team estimates that the application provides in a single visualization what would have required a minimum of 20 reports from BI in the past. As for BI, the application is saving that department a lot of time as well. In the past, some reports would take five hours or more to build, and up to five days to deliver. Now, BI can pull the data they need from the EDW in five minutes or less.
97% reduction in staff time to identify root causes
The revenue cycle team is now able to investigate variances, unusual increases in A/R days, or other performance metrics without requesting reports from BI. Whereas researching an issue used to take the team eight or nine hours, they can now perform this analysis in 15 minutes. This represents a 97% reduction in the time required to research variances and identify root cause. Since the team researches approximately a dozen such issues per month, the cumulative time savings is significant. This time savings creates capacity to perform deeper analysis and further improve the outcomes of the department.
“Becoming a data-driven organization is an evolution, not a single event. We started out using analytics to drive improvement in certain clinical and operational areas. Now we’re tackling revenue cycle. We are moving toward access to data in multiple analytics applications that help us as an organization make faster, more data-driven decisions.”
– Lou Cervone, Director of Business Intelligence
WHAT’S NEXT
Crystal Run is still in the early stages of realizing the benefits of using the EDW to streamline revenue cycle management. To further improve the revenue cycle, the team is working to add denials and charity care data to the system—which requires improving the quality of these data streams so the information can serve as a trusted portion of the organization’s single source of truth. With the incorporation of denials and charity data into the EDW, the team will also fully deploy the Executive Dashboard, to which they will continue to add metrics over time.
Up to this point, use of the application has been limited to a key financial team while Crystal Run works to improve data integrity in order to further develop monitoring and trending functionality. The organization will soon deploy Revenue Cycle Explorer more widely to enable system-wide analytics. This broad rollout will increase Crystal Run’s use of data to drive process improvement in areas like operational efficiency, A/R days, collection rates, and denials.
References
- Healthcare Financial Management Association. (2013). Tool: Sample revenue cycle governance council charter.
- Centers for Medicare and Medicaid Services (2015). Shared Savings Program.
ABOUT HEALTH CATALYST
Health Catalyst is a mission-driven data warehousing and analytics company that helps healthcare organizations of all sizes perform the clinical, financial, and operational reporting and analysis needed for population health and accountable care. Our proven enterprise data warehouse (EDW) and analytics platform helps improve quality, add efficiency and lower costs in support of more than 50 million patients for organizations ranging from the largest US health system to forward-thinking physician practices.
For more information, visit healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.