Analytics-Driven Clinical Documentation Improvement Efforts Positively Impact Reimbursement

- 50 percent relative improvement in appropriate coding, as demonstrated in the reduction in the potential opportunity in the emergency department (ED).
- 10.8 percent relative improvement in DRG group captured for ED visits.
Albany Med’s clinical documentation improvement specialists provide high-quality care to complex, acute-care patients; however, Albany Med was experiencing lower reimbursement rates due to gaps in clinical documentation. The organization created a seamless process for clinical documentation with the use of an analytics application as driven by clinical leadership.
CLINICAL DOCUMENTATION KEY TO ACCURATE REIMBURSEMENT
Substantial volumes of clinical data obtained through documentation and contained within the medical record drive healthcare reimbursement. Over 90 percent of healthcare organizations that implement useful clinical documentation improvement (CDI) activities have realized over $2.1 million in appropriate revenue and proper reimbursements.1
Albany Med is northeastern New York’s only academic health sciences center and is one of the largest private employers in the Capital Region. The 734-bed Albany Medical Center Hospital and the Albany Medical College provide the community with the highest level of patient care across disciplines while receiving regional, national, and international recognition for high standards in patient care, education, and biomedical research.
GAPS IN REPORTING PROVE NEED FOR CLINICAL DOCUMENTATION IMPROVEMENT
Albany Med employs CDI specialists with a clinical background and specialized training in every inpatient unit. The CDI specialist function is to review the patient’s chart and request clarifications when documentation is ambiguous and/or contradictory.
Data needed by the CDI specialist were contained in different source systems, requiring many days of manual labor, gathering and consolidating the information necessary to perform chart reviews to ensure accurate coding and reimbursement.
The clinicians at Albany Med provide excellent care for the most acute and complex patients in the region; however, sometimes gaps in the documentation of the clinical care provided would negatively impact case mix index (CMI) and reimbursement rates.
Delays in chart review inhibited the ability of the CDI specialist to inform clinicians of documentation gaps promptly. Albany Med desired an analytics solution to streamline CDI processes and provide timely ongoing feedback to clinicians regarding documentation gaps.
ANALYTIC INSIGHTS, COLLABORATION LEAD TO PROCESS IMPROVEMENT
As a data-driven organization, Albany Med leveraged the Health Catalyst® Data Operating System (DOS™) and a robust suite of analytics applications. The data and analytics platform extracts data from multiple source systems and gathers them into an easily consumable visualization. Leveraging data within the analytics platform, Albany Med implemented a clinical documentation analytics accelerator to gain insight into the data it needed to ensure accurate coding and reimbursement.
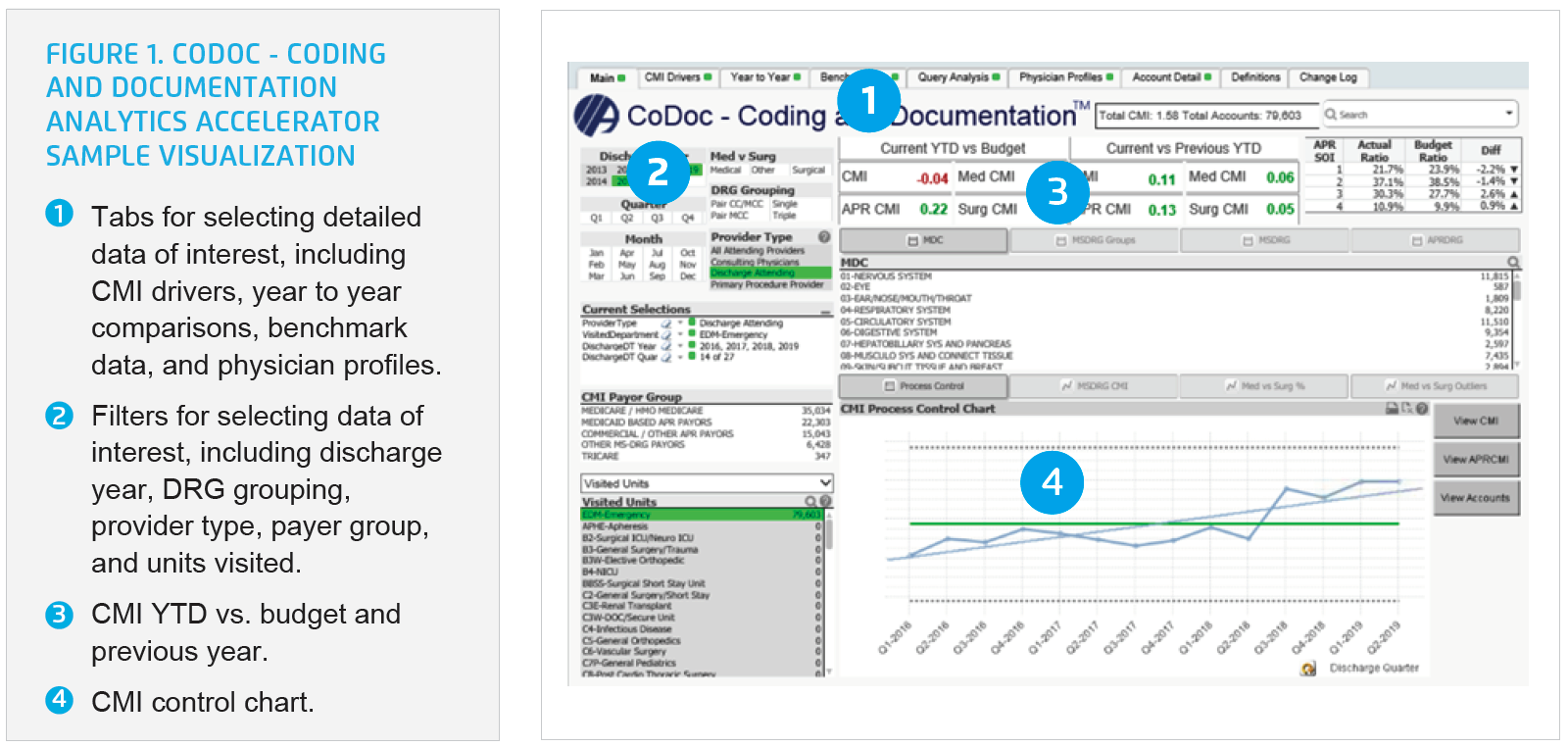
The analytics application combines financial data, MS-DRG, APRDRG, CMI, capture rates, the severity of illness, major diagnostic categories, mortality rates, and case volumes into one visualization. The CDI specialists now have near real-time access to review CDI operational metrics; they are able to view differences in documentation behaviors between physicians, conduct trend analysis, make national benchmark comparisons, and understand variances in documentation (see Figure 1).
The analytics application helped Albany Med identify $12.7 million in potential opportunity flowing through the ED. Armed with new analytics insight, the CDI team offered education and mentorship to the ED clinicians to help them better understand the importance and value of clinical documentation for coding. They also provided coaching and support that enabled the physicians to improve the accuracy and specificity of their clinical documentation.
The CDI specialists use the analytics application for review of individual clinician performance and provides specific feedback, ensuring clinical documentation is high quality and corresponds to the care the clinician delivered, including assigning the diagnosis for the treatment provided. Clinicians have access to the analytics accelerator, enabling a self-review of individual quality scores and engagement in CDI activities.
Albany Med used the benchmarking information to make comparisons with other organizations, leading to increased awareness driving improved performance. Accurate coding translated to improved revenue capture for the organization, enabling reinvestment to further its patient-centric mission.
RESULTS
Using this collaborative analytics solution to bridge the gap between clinical excellence and expertise with the documentation needed to reflect the care provided, Albany Med achieved substantial improvements, including the following:
- 50 percent relative improvement in appropriate coding as demonstrated in the reduction in the potential opportunity in the ED.
- Five percent relative increase in CMI value for ED visits.
- 10.8 percent relative improvement in DRG group captured for ED visits.
“Using this solution, we are able to use data and visualizations to help physicians improve their documentation. In addition, our doctors can now see the direct effects of the patterned changes they make through resultant coding changes over time.”
– Ashley Telisky, MD, Associate Medical Director, Director of Clinical Documentation Improvement, Albany Med
WHAT’S NEXT
Albany Med intends to continuously engage with clinicians for ongoing education and share specific opportunities as they arise to drive further documentation improvement opportunities. Albany Med’s correctly coded data will lead to an increase in provider quality scores and patient safety scores, improved relevance in documented patient conditions and clinical activities, and more accurate professional and facility reimbursement. Through these activities, providers become more aware of the importance and value of clinical documentation for coding, which translates to improved revenue capture for the organization that can be reinvested into its patient-centered and academic missions.
REFERENCES
- Gooch, K. (2018). Clinical documentation improvement a top priority for hospitals, survey finds. Becker’s Healthcare – Hospital CFO Report.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.