Using Data to Spotlight Variation and Transform Total Joint Care

- 76.5 percent relative reduction in complication rate for total hip and total knee replacement.
- 38.5 percent relative reduction in LOS for patients with total hip replacements.
- 23.3 percent relative reduction in LOS for patients with total knee replacement.
- $815,103 cost savings, achieved in less than two years.
Total Hip (THA) and Total Knee (TKA) Arthroplasty are the most prevalent surgeries for Medicare patients, numbering over 400,000 cases in 2014, costing more than seven billion dollars annually for the hospitalization alone. Today, more than seven million Americans have hip or knee implants, and the number is rising. Furthermore, substantial variation in the cost per case has raised questions about the quality of care. At Thibodaux Regional Medical Center, total joint replacement for hips and knees emerged as one of the top two cost-driving clinical areas with variation in care processes.
To address this, Thibodaux Regional maintained its focus on the IHI Triple Aim while developing organizational and clinical strategies to transform the care of patients undergoing THA and TKA. It commissioned a Care Transformation Orthopedic Team that set multiple outcome goals. Among its many efforts, the team established standard care processes, created an educational program, redesigned order sets and workflows, and deployed a joint replacement analytics application.
Thibodaux Regional reduced variability and decreased costs significantly while maintaining high levels of patient satisfaction.
THE HIGH COSTS OF TOTAL JOINT REPLACEMENT
Hip and knee replacement are among the most common inpatient surgeries for Medicare beneficiaries. In 2014, there were more than 400,000 surgeries, costing several billions of dollars annually for the hospitalization. The number of THA and TKA operations performed each year have been on the rise, a trend that is expected to continue. It is estimated that more than seven million Americans now live with an artificial hip or knee.1
There is also substantial variation in the cost of total joint replacement, with the average Medicare expenditure ranging from $16,500 to $33,000.2 As such, expenditures and associated quality outcomes are often under scrutiny.
Thibodaux Regional, a community hospital, experienced these same variation issues at a local level. As a recipient of the Healthgrades Patient Safety Excellence Award and the J.D. Power and Associates Distinguished Hospital Award, Thibodaux Regional has been committed to providing high-quality care, including its comprehensive orthopedic services.
VARIATION IN CARE INCREASES COSTS AND DECREASES QUALITY
Thibodaux Regional has diligently focused on the IHI Triple Aim: improving the quality of care, reducing the cost of providing care, and creating a great patient experience. To help achieve this, it had previously implemented the Health Catalyst® Analytics Platform, including the Late-Binding™ Data Warehouse and a broad suite of analytics applications, including the Key Process Analysis (KPA) application.
Using the analytics platform and KPA application, Thibodaux Regional examined all of its hospital care processes and determined where the greatest resource consumption and variation existed. Total joint replacement for hips and knees emerged as one of the top two cost-driving clinical areas with variation in care processes.
Upon further analysis, Thibodaux Regional identified sizeable variation in LOS, cost of care, and complication rates.
- Not all patients were medically cleared for surgery prior to their procedures, which periodically caused delays or postponements on the day of surgery. Not only were these delays costly, they also frustrated patients and their families.
- There were no clearly defined or consistent pre-op or intra-op processes, which led to provider-specific variations in care and decreased efficiency.
- Patient understanding of the pre- and postoperative expectations and care processes varied, which negatively impacted some patients’ ability to effectively participate in their care.
Thibodaux Regional needed a plan that would transform orthopedic care for its patients undergoing THA and TKA. It needed to establish consistent care processes, drive out variability, and decrease costs while improving the quality of care and patient satisfaction.
A DEDICATED TEAM TRANSFORMED ORTHOPEDIC CARE
From previous improvement efforts, Thibodaux Regional has experience with the effectiveness of dedicated improvement teams, which showed that when it focused on the Triple Aim, used data-driven approaches to improvement, and provided physicians with the necessary tools to lead change by engaging cross-functional teams, it could truly transform care.
Thibodaux Regional’s Care Transformation Steering Team commissioned a Care Transformation Orthopedic Team to focus on the care of THA and TKA patients. The cross-functional team included orthopedic surgeons, an anesthesiologist, an internal medicine physician, registered nurses, clinical directors, physical therapists, a pharmacist, a data architect, and an outcomes analyst.
The Care Transformation Orthopedic Team understood that clear goals provide focus, increase motivation, improve group cohesion, and are an essential requirement to guide work and facilitate measurement of success. The team first established outcome goals, including:
- Decreasing the risk-standardized complication rate by 1.2 percentage points.
- Decreasing the variable cost per case by 20 percent.
- Decreasing length of stay for total hip replacements by 1.3 days.
- Decreasing length of stay for total knee replacements by 0.4 days.
- Maintaining a patient satisfaction score in the 99th percentile for patients receiving total hip or total knee replacement.
Setting the stage for transformation
With the goals in place, the Care Transformation Orthopedic Team researched evidence-based practices across multiple disciplines and evaluated various strategies to improve patient safety, reduce complication rates, and improve patient education. The team planned how to change perioperative care, established standard processes, and discussed various strategies to ensure all patients received appropriate medical clearance prior to each procedure. The transformation included multiple, far-reaching, ongoing efforts:
- Redesigned pre-op workflow to ensure medical clearance is obtained prior to scheduling surgery and redesigned lab ordering processes to reduce inadvertent over-ordering of labs.
- Implemented a mandatory total joint replacement class for all patients undergoing elective hip and knee replacements.
- Classes focus on the patient experience, providing important information and expectation setting about pre- and postoperative activities, such as pain control, the importance of early mobility, anticipated length of stay, and the continuation of care post discharge.
- Patients are encouraged to bring a family member or significant other who will be helping them with their recovery.
- During the class, patients complete an assessment, providing valuable insight into the patients’ postoperative needs, allowing the care team to plan for how to best meet their needs prior to surgery, which, in turn, improves the efficiency of the inpatient discharge processes.
- Redesigned pre- and postoperative order sets, eliminating unnecessary or redundant orders and ensuring up-to-date, clearly defined, standard practices for patients undergoing hip and knee replacements.
- Revised order sets, provided physician education regarding current evidence-based transfusion practices, and implemented new requirements for physician authorization prior to transfusion, all to ensure appropriate blood products utilization.
- Redesigned the intraoperative workflow, moving away from general anesthesia, instead using spinal and epidural anesthesia. The team also standardized the supplies used for total joints, discontinuing the use of supplies that did not add value or improve patient outcomes.
- Changed available surgery times in the operating room, with all elective hip and knee surgeries occurring on Mondays and Tuesdays with overflow into Wednesday. This helps ensure these surgeries have a consistent, dedicated OR crew, assisting the surgeon to be as efficient as possible. Patients can participate in early mobilization and activities designed to ensure safe discharge prior to the weekend.
- Focused on improving early mobility postoperatively, promptly discontinuing indwelling urinary catheters after surgery, getting patients out of bed the day of surgery, and using multi-modal pain management to decrease the use of opioids.
Data and analytics illuminate the issues
The Care Transformation Orthopedic Team used the Health Catalyst Joint Replacement – Hip and Knee improvement application to monitor performance and the outcomes associated with its improvement work (see Figure 1).
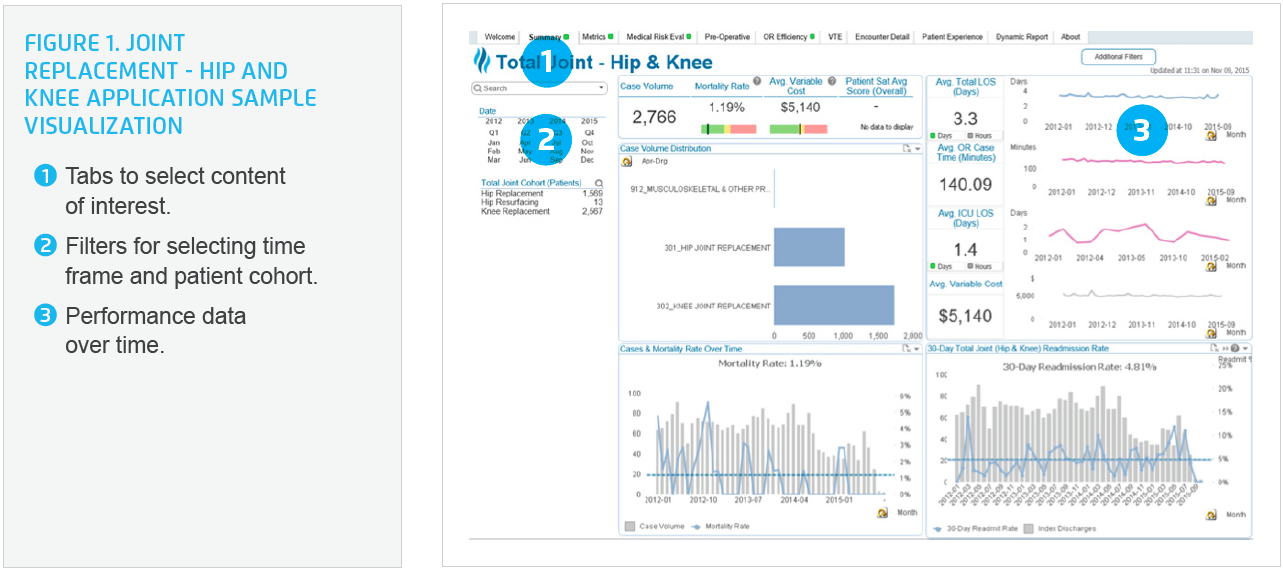
The analytics application provided near real-time data, giving the team valuable insight into complication rates, average variable cost, length of stay, compliance with the newly defined pre- and postoperative processes, and patient satisfaction. The team could immediately see the impact of their work on outcomes, which increased stakeholder commitment and willingness to change.
RESULTS
Thibodaux Regional successfully transformed the care processes and outcomes for patients undergoing hip and/or knee joint replacement. Results include:
- 76.5 percent relative reduction in complication rate for total hip and total knee replacement.
- 38.5 percent relative reduction in LOS for patients with total hip replacements.
- 23.3 percent relative reduction in LOS for patients with total knee replacement.
- Improved patient education, early mobilization, and decreased use of opioids have contributed to a shortened LOS.
- $815,103 cost savings, achieved in less than two years.
- All changes accomplished while maintaining high levels of patient satisfaction.
“Data transparency helped make the case for change with the physicians. When we were able to see our individual performance in comparison to our peers, it motivated us to want to do better.”
– Dr. David Elias, MD
Orthopaedic Surgery
WHAT’S NEXT
Thibodaux Regional plans to continue its focus on the Triple Aim, using data-driven approaches to transform care. The Care Transformation Orthopedic Team is exploring opportunities to further decrease the costs within the operating room.
REFERENCES
- American Academy of Orthopaedic Surgeons. (2014). 2.5 million Americans living with an artificial hip, 4.7 million with and artificial knee.
- Centers for Medicare & Medicaid Services. (2015). Comprehensive care for joint replacement (CJR) model.
ABOUT HEALTH CATALYST
Health Catalyst is a next-generation data, analytics, and decision support company committed to being a catalyst for massive, sustained improvements in healthcare outcomes. We are the leaders in a new era of advanced predictive analytics for population health and value-based care. With a suite of machine learning-driven solutions, decades of outcomes-improvement expertise, and an unparalleled ability to integrate data from across the healthcare ecosystem. Our proven data warehousing and analytics platform helps improve quality, add efficiency and lower costs in support of more than 85 million patients and growing, ranging from the largest US health system to forward-thinking physician practices. Our technology and professional services can help you keep patients engaged and healthy in their homes and workplaces, and we can help you optimize care delivery to those patients when it becomes necessary. We are grateful to be recognized by Fortune, Gallup, Glassdoor, Modern Healthcare and a host of others as a Best Place to Work in technology and healthcare.
Visit www.healthcatalyst.com, and follow us on Twitter, LinkedIn, and Facebook.
This website stores data such as cookies to enable essential site functionality, as well as marketing, personalization, and analytics. By remaining on this website you indicate your consent. For more information please visit our Privacy Policy.